Published online Apr 16, 2012. doi: 10.4253/wjge.v4.i4.99
Revised: February 20, 2012
Accepted: March 30, 2012
Published online: April 16, 2012
Since the first reports almost ten years ago, wireless capsule endoscopy has gained new fields of application. Colon capsule endoscopy represents a new diagnostic technology for colonic exploration. Clinical trials have shown that colon capsule endoscopy is feasible, accurate and safe in patients suffering from colonic diseases and might be a valid alternative to conventional colonoscopy in selected cases such as patients refusing conventional colonoscopy or with contraindications to colonoscopy or when colonoscopy is incomplete. Despite the enthusiasm surrounding this new technique, few clinical and randomized controlled trials are to be found in the current literature, leading to heterogeneous or controversial results. Upcoming studies are needed to prove the substantial utility of colon capsule endoscopy for colon cancer screening, especially in a low prevalence of disease population, and for other indications such as inflammatory bowel disease. Possible perspectives are critically analysed and reported in this paper.
- Citation: Riccioni ME, Urgesi R, Cianci R, Bizzotto A, Spada C, Costamagna G. Colon capsule endoscopy: Advantages, limitations and expectations. Which novelties? World J Gastrointest Endosc 2012; 4(4): 99-107
- URL: https://www.wjgnet.com/1948-5190/full/v4/i4/99.htm
- DOI: https://dx.doi.org/10.4253/wjge.v4.i4.99
After the Food and Drug Administration (FDA) approval in 2001, small bowel capsule endoscopy has rapidly gained ground in the armamentarium of small bowel investigation techniques and has quickly come up to expectations. Small bowel endoscopy has proved to be an extremely efficient tool providing high quality images of the entire small bowel which up to that time were largely inaccessible to flexible endoscopy[1]. Capsule endoscopy has dramatically changed the diagnostic approach to intestinal diseases. Technical and clinical experience gained in this field have been extended to segments of the digestive tract other than the small bowel and new capsule endoscopy applications have been implemented, such as oesophageal and colon capsule endoscopy[2,3]. Currently, conventional optical colonoscopy is considered the gold standard for colon diagnosis and therapy, carrying an overall risk of complications of 0.3% and rising to 2% when including a therapeutic procedure[4-6]. Conventional colonoscopy is an invasive procedure with some contraindications. It mostly requires conscious or deep sedation, and is thus associated with a further degree of procedural risk[7]. PillCam colon capsule endoscopy (PCCE) is a new device recently developed to investigate and provide images of the entire colon in a minimally invasive way. Despite great expectations surrounding this new technique, few available studies in the literature report controversial and conflicting results. There is still a high degree of uncertainty regarding its clinical indications.
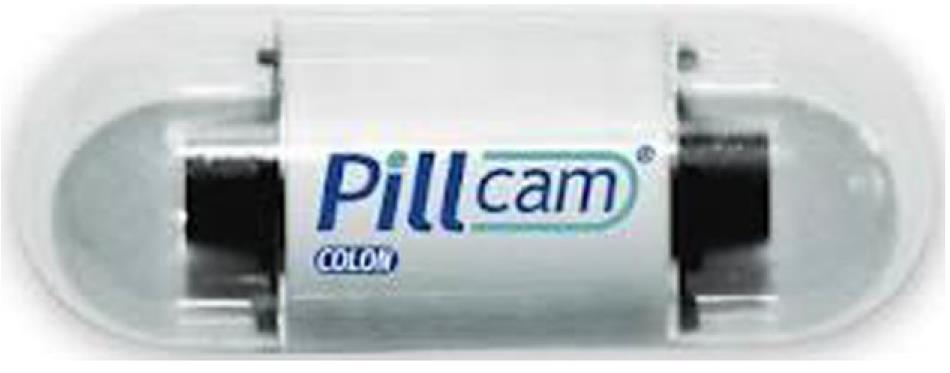
In 2006, Given Imaging Ltd. developed the first generation of capsule specifically designed for colon investigation[8,9] and represented a technical evolution of the pre-existing small bowel and oesophageal capsules. Similar to the other PillCam systems, the current system consists of an ingestible videocapsule. The PillCam colon capsule (PCC) measures 31 mm × 11 mm (Figure 1), is equipped with dual cameras and implemented optics and has a total operating time of approximately 10 h. Both imagers acquire 2 images per second, contain an advanced automatic light control and capture more than twice the coverage area and depth of field of PillCam small bowel resulting in a superior observation field. The angle of view from each imager is 156°. Other specific features are the presence of a longer battery lasting 9-10 h. Furthermore, the battery can “hibernate” minutes to hours after ingestion in order to save power before the capsule enters the colon. At the beginning of the examination, PCC turns on and transmits images for 3 min and then enters a “sleep” mode for 1 h and 45 min to save battery energy. After this time, it automatically reactivates and restarts the transmission of images of the terminal ileum, theoretically allowing complete colonic exploration. Images transmitted by PCC are stored in a dedicated portable external recorder (DR2C). After completion of the examination the recorder is connected to a workstation and loaded with a dedicated software (RAPID software) for video processing and subsequent viewing[8,9].
Recently, a second-generation colon capsule has been developed to increase sensitivity for detection of colonic findings and to simplify the procedure[10]. The new PCC-2 is slightly bigger measuring 11.6 mm × 31.5 mm. The angle of view from both the imagers has been widened to 172 degrees, allowing for nearly 360° coverage of the colon. In order to further enhance the colon coverage, to adequately image the mucosa when the capsule is accelerated by peristalsis, to economise on battery energy and optimize the video length, the capsule is equipped with an adaptable image acquisition rate depending on the speed of progression of the capsule along the colon. PCC-2 captures 35 frames per second while it is moving and 4 frames per second when it is virtually stationary. To further save battery energy and to allow automatic identification of the small bowel, PCC-2, instead of entering a “sleep” mode, continues to work at a low rate of 14 images per minute until small bowel images are detected. The capsule then turns into the adaptive frame rate mode. The new data recorder (DR3) also assists and guides the medical staff and the patient through the procedure. In fact, it buzzes and vibrates and displays instructions on its liquid crystal diode screen to alert the patient to continue the preparation according to the protocol. The new RAPID software embeds additional diagnostic features for video processing and viewing such as a flexible spectral imaging colour enhancement (FICE) technology to allow a more detailed analysis of the mucosal surface and better detection of flat lesions and has a polyp size estimation tool. The clinical value of these features deserves further assessment and validation.
