Copyright
©The Author(s) 2017.
World J Gastrointest Oncol. Dec 15, 2017; 9(12): 475-491
Published online Dec 15, 2017. doi: 10.4251/wjgo.v9.i12.475
Published online Dec 15, 2017. doi: 10.4251/wjgo.v9.i12.475
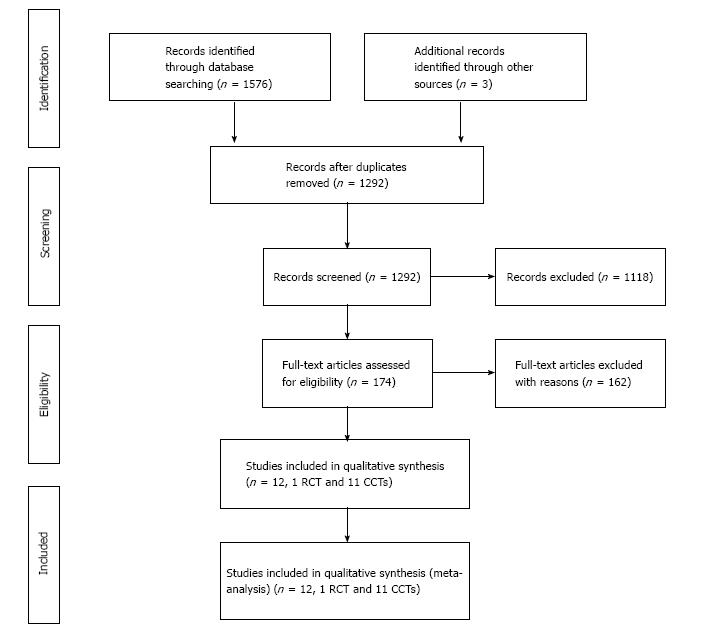
Figure 1 Flow diagram of the systematic literature search and study selection according to prisma statement.
RCT: Randomized control trial; CCT: Controlled clinical trial.
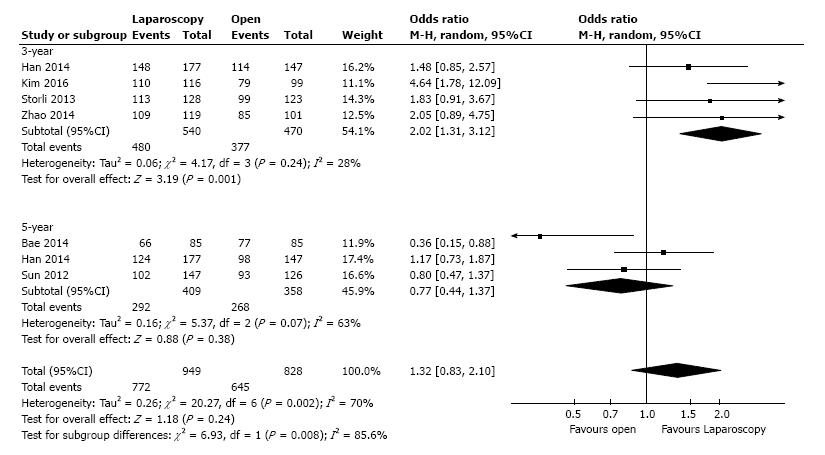
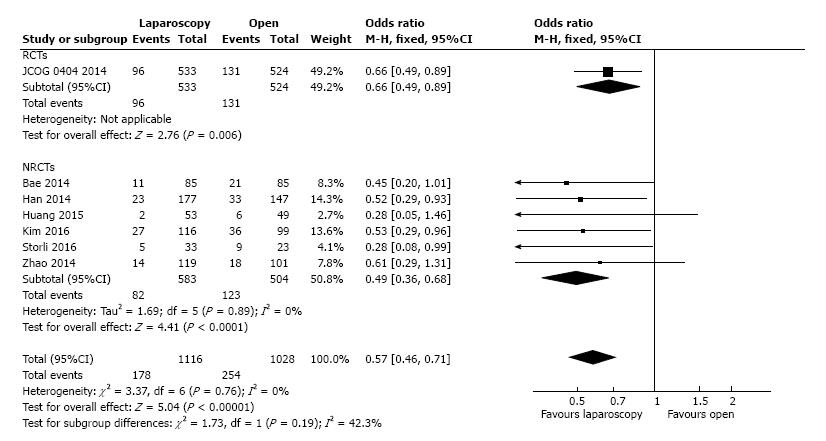
Figure 2 Meta-analysis of studies on overall survival of patients undergoing laparoscopic vs open complete mesocolic excision with central vascular ligation excision for colon cancer.
