Copyright
©The Author(s) 2021.
World J Gastrointest Oncol. Jun 15, 2021; 13(6): 625-637
Published online Jun 15, 2021. doi: 10.4251/wjgo.v13.i6.625
Published online Jun 15, 2021. doi: 10.4251/wjgo.v13.i6.625
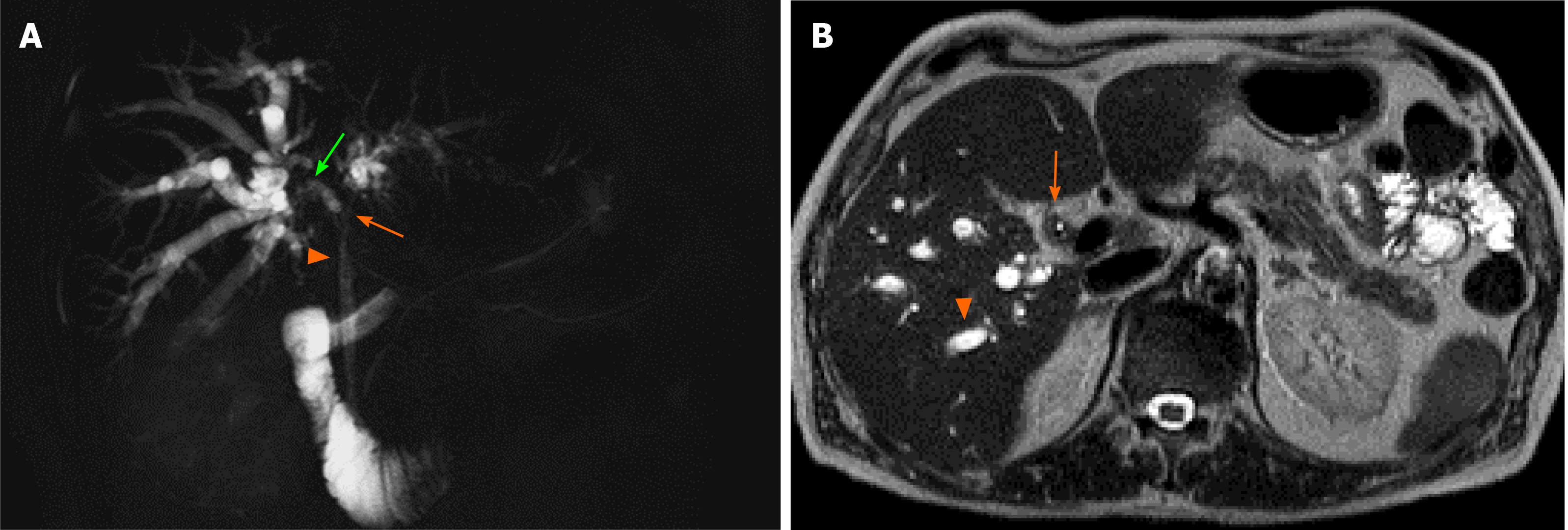
Figure 1 Patient was a 67-year-old man who was admitted to our hospital due to obstructive jaundice.
A: Cholangio-MRI showed severe and long stricture of the common (arrowhead) and both right (green arrow) and left (orange arrow) hepatic ducts and, to a lesser extent, of distal branching of both right anterior and posterior segmental duct, with secondary upstream intrahepatic bile duct dilatation; B: Axial T2-weighted magnetic resonance image showed intrahepatic biliary dilatation (arrowhead) due to a T2 isointense intraductal mass (arrow). Preoperative imaging was consistent with an extrahepatic cholangiocarcinoma of Bismuth-Corlette type IV. Endoscopic preoperative biliary drainage was performed to relieve the obstruction. After multidisciplinary discussion, extended right hepatectomy was planned. Portal vein embolization of the right liver was carried out three weeks before the operation. Then, the patient underwent right hepatectomy extended to segment I, complete extirpation of the extrahepatic biliary system, and simultaneous pancreatoduodenectomy due to tumour involvement of the distal common bile duct at intraoperative frozen section. Thus, hepatopancreatoduodenectomy was the final surgical procedure. Final pathology showed a moderately differentiated cholangiocarcinoma with mucinous component, with 14 negative lymph nodes. Postoperative course was complicated by development of transient liver failure with ascites, electrolyte imbalance, and delayed gastric emptying with nausea and vomiting. The patient was discharged in postoperative day 58 and did not undergo chemotherapy. After 12 months, the patient is doing well, in stable health condition.