The video evaluation process should include three steps: (1) preview; (2) review; and (3) report. During the “preview step”, it is advisable to run and preview the entire video with simultaneous viewing from both heads and capture all the main anatomical landmarks (first caecal image, last anal image, hepatic flexure and splenic flexure). During this initial evaluation, high viewing speed (30-40 frames per second) may be selected. The “review step” consists of a careful examination of the video from the first caecal image to the last colonic image using the single head mode, followed by examination of the colon using the other head side, as lesions could be detected by only one of the two optics[11]. During this detailed review it is advisable to select a slow speed viewing mode. All encountered findings should be captured during this step. In the “report step”, once the video review is finished, all captured findings should be reviewed and described in terms of nature, size and location. Diverticulosis and other collateral findings should also be reported.
The technical performance of the PCC-1 was good, but that of the PCC-2 seems close to perfect.
Colorectal cancer (CRC) is the third most common type of cancer with a cumulative lifetime risk of approximately 5%, and is the second leading cause of cancer-related death in Western countries. One of three patients suffering from CRC will present with advanced disease at the time of diagnosis and will not survive[12]. Despite this, CRC can be considered a preventable condition. CRC mostly arises from adenomatous polyps as a result of their progression to invasive adenocarcinoma over many years. Colonic adenomas are found in 11% to 40% of the population with average risk[13-15]. Furthermore CRC can be considered a curable condition. In fact, the 5-year survival rate in early stages can reach 90%[12]. For these reasons, conventional colonoscopy is suggested as the optimal technique to be used for CRC screening programs in high-risk populations. However, it has to be considered that compliance rates in screening programs do not rank above 25%[16]. Low compliance can be explained by the drawbacks of conventional colonoscopy, such as being painful, patient’s discomfort or embarrassment and/or the need for sedation.
Non-invasive techniques for colonoscopy, such as CT colonography[17,18] and colon capsule endoscopy[19-20] are currently being evaluated as alternatives to conventional colonoscopy in order to improve compliance to screening programs. The long-term primary objective of the PCC is the average risk population undergoing CRC screening. All currently available studies are based on disease enriched populations mainly consisting of symptomatic patients. No studies have been performed to date in the setting of a low prevalence of disease.
Five studies based on the first generation of colon capsule, overall including 602 patients, and two studies on the second generation capsule, respectively enrolling 104 and 117 patients, have been published[8-10,21-24]. Two feasibility studies initially addressed whether PCCE was technically successful in human subjects, also provided preliminary accuracy estimates[8,9].
In the first Israeli multicentre study[8], PCCE was able to visualize the entire colon in 80% of cases. The level of bowel preparation was quite high, being rated as good-excellent in 84% of the cases. Accuracy values were estimated according to three reading levels, depending on the reader’s expertise. When assessing the least experienced (the centre investigator), PCCE sensitivity was disappointing, being respectively 56% for polyps of any size and 50% for significant findings (defined as one polyp ≥ 6 mm or more than 3 polyps), with specificity being 69% and 83%. On the other hand, when the same cases were re-evaluated by an expert panel, accuracy values substantially increased, suggesting that dedicated training may be needed before implementing this technique. We might speculate that PCCE, similar to colonoscopy, could be operator-dependant. In the second study[9], complete visualization of the whole colon was reached in 83% of cases, and 89% of the patients showed a good-excellent bowel preparation. PCCE sensitivity for both polyps of any size and significant findings was promising being 76% and 77%, respectively (substantially higher than that reported by Eliakim et al[10]). On the other hand, specificity was still low, being 64% and 70% for polyps of any size and significant findings, respectively.
The first European multicentre study[21], a head-to-head technical comparison between PCCE and colonoscopy, involved 328 subjects enrolled in eight centres. Similar to the feasibility studies, PCCE appeared to be technically successful in 320 patients, only 12 (4%) being excluded from the final analysis because of technical failure. PCCE sensitivity for polyps of any size, ≥ 6 mm and ≥ 10 mm were 72%, 64%, and 60%, respectively, while specificity values for polyps of any size, ≥ 6 mm and ≥ 10 mm were 78%, 84% and 98%, respectively (Table 1). A sufficiently high number of cancers were identified at colonoscopy in this study. PCCE was able to diagnose 14 of 19 carcinomas diagnosed at colonoscopy, corresponding to a sensitivity of 76%. Such false-negatives were mainly induced by a fair-poor bowel preparation or incomplete examination.
| n | S (%) | E (%) | PPV (%) | NPV (%) | |
| Results for polyps (any size) | |||||
| Eliakim et al[8] 2006 | 91 | 69 | 81 | 74 | 78 |
| Schoofs et al[9] 2006 | 41 | 76 | 64 | 83 | 54 |
| Van Gossum et al[21] 2009 | 320 | 72 | 78 | - | - |
| Eliakim et al[10] 20091 | 98 | 88 | - | - | - |
| Results for significant polyps (≥ 6 mm or > 3 polyps > 3 mm) | |||||
| Eliakim et al[8] 2006 | 91 | 63 | 94 | 67 | 91 |
| Schoofs et al[9] 2006 | 41 | 60 | 73 | 46 | 83 |
| Van Gossum et al[21] 2009 | 320 | 64 | 84 | - | - |
| Eliakim et al[10] 20091 | 98 | 89 | 76 | - | - |
| Spada et al[24] 20111 | 109 | 84 | 64 | - | - |
| Results for polyps ≥ 10 mm | |||||
| Eliakim et al[10] 20091 | 98 | 88 | 89 | - | - |
| Spada et al[24] 20111 | 109 | 88 | 95 | - | - |
| Results for other lesions | - | - | - | - | - |
| Schoofs et al[9] 2006 | 41 | 76 | 63 | 82 | 52 |
| Eliakim et al[8] 2006 | 91 | 78 | 76 | 47 | 93 |
| Van Gossum et al[21] 2009 | 320 | 76 | - | - | - |
To estimate the potential impact of PCCE on an asymptomatic population, a small monocentric study enrolling 38 consecutive subjects was performed[22]. Although half of the study population underwent PCCE for screening purposes, 17 patients (45%) were on the work-up of a positive FOBT. Therefore, the study should not be considered representative of a low prevalence of disease screening setting. The study reported a 27% withdrawal rate, presumably related, in the Authors’ opinion, to the extensive bowel preparation required and to the in-hospital setting in which PCCE was performed. Although a good-excellent bowel preparation was achieved in 88% of cases, PCCE sensitivity for polyps of any size was only 65%, whilst a very high 96% specificity was reported for the first time.