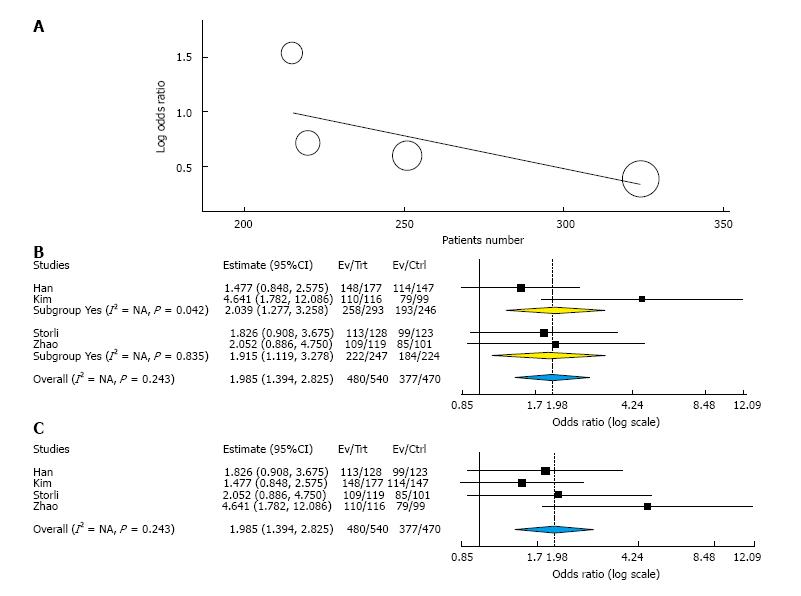
Figure 3 Results of statistical analysis.
A: Meta-regression on three-year overall survival according with the number of included patients in each study, of patients undergoing laparoscopic vs open complete mesocolic excision with central vascular ligation excision for colon cancer; B: Subgroup meta-analysis according with the selection of patients with only right colon cancers (Yes group) or all-localizations colon cancer (No group); C: Cumulative meta-analysis according to the year of publishing for each study.
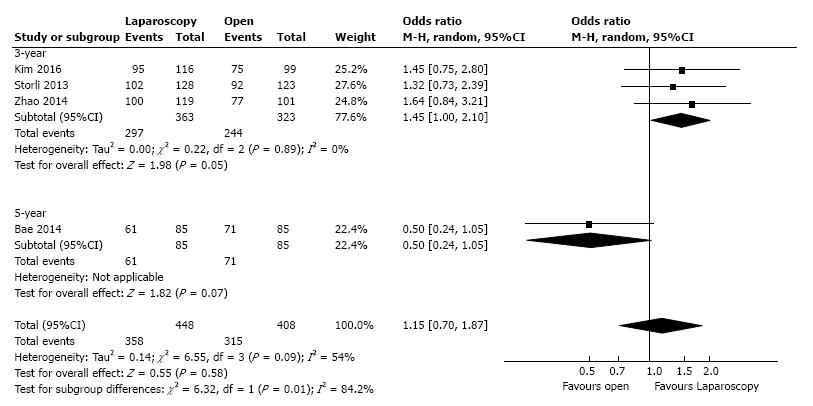
Figure 4 Meta-analysis of studies on disease-free survival of patients undergoing laparoscopic vs open complete mesocolic excision with central vascular ligation excision for colon cancer.
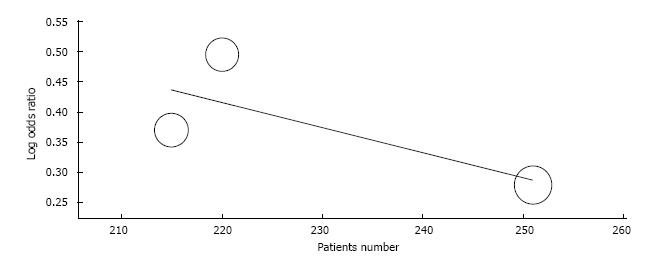
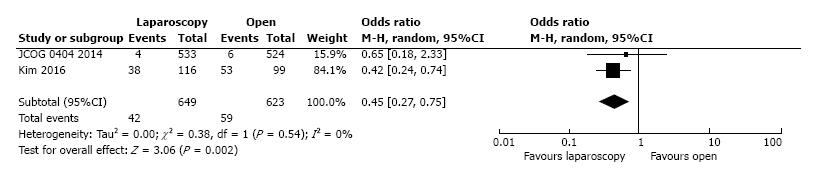
Figure 5 Meta-regression of studies on three-year disease-free survival of patients undergoing laparoscopic vs open complete mesocolic excision with central vascular ligation excision for colon cancer.