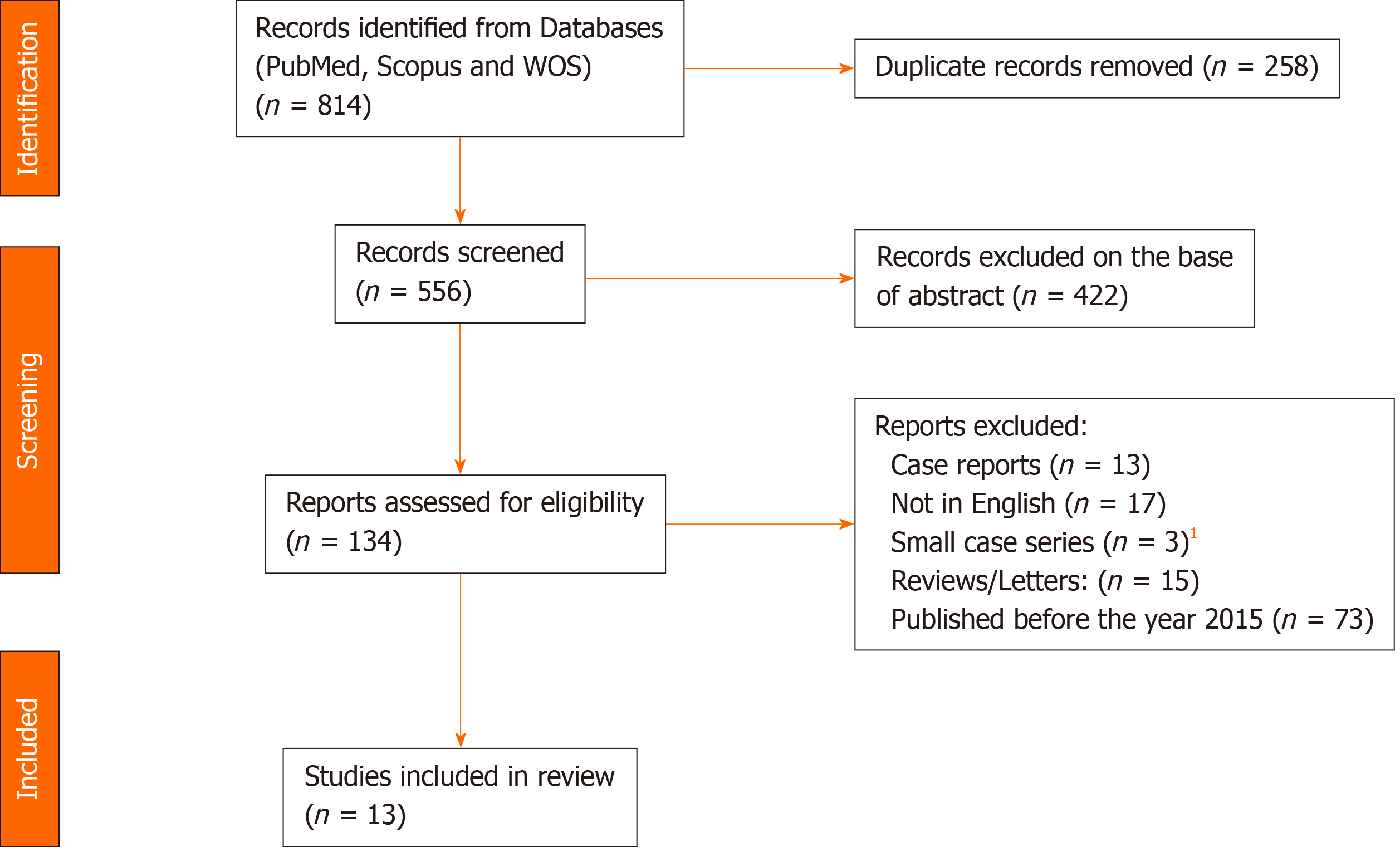
Figure 2 Flowchart of the study search and selection in this review.
1Articles not reporting on at least 10 cases of hepatopancreatoduodenectomy.
- Citation: Fancellu A, Sanna V, Deiana G, Ninniri C, Turilli D, Perra T, Porcu A. Current role of hepatopancreatoduodenectomy for the management of gallbladder cancer and extrahepatic cholangiocarcinoma: A systematic review. World J Gastrointest Oncol 2021; 13(6): 625-637
- URL: https://www.wjgnet.com/1948-5204/full/v13/i6/625.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v13.i6.625