The last study available for the first generation of PCCE is a monocentric series of 128 patients in a non-screening setting, aiming to assess post-PCCE colonoscopy referral[23]. When considering the 76% PCCE specificity and a 44% prevalence of significant findings (based on a 6 mm cut-off), such a referral rate appeared to be 56%. The related positive predictive value (79%) would have clearly been lower in a screening setting, where the expected prevalence of significant findings is much lower than 10%.
Not all the studies led to encouraging outcomes. In a prospective multicentre trial[25] comparing PCCE and colonoscopy in asymptomatic subjects enrolled in screening or surveillance programmes for the detection of colorectal neoplasia, the sensitivity and specificity of PCCE for detecting polyps ≥ 6 mm were 39% (95% CI 30-48) and 88% (95% CI 85-91), respectively, with a positive predictive value of 47% (95% CI 37-57) and a negative predictive value of 85% (95% CI 82-88).
In two meta-analyses recently published[26,27], the Authors reported that for polyps of any size, sensitivity values ranged from 71% to 73% and specificity values ranged from 75% to 89%. For significant polyps, the corresponding values were 68%-69% and 82%-86%, respectively.
When weighing the results of all these studies, the first generation of PCCE appeared to be a safe and feasible non-invasive technique to investigate and visualize the colon, but was characterized by suboptimal accuracy and a high degree of variability in its technical performances.
Currently, two multicentre studies[10,24] assessing the performance of the second generation of PCCE are reported in the literature.
The first series is a multicentre Israeli feasibility study, enrolling 104 patients[10]. Bowel preparation was adequate in 78% of patients. PCCE failed to visualize the entire colon in 19% of cases. PCCE sensitivity for polyps ≥ 6 mm and ≥ 10 mm appeared to be 89% and 88%, whilst specificity still appeared to be suboptimal, being 76% and 89%, respectively. In 10 cases, PCCE detected a ≥ 10 mm polyp unidentified by blinded colonoscopy. In 4 out of the 5 cases in which an unblinded colonoscopy was repeated, a previously missed polyp was detected, suggesting that most of the apparent false-positive results with PCCE may be due to false-negatives at colonoscopy or related to size mismatching.
The second recently published prospective multicentre study[24] involving 117 patients in 8 centres also provided very encouraging results. Accuracy parameters were calculated per-patient. Bowel preparation was adequate (good to excellent) in 81% of patients and in 88% of cases the capsule was naturally excreted within 10 hours. Colon capsule endoscopy proved to be highly sensitive for clinically relevant lesions. The sensitivity values of 84% and 88% for polyps ≥ 6 mm and polyps ≥ 10 mm (95% CI) are consistent with the sensitivity rates (89% and 88%, respectively) obtained in the previous Israeli study and are higher for significant polyps (i.e., polyps ≥ 6 mm) than the corresponding results obtained with the first-generation colon capsule (68%-69%)[26,27]. Furthermore, all cancers detected by colonoscopy were also identified on PCCE-2, whereas first-generation colon capsule endoscopy revealed suboptimal sensitivity for cancer. However, a direct comparison between the two generations of colon capsules was beyond the aims of the study and conclusive statements can not be made. The high sensitivity of PCCE-2 may be ascribable to technological improvements and to improvements in the regimen of bowel preparation leading to the higher degree (81%) of adequate bowel preparation. This level of adequate bowel preparation is consistent with the 78% reported in the Israeli study and that reported in a previous study based on PCCE-1 with the same regimen, but is substantially higher than the 72% reported in the above-mentioned meta-analysis of studies with the first generation colon capsule[26,27]. Finally, PCCE-2 specificity for the detection of polyps ≥ 6 mm and ≥ 10 mm was 64% and 95%, respectively (95% CI). An apparently suboptimal specificity of PCCE-2 has also been observed in this series, resulting in a low positive predictive value for post-PCCE-2 colonoscopy, however, the low specificity for polyps ≥ 6 mm can be explained differently. A substantial rate of false positive results was due to size mismatching. Furthermore, it cannot be excluded that apparently false-positive results at PCCE were actually false-negative results at colonoscopy. The overall colon capsule endoscopy accuracy (mean between sensitivity and specificity) for lesions ≥ 6 mm and ≥ 10 mm appeared to be 76% and 92%, respectively. Although the present study included a population with a mean age of 60 years, similar to that of an unselected population referred for colonoscopy, it has also been performed in the Israeli study in an enriched population.
Technical improvements of PCCE-2 and better bowel preparation led to promising results producing a substantial improvement in the polyp and colorectal cancer detection rate of the new generation capsule. Nevertheless, at the moment these results cannot be extended to a screening population. The use of colon capsule endoscopy in an average or low prevalence of disease setting deserves further investigation to pave the way for capsule endoscopy as an additional patient-friendly method to complement colonoscopy for colon visualization and for colorectal cancer screening.
Theoretically, all patients with suspected or known colonic disease referred for a diagnostic colonoscopy could be candidates for a PCCE examination. PCCE may be indicated when a patient refuses conventional colonoscopy or when colonoscopy provides inconclusive results or when the risks from colonoscopy, such as colon perforation (for example when there is a clinical suspicion of acute diverticulitis), may outweigh the benefits.
In up to 10% to 20% of colonoscopies, caecal intubation may be considered difficult[28,29]. Failure to intubate the caecum is not infrequent[29,30], occurring in about 14% of colonoscopies[31-34]. In these cases, alternative endoscopic diagnostic pathways have been described, including the use of single-or double-balloon endoscopy[35-44]. PCCE could provide an easy and painless way to explore difficult colons and avoid exposing patients to the risk of repeated colonoscopy attempts[45]. In the series by Triantafyllou et al[46], of 12 patients with incomplete colonoscopy due to neoplastic stricture (6 cases) or difficult anatomy (6 cases), PCCE was conclusive in 5/6 patients with neoplastic stricture and in 1 of 6 patients with technical difficulties. Further studies on larger populations are needed to confirm the efficacy of PCCE in patients with incomplete colonoscopy.
The ideal candidates for PCCE are patients at low risk of lesions requiring a post-PCCE colonoscopy and consequently avoiding useless duplication of endoscopic procedures. The rational use of PCCE should be as a filter for therapeutic colonoscopy, hence avoiding a number of negative colonoscopies. Clinical indications less frequently associated with the need of biopsies or therapeutic procedures (such as endoscopic resection) are constipation, abdominal pain, and surveillance after surgical resection of CRC. However, it is still unknown whether surgical anastomosis represents a contraindication to PCCE.