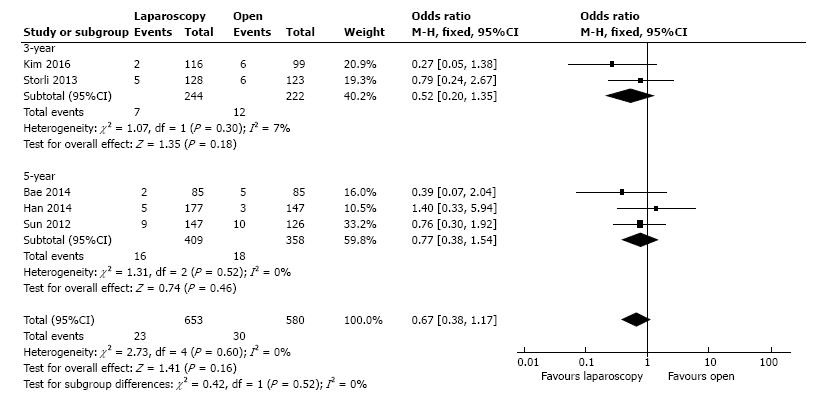
Figure 6 Meta-analysis of studies local recurrence rate of patients undergoing laparoscopic vs open complete mesocolic excision with central vascular ligation excision for colon cancer.
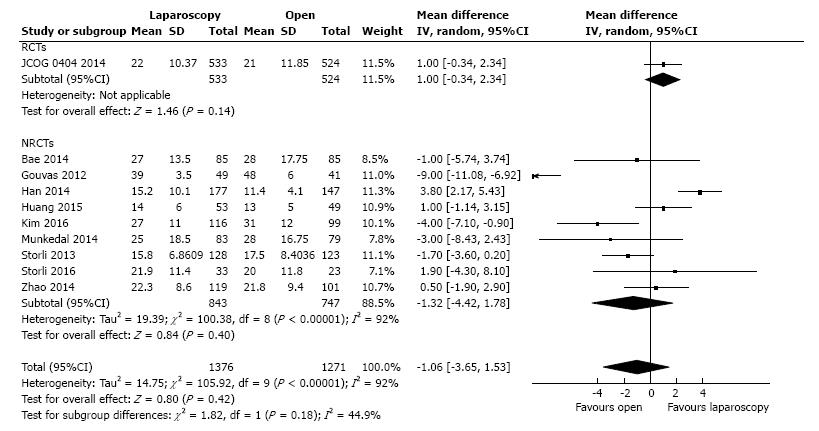
Figure 7 Meta-analysis of studies on lymphnodes retrieved of the specimen of patients undergoing laparoscopic vs open complete mesocolic excision with central vascular ligation excision for colon cancer.
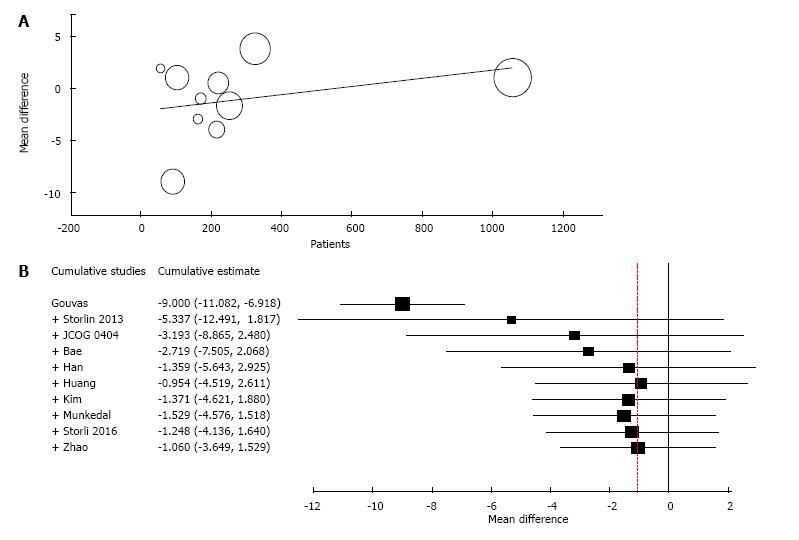
Figure 8 Results of statistical analysis.
A: Meta-regression of studies on lymphnodes retrieved of the specimen according to the number of the included patients in each study; B: Cumulative meta-analysis according to the year of publishing of the article of patients undergoing laparoscopic vs open complete mesocolic excision with central vascular ligation excision for colon cancer.
