Copyright
©The Author(s) 2025.
World J Gastrointest Surg. Aug 27, 2025; 17(8): 108767
Published online Aug 27, 2025. doi: 10.4240/wjgs.v17.i8.108767
Published online Aug 27, 2025. doi: 10.4240/wjgs.v17.i8.108767
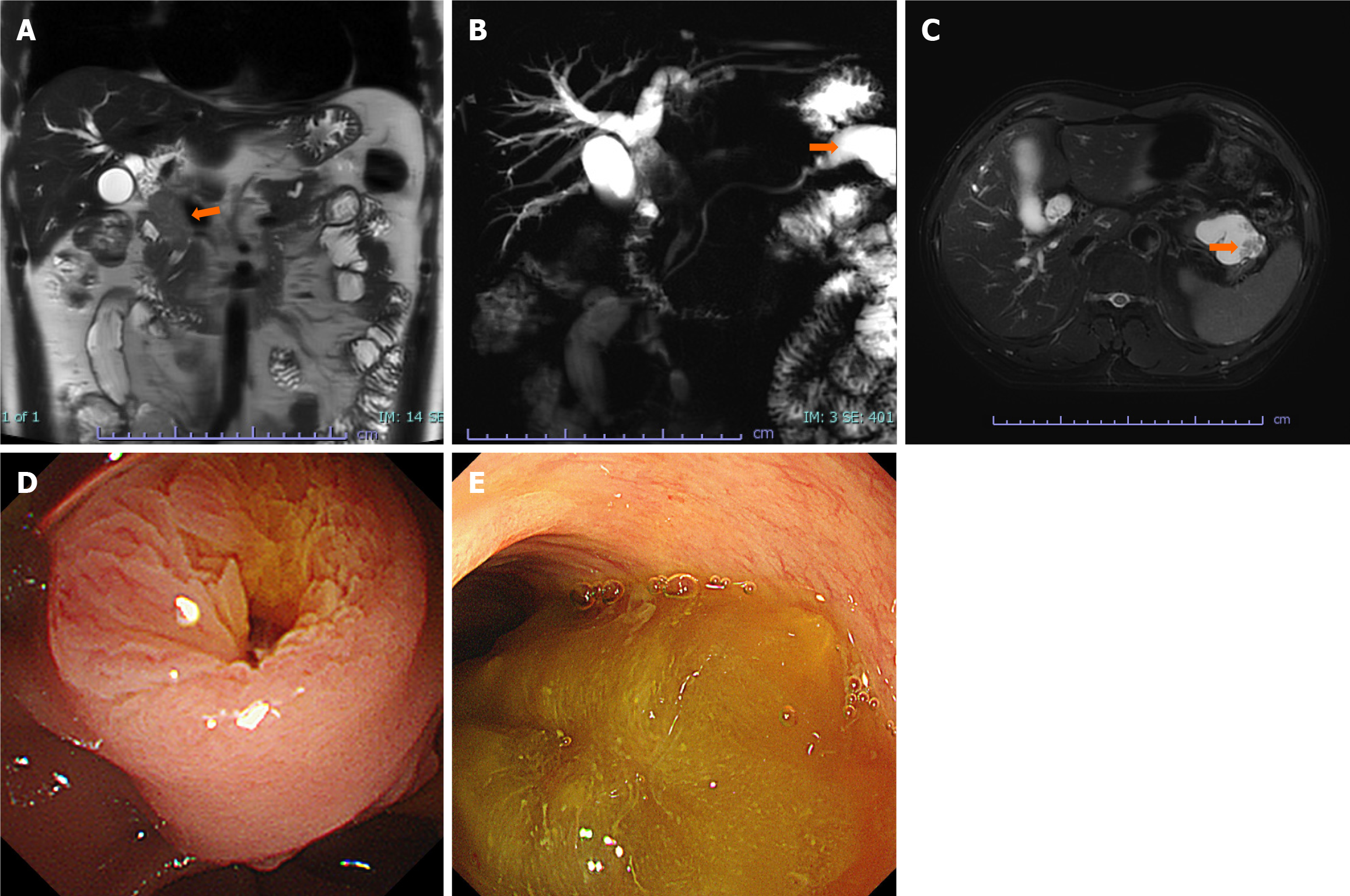
Figure 1 Abdominal magnetic resonance imaging scan and duodenoscopy findings.