Currently, PCCE should not be considered an alternative to conventional colonoscopy. Further studies are needed in order to assess whether it may replace conventional colonoscopy for non-operative indications. However, based on current available studies, PCCE may be a valid complement to standard colonoscopy in cases of incomplete or difficult colonoscopy[45,46], contraindication to conventional colonoscopy or in patients who are unwilling to undergo colonoscopy.
Chronic inflammatory bowel disease may represent another potential indication for PCCE. Although at present few data are available in the literature, PCCE might play a role in establishing the diagnosis of IBD, monitoring disease location, extent, activity and severity, monitoring mucosal healing, establishing disease prognosis and assessing acute severe colitis and post-surgical recurrences. Among diagnostic tests, ileo-colonoscopy with biopsies represents the gold standard for the diagnosis of IBD, but in several situations histology and the other classic diagnostic tests might be inconclusive.
An advantage of PCCE is that it can allow complete evaluation of the gastrointestinal tract. Monitoring the disease extent has important implications in the treatment strategy for IBD patients; the extension of disease suggests the more effective route of drug administration (topical therapy, enemas, combined oral and topical treatment). Monitoring disease extent also impacts on the prognosis as patients with proctitis or left-sided colitis have a better prognosis than those whose colon is extensively involved[47]. The extent of disease also determines the beginning and frequency of surveillance for colorectal cancer.
Despite not yet being included in official guidelines for IBD-treatment and assessment, mucosal healing (MH) may become an important goal of treatment for patients with IBD. Wireless capsule endoscopy is the only method, except for double-balloon enteroscopy, for accurate assessment of mucosal healing in Crohn’s disease. Based upon new evidence, MH can influence the course of IBD because it is associated with a sustained clinical remission and with lower hospitalization and resection rates[48-56]. In this setting, endoscopy will be indicated also to guide a therapeutic decision[57,58] and PCCE may overcome the invasiveness and the risks of conventional endoscopy and could be used to assess mucosal changes.
In cases of moderate-to-severe disease, PCCE could be a valid alternative to colonoscopy and sigmoidoscopy, allowing assessment of the extent of the disease and establishing whether the whole colon and ileum are involved and at the same time avoiding the higher risk of bowel perforation[59].
Within 20 years of the onset of their disease, 75% of patients suffering from Crohn’s disease require surgery[60]. Endoscopic evaluation is advisable in the first 6-12 mo after resection to identify any early recurrence and the prompt initiation of aggressive therapy[61]. PCCE might offer the same accuracy as small bowel capsule endoscopy in assessing the ileum and neoterminal ileum, and may have the advantage of exploring the whole colon.
The role of PCCE in IBD has only been evaluated in one series of 42 patients with suspected or known ulcerative celitis (UC)[62]. The aim of the study, published in abstract form, was to assess the accuracy of PCCE as compared to conventional colonoscopy in monitoring colonic inflammation in this subset of patients. Sensitivity, specificity, PPV and NPV values of PCCE for diagnosing UC were 77%, 78%, 81% and 74%, respectively.
To date there is no evidence that PCCE may be indicated in the diagnostic work up or in the surveillance of patients with suspected or known IBD, but this is an attractive field of further investigation.
One of the main challenges with colon capsule endoscopy is bowel cleansing. Because of the intrinsic inability of PCC to inflate, suck or wash, preparation should aim to clean the colon as thoroughly as possible, to allow a “natural” colonic distension by filling the lumen with clear liquids and facilitating the so-called submarine view and, at the same time, to propel the capsule within the battery life-time through the small bowel and the entire colon, the latter characterized by few longitudinal contractions per day. Even small amounts of residual stool may prevent accurate visualization of the colonic mucosa.
The preparation regimen consists of conventional colonoscopy preparation adapted with additional laxative boosters and prokinetics in order to meet the above-mentioned purposes. As for conventional colonoscopy, the patient is asked to follow a low-fibre diet and the day before capsule ingestion to drink polyethylene glycol solution. After the capsule has been ingested, additional laxative stimulants and prokinetic agents are provided to the patient in order to maintain cleanliness of the colon during the transit of the capsule and enhance capsule propulsion and excretion within 9-10 h.
The most extensively tested preparation protocol in PCCE trials was originally described by Schoofs et al[9]. The Belgian preparation regimen includes an oral preparation of polyethylene glycol solution and sodium phosphate boosters (Table 2). Using this protocol, colonic preparation was judged adequate (good-excellent) in a median of 77% (range 35%-89%) of cases[9,21,23]. The largest study so far published (the European multicentre trial) showed an overall adequate cleansing level in 72% of patients[21]. This result is consistent with that of a recent meta-analysis which showed a median excellent-good level of 77%[27]. As far as the PCC natural excretion rate is concerned, a 100% excretion rate within the battery life-time is among the main goals of any preparation regimen, in order to ensure complete visualization of the entire colon with PCCE in all cases. Preliminary studies performed using the same preparation as conventional colonoscopy showed low capsule excretion rates (about 20%) resulting in a high rate of incomplete PCCE. For this reason, the colonic preparation was adapted to PCCE and additional doses of stimulants (sodium phosphate boosters) after capsule ingestion were included in the preparation protocols to promote capsule propulsion and enhance capsule excretion within 9-10 h after ingestion[22,63]. When sodium phosphate is removed, the excretion rate drops affecting completion rate of PCCE[22]. The substitution of NaP with PEG-boosters was not effective[63]. However, the inclusion of sodium phosphate booster to PCCE may raise some concern, as it is associated in colonoscopy with major complications such as electrolyte disturbance, acute nephropathy and kidney failure[64]. Using the Belgian regimen, natural excretion within 10 h was observed in a median of 92% (range 83%-100%) of patients, when pooling the available series[9,21,23,63]. This rate of complete examination with PCCE appears to be very close to the 95% threshold value recommended for screening colonoscopy.