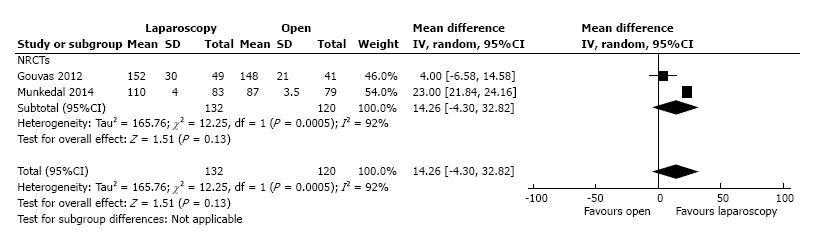
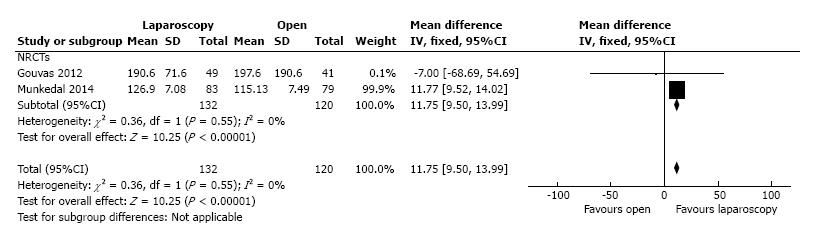
Figure 9 Meta-analysis of studies on tumor to arterial high tie (mm) distance of the specimen of patients undergoing laparoscopic vs open complete mesocolic excision with central vascular ligation excision for colon cancer.
Figure 10 Meta-analysis of studies on resected mesocolon surface (cm2) of the specimen of patients undergoing laparoscopic vs open complete mesocolic excision with central vascular ligation excision for colon cancer.
Figure 11 Meta-analysis of studies on transfusion requirements of patients undergoing laparoscopic vs open complete mesocolic excision with central vascular ligation excision for colon cancer.
Figure 12 Meta-analysis of studies on postoperative overall morbidity of patients undergoing laparoscopic vs open complete mesocolic excision with central vascular ligation excision for colon cancer.
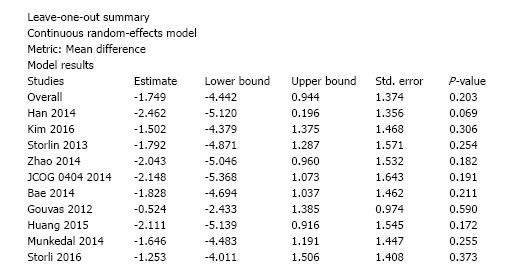
Figure 13 Leave-one-out meta-analysis for the endpoint number of retrieved lymphnodes of patients undergoing laparoscopic vs open complete mesocolic excision with central vascular ligation excision for colon cancer.
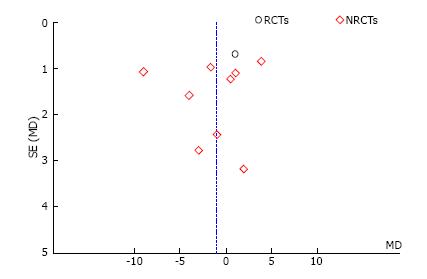
Figure 14 Begg’s funnel plot for the endpoint number of retrieved lymphnodes of patients undergoing laparoscopic vs open complete mesocolic excision with central vascular ligation excision for colon cancer.
RCTs: Randomized control trial; NRCTs: Non-randomized clinical studies.
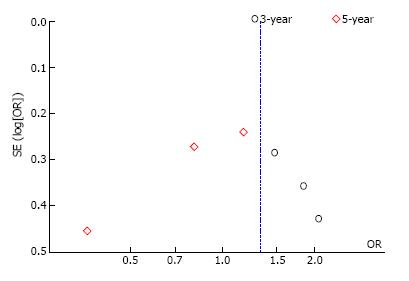
Figure 15 Begg’s funnel plot for the endpoint overall survival of patients undergoing laparoscopic vs open complete mesocolic excision with central vascular ligation excision for colon cancer.
- Citation: Negoi I, Hostiuc S, Negoi RI, Beuran M. Laparoscopic vs open complete mesocolic excision with central vascular ligation for colon cancer: A systematic review and meta-analysis. World J Gastrointest Oncol 2017; 9(12): 475-491
- URL: https://www.wjgnet.com/1948-5204/full/v9/i12/475.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v9.i12.475