Copyright
©The Author(s) 2017.
World J Cardiol. Jul 26, 2017; 9(7): 574-582
Published online Jul 26, 2017. doi: 10.4330/wjc.v9.i7.574
Published online Jul 26, 2017. doi: 10.4330/wjc.v9.i7.574
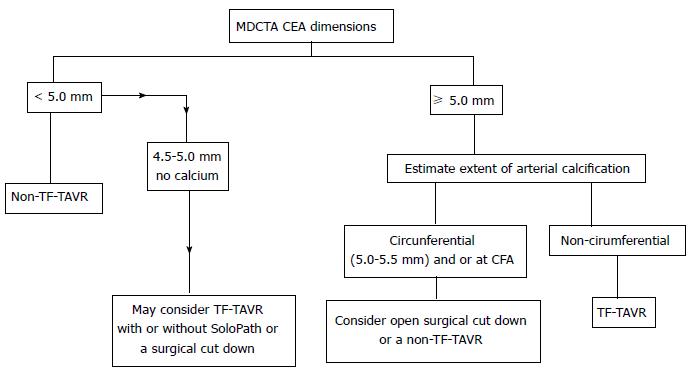
Figure 1 Schematic representation of trans catheter aortic valve replacement access approach based on common femoral artery dimensions as seen on multidetector computed tomography angiography.
TAVR: Transcatheter aortic valve replacement; CFA: Common femoral artery; MDCTA: Multidetector computed tomography angiography. Republished with permission of Sage from Sardar et al[39].
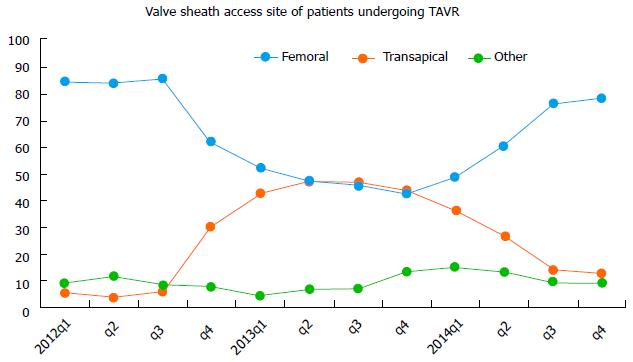
Figure 2 Transcatheter aortic valve replacement vascular access site in the transcatheter valve therapy Registry, 2012 to 2014.
The changing valve sheath access site over time has resulted from multiple factors, including FDA instructions for use, and changing technology. TAVR: Transcatheter aortic valve replacement. Republished with permission of Elsevier, from Holmes DR, Nishimura RA, Holmes et al[4].
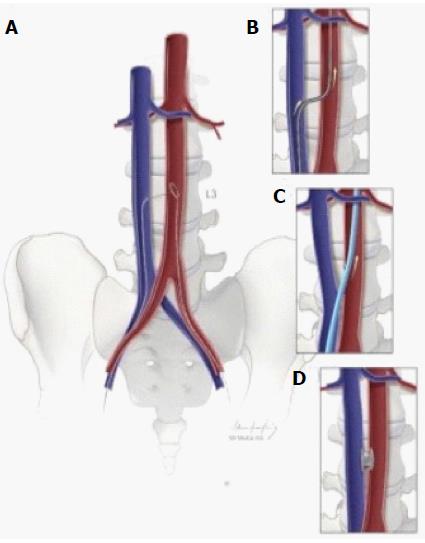
Figure 3 Schematic depiction of caval-aortic access.
A: Using transfemoral venous access, a catheter directs a guidewire from the inferior vena cava toward a snare positioned in the adjacent abdominal aorta; B: The catheter is advanced over the guidewire into the aorta and used to introduce a more rigid guidewire; C: The valve introducer sheath is advanced from the vena cava into the aorta; D: After completion of transcatheter aortic valve replacement, the aorto-caval access tract is closed with a nitinol occluder. Republished with permission of Elsevier from A.B Greenbaum, J Am Coll Cardiol 2014; 63: 2795-2804.
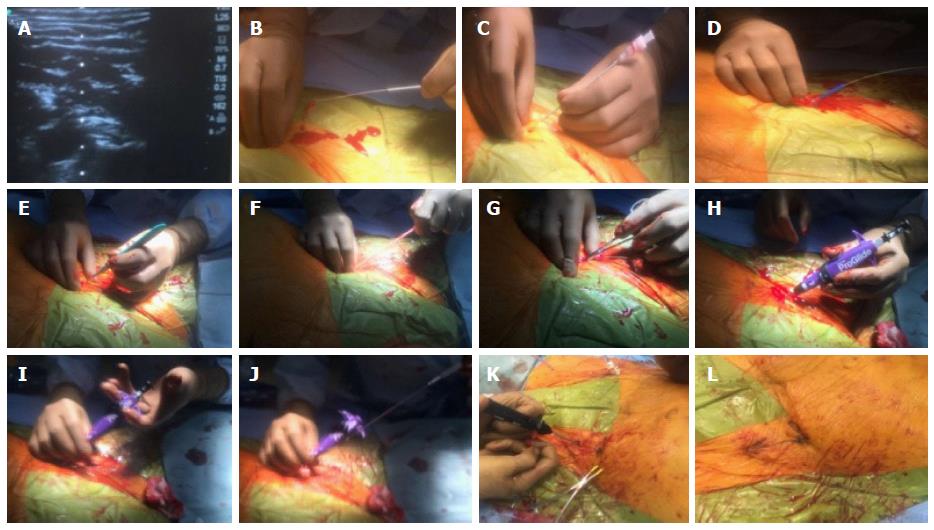
Figure 4 Pre-close hemostasis technique during a transcatheter aortic valve replacement procedure.
A-C: A calcium-free zone is visualized using real time ultrasound and access is obtained using a micropuncture needle system; D-G: The micropuncture system is exchanged for a 180 cm 0.035 wire and the skin tract is sequentially dilated with scalpel, 7 F sheath dilator and later a forceps; H: A Proglide is advanced over the wire into the arterial lumen, and return of pulsatile blood flow confirmed; I and J: After ensuring stable Proglide position, two sequential sutures are deployed at 10 and 2 0’clock; K and L: After the removal of transcatheter aortic valve replacement sheath and guide wire, pre-close sutures are sequentially locked to ensure hemostasis.
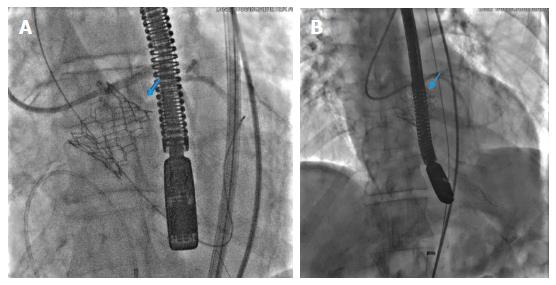
Figure 5 Annular rupture post transcatheter aortic valve deployment with the rupture site marked by blue arrows (A, B).
- Citation: Chaudhry MA, Sardar MR. Vascular complications of transcatheter aortic valve replacement: A concise literature review. World J Cardiol 2017; 9(7): 574-582
- URL: https://www.wjgnet.com/1949-8462/full/v9/i7/574.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i7.574