| Day | Time | Action |
| −1 | All day | Liquid diet only |
| 6:00 pm–9:00 pm | 3 L PEG | |
| Exam day | 6:00 am–7:00 am | 1 L PEG |
| 7.45 am | Domperidone (20 mg) | |
| 8:00 am | PillCam ingestion | |
| 10:00 am | 45 mL NaP + 1 L water1 | |
| 02:00 pm | 30 mL NaP + 1 L water | |
| 03:00 pm | Snack (optional) | |
| 4.30 pm | 10 mg Bisacodyl (suppository) |
Eliakim et al[10] (Table 3) described a new protocol for colon preparation for second-generation colon capsule endoscopy. This regimen envisages a more balanced split-dose of PEG solution (2 litres on the evening before and 2 litres on the day of capsule ingestion), a low dose of sodium phosphate boosters, and the use of domperidone only if stomach emptying is delayed for more than 1 h. Using this regimen, the Authors reported an adequate cleansing level in 78% of patients and an excretion rate within 8 h in 81% of capsule colonoscopies[10]. This excretion rate might be regarded as low. This new regimen of preparation seems advisable for three main reasons: (1) the split-dose PEG solution suggested in this protocol theoretically appears to be more tolerable for patients and may increase compliance to the preparation; (2) the lower doses of sodium phosphate boosters is likely to decrease the risk of sodium phosphate-related adverse events; and (3) colonic cleanliness and excretion rates are encouraging although still suboptimal.
| Day | Time | Action |
| −1 | All day | Liquid diet only |
| 7:00 pm–9:00 pm | 2 L PEG | |
| Exam day | 8:00 am–9:00 am | 2 L PEG |
| 10:00 am | PillCam ingestion1 | |
| 1st booster (at small bowel detection) | 30 mL NaP + 1 L water | |
| 2nd booster (3 h after 1st booster) | 15 mL NaP + 0.5 L water | |
| Suppository (2 h after 2nd booster) | 10 mg Bisacodyl (suppository) |
Recently Spada et al[65] experimented with a bowel preparation regimen starting with a low-fibre diet 5 d to 2 d before the procedure and further consisting of (1) four senna tablets at bedtime 2 d before the examination day; (2) clear liquid diet the day before examination; (3) four litres of polyethylene glycol solution split into two doses (on the evening and on the morning of examination; and (4) prokinetics and additional doses of sodium phosphate boosters after capsule ingestion and a bisacodyl suppository if the capsule is not expelled approximately five h after the first boost (Table 4). Forty-six patients were included in the final analysis. At PCCE, bowel preparation was rated as good in 78% of patients, fair in 20% and poor in 2%. PCCE excretion occurred in 83% of patients. PCCE sensitivity and specificity for significant findings were 100% and 95%, respectively, confirming that the combination of a split-dose of PEG solution with a low dose of sodium phosphate boosters resulted in high rates of adequate cleansing level and PCCE excretion.
| Day | Time | Action |
| −5 to −2 | All day | Low fibre diet |
| −2 | 08:00 pm | 4 senna tablets (48mg) |
| −1 | All day | Liquid diet only |
| 7:00 pm–9:00 pm | 2 L PEG | |
| Exam day | 6:00 am–8:00 am | 2 L PEG |
| 8:45 am | Domperidone (20 mg) | |
| 9:00 am | PillCam ingestion | |
| 11:00 am | 30 mL NaP + 1 L water1 | |
| 02:00 pm | 15 mL NaP + ½ L water | |
| 04:00 pm | 10 mg Bisacodyl (suppository) | |
| 07:00 pm | Colonoscopy |
This same regimen was used in the more recent European multicenter study comparing PCCE-2 with colonoscopy for detecting colorectal polyps[24]. Overall, 88% of the capsules were naturally excreted within 10 h after ingestion and the overall cleansing level was judged adequate in 81% of cases. This level of adequate bowel preparation is comparable to the 78% reported in the Israeli study, but whether those results are satisfactory is still questionable.
Multiple studies using different regimens of bowel preparation are ongoing in order to identify a preparation regimen that combines high rates of adequate cleansing level and capsule excretion.
Colonic preparation for colon capsule still represents a crucial issue, potentially compromising the accuracy of PCCE. The performance of PCCE is strictly dependent on the quality of colonic preparation. Agents that effectively enhance capsule propulsion should always be included in the preparation protocols for PCCE. Sodium phosphate that seems to be indispensable in the propulsion of the videocapsule through the colon has been withdrawn from sale in the US due to side-effects. Studies are underway using low volume PEG and bisacodyl as an engine but as yet no results are available.
The PCCE seems to be a safe procedure. No examination-related adverse events have been reported in the first feasibility studies[8,9,18,21]. Two of 126 patients (1.6%) were unable to swallow the capsule in the study by Eliakim et al[8]. Inability to ingest the capsule occurred with the PCCE-2 in less than 1% of cases[10,24]. Swallowing problems can be easily overcome by introducing the capsule into the stomach or duodenum by means of the capsule endoscopy delivery system (US Endoscopy). As demonstrated by several studies, patients’ compliance for CRC screening is still much lower than that for other common neoplastic diseases. PCCE may be an attractive patient-friendly non-invasive method for CRC screening, especially for those patients who are non-compliant to current screening procedures. The cost-effective of PCCE has not been assessed. However, a recent paper by Hassan et al[66] based on a mathematical Markov model concludes that PCCE may be a cost-effective option compared with colonoscopy if patient adherence is increased by 30%. The cost-effectiveness of capsule endoscopy in CRC screening mainly depends on its ability to improve compliance in the general population.
Based on current available studies, PCCE is a feasible, effective and safe procedure that allows visualization of the entire colon in most cases. It may be complementary to conventional colonoscopy and could be appropriate for patients who have received an incomplete colonoscopy, who have contraindications to colonoscopy or are unwilling to undergo conventional colonoscopy.
PCCE may be preferred in patients in areas with a low prevalence of disease, in order to avoid an unnecessary rate of post-PCCE colonoscopy. In this setting, CCE might be used as a high adherence filter for therapeutic colonoscopy. Finally, at present, PCCE represents the only imaging test that may be administered at the patient’s home with clear advantages in terms of acceptability and feasibility for an imaging population-screening test and because of its non-invasiveness, safety, and lack of ionizing radiation, would also appear to be a promising tool for the diagnosis and management of IBD patients.
Another important issue is selection bias of patients in the studies performed so far. All these studies included symptomatic patients. To date, no studies have been performed in a low prevalence of disease setting. Upcoming studies are needed to clarify the substantial utility of colon capsule endoscopy in an unselected screening population particularly as competitor methods, such as CT-colonography, have shown great performance.
Bowel preparation is the most challenging factor in PCCE implementation. A reasonable balance between adequate preparation and patient satisfaction needs to be pursued, and the adoption of a split regimen of PEG is a step in this direction. Suboptimal accuracy of the first generation of PCCE was partly related to technical factors which have been successfully addressed in the second generation of PCCE.