A: On the coronal magnetic resonance imaging (MRI)/T2-weighted imaging (T2WI), a soft-tissue mass was seen in the middle and upper segments of the common bile duct, as indicated by the orange arrow; B: Magnetic resonance cholangiopancreatography shows a cystic lesion in the pancreatic tail continuous with the main pancreatic duct, as indicated by the orange arrow; C: The axial MRI/T2WI indicates a cystic lesion in the pancreatic tail with visible mural nodules, as indicated by the orange arrow; D and E: Duodenoscopy revealed an enlarged, fish-mouth papilla resulting from excessive mucinous secretion from the bile duct or pancreatic duct-a characteristic endoscopic sign of intraductal papillary mucinous neoplasm or intraductal papillary neoplasm of the bile duct.
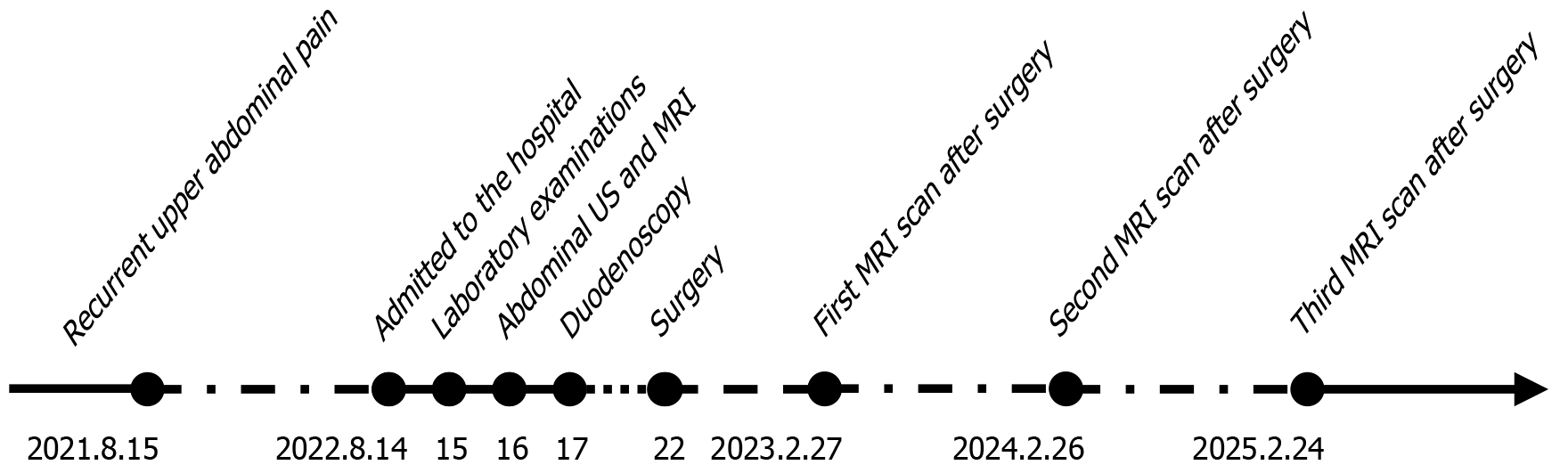
Figure 2 Timeline of the patient’s disease course, treatment, and follow-up.
US: Ultrasonography; MRI: Magnetic resonance imaging.
- Citation: Huang XR, Zhu DS, Yu YH. Surgical resection for simultaneous intraductal papillary mucinous neoplasm of the bile duct and pancreatic duct: A case report. World J Gastrointest Surg 2025; 17(8): 108767
- URL: https://www.wjgnet.com/1948-9366/full/v17/i8/108767.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i8.108767