Peer reviewer: Reena Sidhu, MRCP, MD, Department of Gastroenterology, Royal Hallamshire Hospital, 15 Barncliffe Road, Fulwood, Sheffield S10 4DF, United Kingdom
S- Editor Yang XC L- Editor Webster JR E- Editor Yang XC
| 1. | Mishkin DS, Chuttani R, Croffie J, Disario J, Liu J, Shah R, Somogyi L, Tierney W, Song LM, Petersen BT. ASGE Technology Status Evaluation Report: wireless capsule endoscopy. Gastrointest Endosc. 2006;63:539-545. [PubMed] [DOI] [Cited in This Article: ] |
| 2. | Adler DG, Chand B, Conway JD, Diehl DL, Kantsevoy SV, Kwon RS, Mamula P, Rodriguez SA, Shah RJ, Song LM. Capsule endoscopy of the colon. Gastrointest Endosc. 2008;68:621-623. [PubMed] [DOI] [Cited in This Article: ] |
| 3. | Principi M, De Tullio N, Guido R, Pisani A, Francavilla A, Di Leo A. E-Worm and Pillcam Colon Capsule: fesability and patient acceptance. [abstract]. Digestive and Liver Disease. 2009;41S:S1–S167. [Cited in This Article: ] |
| 4. | Dominitz JA, Eisen GM, Baron TH, Goldstein JL, Hirota WK, Jacobson BC, Johanson JF, Leighton JA, Mallery JS, Raddawi HM. Complications of colonoscopy. Gastrointest Endosc. 2003;57:441-445. [PubMed] [DOI] [Cited in This Article: ] |
| 5. | Nelson DB, McQuaid KR, Bond JH, Lieberman DA, Weiss DG, Johnston TK. Procedural success and complications of large-scale screening colonoscopy. Gastrointest Endosc. 2002;55:307-314. [PubMed] [DOI] [Cited in This Article: ] |
| 6. | Korman LY, Overholt BF, Box T, Winker CK. Perforation during colonoscopy in endoscopic ambulatory surgical centers. Gastrointest Endosc. 2003;58:554-557. [PubMed] [DOI] [Cited in This Article: ] |
| 7. | Nadel MR, Blackman DK, Shapiro JA, Seeff LC. Are people being screened for colorectal cancer as recommended? Results from the National Health Interview Survey. Prev Med. 2002;35:199-206. [PubMed] [DOI] [Cited in This Article: ] |
| 8. | Eliakim R, Fireman Z, Gralnek IM, Yassin K, Waterman M, Kopelman Y, Lachter J, Koslowsky B, Adler SN. Evaluation of the PillCam Colon capsule in the detection of colonic pathology: results of the first multicenter, prospective, comparative study. Endoscopy. 2006;38:963-970. [PubMed] [DOI] [Cited in This Article: ] |
| 9. | Schoofs N, Devière J, Van Gossum A. PillCam colon capsule endoscopy compared with colonoscopy for colorectal tumor diagnosis: a prospective pilot study. Endoscopy. 2006;38:971-977. [PubMed] [DOI] [Cited in This Article: ] |
| 10. | Eliakim R, Yassin K, Niv Y, Metzger Y, Lachter J, Gal E, Sapoznikov B, Konikoff F, Leichtmann G, Fireman Z. Prospective multicenter performance evaluation of the second-generation colon capsule compared with colonoscopy. Endoscopy. 2009;41:1026-1031. [PubMed] [DOI] [Cited in This Article: ] |
| 11. | Triantafyllou K, Papanikolaou IS, Papaxoinis K, Ladas SD. Two cameras detect more lesions in the small-bowel than one. World J Gastroenterol. 2011;17:1462-1467. [PubMed] [Cited in This Article: ] |
| 12. | Ibanez MB, Ribon CC, de la Torre FT, Munoz-Navas M. Evidencia científica en cribado del cáncer colorrectal: manual de actuacion. Madrid: International Marketing and Communication 2006; . [Cited in This Article: ] |
| 13. | Dolinský A, Kolesár J. [Chronic obstructive lung disease in the spirographic and x-ray picture. Stage of general deterioration]. Vnitr Lek. 1973;19:124-134. [PubMed] [DOI] [Cited in This Article: ] |
| 14. | Betés Ibáñez M, Muñoz-Navas MA, Duque JM, Angós R, Macías E, Súbtil JC, Herraiz M, de la Riva S, Delgado-Rodríguez M, Martínez-Gonzélez MA. Diagnostic value of distal colonic polyps for prediction of advanced proximal neoplasia in an average-risk population undergoing screening colonoscopy. Gastrointest Endosc. 2004;59:634-641. [PubMed] [DOI] [Cited in This Article: ] |
| 15. | Silva AC, Wellnitz CV, Hara AK. Three-dimensional virtual dissection at CT colonography: unraveling the colon to search for lesions. Radiographics. 2006;26:1669-1686. [PubMed] [DOI] [Cited in This Article: ] |
| 16. | Johnson KT, Carston MJ, Wentz RJ, Manduca A, Anderson SM, Johnson CD. Development of a cathartic-free colorectal cancer screening test using virtual colonoscopy: a feasibility study. AJR Am J Roentgenol. 2007;188:W29-W36. [PubMed] [DOI] [Cited in This Article: ] |
| 17. | Chaoui AS, Barish MA. Virtual colonoscopy: a new tool for colorectal cancer screening. Curr Opin Gastroenterol. 2001;17:78-85. [PubMed] [Cited in This Article: ] |
| 18. | Lewis B, Rex D, Lieberman D. Capsule Colonoscopy: An Interim Report of a Pilot 3 Arm, Blinded Trial of Capsule Colonoscopy, Virtual Colonoscopy and Colonoscopy. Am J Gastroenterol. 2006;101:S545–S561. [Cited in This Article: ] |
| 19. | Leighton JA, Rex DK. A grading scale to evaluate colon cleansing for the PillCam COLON capsule: a reliability study. Endoscopy. 2011;43:123-127. [PubMed] [DOI] [Cited in This Article: ] |
| 20. | Mussetto A, Triossi O, Gasperoni S, Casetti T. Colon capsule endoscopy may represent an effective tool for colorectal cancer screening: A single-centre series. Dig Liver Dis. 2012;44:357-358. [PubMed] [Cited in This Article: ] |
| 21. | Van Gossum A, Munoz-Navas M, Fernandez-Urien I, Carretero C, Gay G, Delvaux M, Lapalus MG, Ponchon T, Neuhaus H, Philipper M. Capsule endoscopy versus colonoscopy for the detection of polyps and cancer. N Engl J Med. 2009;361:264-270. [PubMed] [Cited in This Article: ] |
| 22. | Sieg A, Friedrich K, Sieg U. Is PillCam COLON capsule endoscopy ready for colorectal cancer screening? A prospective feasibility study in a community gastroenterology practice. Am J Gastroenterol. 2009;104:848-854. [PubMed] [DOI] [Cited in This Article: ] |
| 23. | Gay G, Delvaux M, Frederic M, Fassler I. Could the colonic capsule PillCam Colon be clinically useful for selecting patients who deserve a complete colonoscopy?: results of clinical comparison with colonoscopy in the perspective of colorectal cancer screening. Am J Gastroenterol. 2010;105:1076-1086. [PubMed] [DOI] [Cited in This Article: ] |
| 24. | Spada C, Hassan C, Munoz-Navas M, Neuhaus H, Deviere J, Fockens P, Coron E, Gay G, Toth E, Riccioni ME. Second-generation colon capsule endoscopy compared with colonoscopy. Gastrointest Endosc. 2011;74:581-589.e1. [PubMed] [Cited in This Article: ] |
| 25. | Sacher-Huvelin S, Coron E, Gaudric M, Planche L, Benamouzig R, Maunoury V, Filoche B, Frédéric M, Saurin JC, Subtil C. Colon capsule endoscopy vs. colonoscopy in patients at average or increased risk of colorectal cancer. Aliment Pharmacol Ther. 2010;32:1145-1153. [PubMed] [DOI] [Cited in This Article: ] |
| 26. | Rokkas T, Papaxoinis K, Triantafyllou K, Ladas SD. A meta-analysis evaluating the accuracy of colon capsule endoscopy in detecting colon polyps. Gastrointest Endosc. 2010;71:792-798. [PubMed] [DOI] [Cited in This Article: ] |
| 27. | Spada C, Hassan C, Marmo R, Petruzziello L, Riccioni ME, Zullo A, Cesaro P, Pilz J, Costamagna G. Meta-analysis shows colon capsule endoscopy is effective in detecting colorectal polyps. Clin Gastroenterol Hepatol. 2010;8:516-522. [PubMed] [DOI] [Cited in This Article: ] |
| 28. | Witte TN, Enns R. The difficult colonoscopy. Can J Gastroenterol. 2007;21:487-490. [PubMed] [Cited in This Article: ] |
| 29. | Rex DK. Achieving cecal intubation in the very difficult colon. Gastrointest Endosc. 2008;67:938-944. [PubMed] [Cited in This Article: ] |
| 30. | Spiegel BM, Talley J, Alvarez E, Bolus RE, Kurzbard N, Ho A, Kaneshiro M, Cohen H. Impact of a novel patient educational booklet on colonoscopy preparation quality: results of a randomized controlled trial. Gastroenterology. 2010;138:S56. [Cited in This Article: ] |
| 31. | Shah HA, Paszat LF, Saskin R, Stukel TA, Rabeneck L. Factors associated with incomplete colonoscopy: a population-based study. Gastroenterology. 2007;132:2297-2303. [PubMed] [DOI] [Cited in This Article: ] |
| 32. | Loffeld RJ, van der Putten AB. The completion rate of colonoscopy in normal daily practice: factors associated with failure. Digestion. 2009;80:267-270. [PubMed] [DOI] [Cited in This Article: ] |
| 33. | Anderson JC, Gonzalez JD, Messina CR, Pollack BJ. Factors that predict incomplete colonoscopy: thinner is not always better. Am J Gastroenterol. 2000;95:2784-2787. [PubMed] [DOI] [Cited in This Article: ] |
| 34. | Anderson JC, Messina CR, Cohn W, Gottfried E, Ingber S, Bernstein G, Coman E, Polito J. Factors predictive of difficult colonoscopy. Gastrointest Endosc. 2001;54:558-562. [PubMed] [DOI] [Cited in This Article: ] |
| 35. | Teshima CW, Aktas H, Haringsma J, Kuipers EJ, Mensink PB. Single-balloon-assisted colonoscopy in patients with previously failed colonoscopy. Gastrointest Endosc. 2010;71:1319-1323. [PubMed] [DOI] [Cited in This Article: ] |
| 36. | Moreels TG, Macken EJ, Roth B, Van Outryve MJ, Pelckmans PA. Cecal intubation rate with the double-balloon endoscope after incomplete conventional colonoscopy: a study in 45 patients. J Gastroenterol Hepatol. 2010;25:80-83. [PubMed] [DOI] [Cited in This Article: ] |
| 37. | Delvaux M, Gay G. Novel applications of balloon endoscopy. Gastrointest Endosc Clin N Am. 2009;19:509-518. [PubMed] [DOI] [Cited in This Article: ] |
| 38. | Gay G, Delvaux M. Double-balloon colonoscopy after failed conventional colonoscopy: a pilot series with a new instrument. Endoscopy. 2007;39:788-792. [PubMed] [DOI] [Cited in This Article: ] |
| 39. | Kita H, Yamamoto H. New indications of double balloon endoscopy. Gastrointest Endosc. 2007;66:S57-S59. [PubMed] [Cited in This Article: ] |
| 40. | Mönkemüller K, Knippig C, Rickes S, Fry LC, Schulze A, Malfertheiner P. Usefulness of the double-balloon enteroscope in colonoscopies performed in patients with previously failed colonoscopy. Scand J Gastroenterol. 2007;42:277-278. [PubMed] [DOI] [Cited in This Article: ] |
| 41. | Pasha SF, Harrison ME, Das A, Corrado CM, Arnell KN, Leighton JA. Utility of double-balloon colonoscopy for completion of colon examination after incomplete colonoscopy with conventional colonoscope. Gastrointest Endosc. 2007;65:848-853. [PubMed] [DOI] [Cited in This Article: ] |
| 42. | Lo SK. Technical matters in double balloon enteroscopy. Gastrointest Endosc. 2007;66:S15-S18. [PubMed] [Cited in This Article: ] |
| 43. | Kaltenbach T, Soetikno R, Friedland S. Use of a double balloon enteroscope facilitates caecal intubation after incomplete colonoscopy with a standard colonoscope. Dig Liver Dis. 2006;38:921-925. [PubMed] [DOI] [Cited in This Article: ] |
| 44. | May A, Nachbar L, Ell C. Push-and-pull enteroscopy using a single-balloon technique for difficult colonoscopy. Endoscopy. 2006;38:395-398. [PubMed] [DOI] [Cited in This Article: ] |
| 45. | Spada C, Riccioni ME, Petruzziello L, Marchese M, Urgesi R, Costamagna G. The new PillCam Colon capsule: difficult colonoscopy? No longer a problem? Gastrointest Endosc. 2008;68:807-808. [PubMed] [DOI] [Cited in This Article: ] |
| 46. | Triantafyllou K, Tsibouris P, Kalantzis C, Papaxoinis K, Kalli T, Kalantzis N, Ladas SD. PillCam Colon capsule endoscopy does not always complement incomplete colonoscopy. Gastrointest Endosc. 2009;69:572-576. [PubMed] [DOI] [Cited in This Article: ] |
| 47. | Moum B, Ekbom A, Vatn MH, Elgjo K. Change in the extent of colonoscopic and histological involvement in ulcerative colitis over time. Am J Gastroenterol. 1999;94:1564-1569. [PubMed] [DOI] [Cited in This Article: ] |
| 48. | Henriksen M, Jahnsen J, Lygren I, Sauar J, Kjellevold Ø, Schulz T, Vatn MH, Moum B. Ulcerative colitis and clinical course: results of a 5-year population-based follow-up study (the IBSEN study). Inflamm Bowel Dis. 2006;12:543-550. [PubMed] [DOI] [Cited in This Article: ] |
| 49. | van Dullemen HM, van Deventer SJ, Hommes DW, Bijl HA, Jansen J, Tytgat GN, Woody J. Treatment of Crohn's disease with anti-tumor necrosis factor chimeric monoclonal antibody (cA2). Gastroenterology. 1995;109:129-135. [PubMed] [Cited in This Article: ] |
| 50. | Arnott ID, Watts D, Ghosh S. Review article: is clinical remission the optimum therapeutic goal in the treatment of Crohn's disease? Aliment Pharmacol Ther. 2002;16:857-867. [PubMed] [DOI] [Cited in This Article: ] |
| 51. | Kane S. Endoscopic healing should be a goal for everyone with ulcerative colitis. Inflamm Bowel Dis. 2008;Nov 4 [Epub ahead of print]. [PubMed] [DOI] [Cited in This Article: ] |
| 52. | Lichtenstein GR, Rutgeerts P. Importance of mucosal healing in ulcerative colitis. Inflamm Bowel Dis. 2010;16:338-346. [PubMed] [DOI] [Cited in This Article: ] |
| 53. | Rutgeerts P, Vermeire S, Van Assche G. Mucosal healing in inflammatory bowel disease: impossible ideal or therapeutic target? Gut. 2007;56:453-455. [PubMed] [DOI] [Cited in This Article: ] |
| 54. | Rutgeerts P, Diamond RH, Bala M, Olson A, Lichtenstein GR, Bao W, Patel K, Wolf DC, Safdi M, Colombel JF. Scheduled maintenance treatment with infliximab is superior to episodic treatment for the healing of mucosal ulceration associated with Crohn's disease. Gastrointest Endosc. 2006;63:433-42; quiz 464. [PubMed] [DOI] [Cited in This Article: ] |
| 55. | Schnitzler F, Fidder H, Ferrante M, Noman M, Arijs I, Van Assche G, Hoffman I, Van Steen K, Vermeire S, Rutgeerts P. Mucosal healing predicts long-term outcome of maintenance therapy with infliximab in Crohn's disease. Inflamm Bowel Dis. 2009;15:1295-1301. [PubMed] [DOI] [Cited in This Article: ] |
| 56. | Rutgeerts P, Sandborn WJ, Feagan BG, Reinisch W, Olson A, Johanns J, Travers S, Rachmilewitz D, Hanauer SB, Lichtenstein GR. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2005;353:2462-2476. [PubMed] [DOI] [Cited in This Article: ] |
| 57. | Colombel JF, Sandborn WJ, Reinisch W, Mantzaris GJ, Kornbluth A, Rachmilewitz D, Lichtiger S, D'Haens G, Diamond RH, Broussard DL. Infliximab, azathioprine, or combination therapy for Crohn's disease. N Engl J Med. 2010;362:1383-1395. [PubMed] [DOI] [Cited in This Article: ] |
| 58. | Louis E. Immunosuppressant combined with infliximab in Crohn's Disease: for 6 months, for 2 years, or forever? Inflamm Bowel Dis. 2011;17:858-859. [PubMed] [DOI] [Cited in This Article: ] |
| 59. | Carter MJ, Lobo AJ, Travis SP. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2004;53 Suppl 5:V1-16. [PubMed] [Cited in This Article: ] |
| 60. | Mekhjian HS, Switz DM, Melnyk CS, Rankin GB, Brooks RK. Clinical features and natural history of Crohn's disease. Gastroenterology. 1979;77:898-906. [PubMed] [Cited in This Article: ] |
| 61. | Binder V, Hendriksen C, Kreiner S. Prognosis in Crohn's disease--based on results from a regional patient group from the county of Copenhagen. Gut. 1985;26:146-150. [PubMed] [Cited in This Article: ] |
| 62. | Sung JJY, Ching JY, Leung WK, Chow DK, Siu D. Assessment of colonic inflammatory lesions and ulcerative colitis with PillCam Colon Capsule Endoscopy compared to colonoscopy. Endoscopy. 2008;40:A199. [Cited in This Article: ] |
| 63. | Spada C, Riccioni ME, Hassan C, Petruzziello L, Cesaro P, Costamagna G. PillCam colon capsule endoscopy: a prospective, randomized trial comparing two regimens of preparation. J Clin Gastroenterol. 2011;45:119-124. [PubMed] [DOI] [Cited in This Article: ] |
| 64. | Wexner SD, Beck DE, Baron TH, Fanelli RD, Hyman N, Shen B, Wasco KE. A consensus documenton bowel preparation before colonoscopy: prepared by a task force from the American Society of Colon and Rectal Surgeons (ASCRS), the American Society for Gastrointestinal Endoscopy (ASGE), and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). Gastrointest Endosc. 2006;63:894–909. [DOI] [Cited in This Article: ] |
| 65. | Spada C, Hassan C, Ingrosso M, Repici A, Riccioni ME, Pennazio M, Pirozzi GA, Pagano N, Cesaro P, Spera G. A new regimen of bowel preparation for PillCam colon capsule endoscopy: a pilot study. Dig Liver Dis. 2011;43:300-304. [PubMed] [DOI] [Cited in This Article: ] |