Published online Sep 16, 2020. doi: 10.4253/wjge.v12.i9.310
- This article has been corrected.
- See: World J Gastrointest Endosc. Nov 16, 2022; 14(11): 737-738
Peer-review started: April 9, 2020
First decision: June 8, 2020
Revised: July 9, 2020
Accepted: August 4, 2020
Article in press: August 4, 2020
Published online: September 16, 2020
Situs inversus totalis (SIT) is a rare anomaly in which structures are located opposite to their usual positions. It is not a premalignant condition and the association with colorectal cancer (CRC) is rare. We here report a patient with SIT who underwent laparoscopic radical resection of sigmoid colon cancer, and review the pertinent literature.
A 53-year-old woman presented with CRC and SIT and underwent a complete examination after admission. The patient then underwent laparoscopic radical resection of sigmoid colon cancer and hyperthermic intraperitoneal chemotherapy. The operation duration was 120 min, and no intraoperative complications occurred. The final pathological report showed stage T4aN0M0. Postoperative chemotherapy was administered and no evidence of recurrence was observed during 18 mo of follow-up.
Surgery in a patient with CRC and SIT can be safely performed on the basis of routine preoperative clinical examination.
Core Tip: Situs inversus totalis is a rare anomaly in which structures are located opposite to their usual positions. It is not a premalignant condition and the association with colorectal cancer is rare. We here report a case and review the literature. In sum, a 53-year-old woman presented with colorectal cancer and situs inversus totalis and underwent a complete examination after admission. The patient then underwent laparoscopic radical resection of sigmoid colon cancer and hyperthermic intraperitoneal chemotherapy. The final pathological report showed stage T4aN0M0. Postoperative chemotherapy was administered and no evidence of recurrence was observed during 18 mo of follow-up.
- Citation: Chen W, Liang JL, Ye JW, Luo YX, Huang MJ. Laparoscopy-assisted resection of colorectal cancer with situs inversus totalis: A case report and literature review. World J Gastrointest Endosc 2020; 12(9): 310-316
- URL: https://www.wjgnet.com/1948-5190/full/v12/i9/310.htm
- DOI: https://dx.doi.org/10.4253/wjge.v12.i9.310
Situs inversus totalis (SIT) refers to the complete reversal of unpaired tissues and organs in the thoracic and abdominal cavity. It is an extremely rare congenital disease with an incidence of approximately 1/4000-8000[1]. According to statistics, the incidence of intestinal cancer is about 376.3/100000, and patients with intestinal cancer and visceral transposition are even rare. When lesions of internal organs in the reverse position occur, patients are easily misdiagnosed if imaging data are not available. We here report a patient with complete visceral transposition combined with sigmoid colon cancer. To the best of our knowledge, this is the first case report of sigmoid colon cancer associated with SIT in China. We also review the relevant literature and discuss the diagnosis and treatment of this patient.
In December 2017, a 53-year-old woman was admitted to our hospital due to lower abdominal discomfort for 1 wk.
The patient’s symptoms started a week ago with recurrent lower abdominal discomfort, which had been worsened the last 24 h.
The patient had a free previous medical history.
Initial vital signs were stable, and a systemic review and physical examination revealed nothing of note. However, the apex beat of her heart was located in the fifth intercostal space of the right clavicle midline.
Serum carcinoembryonic antigen level was elevated (68.5 ng/mL; reference range, 0–5.0 ng/mL).
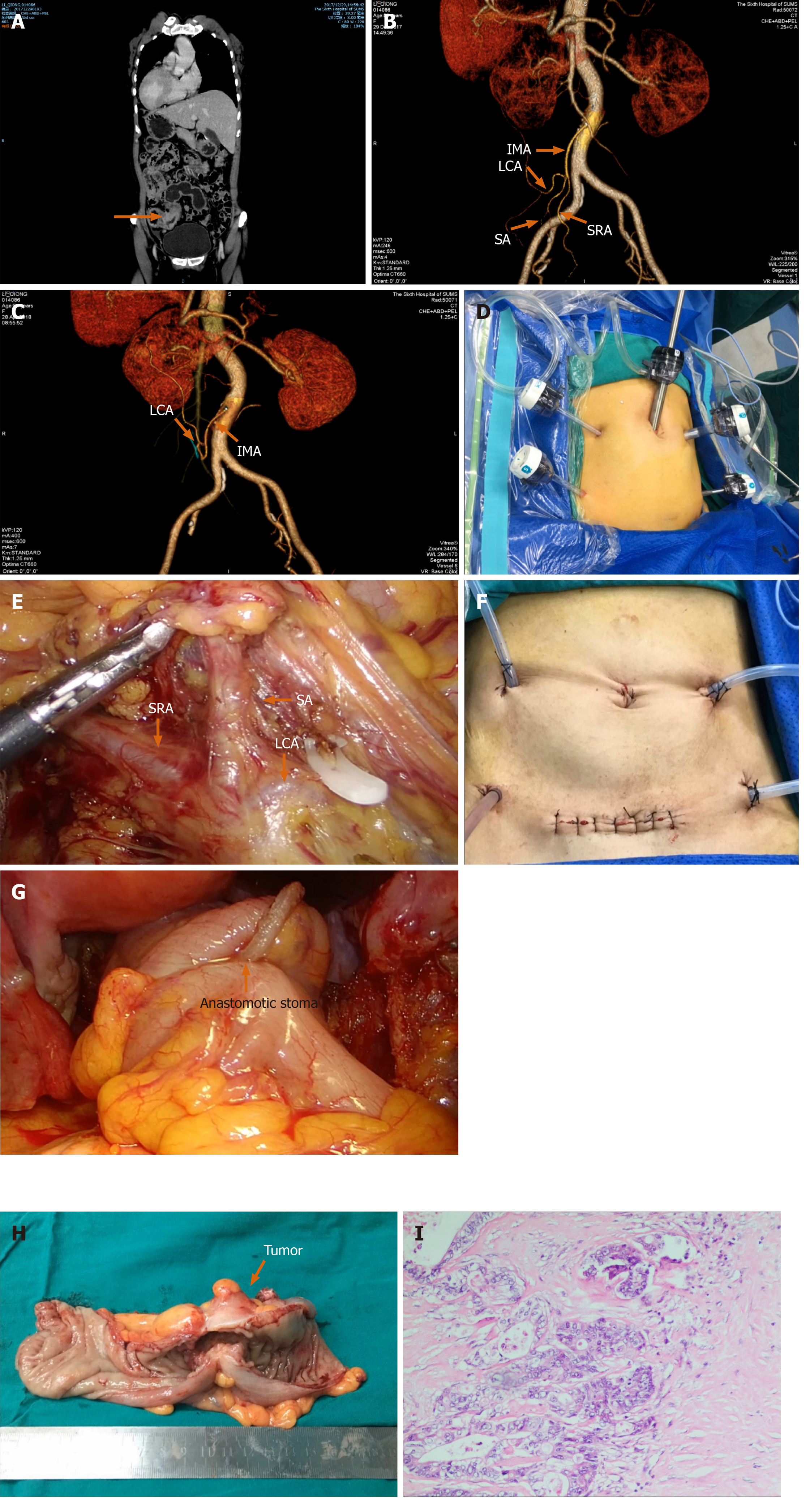
Colonoscopy revealed an obstructing sigmoid mass. Histological examination of the biopsied specimen indicated a moderately differentiated adenocarcinoma. Preoperative thoracic and abdominal enhanced computed tomography showed a complete right-left reversal of the thoracic and abdominal organs, sigmoid colon wall thickening, and the surrounding mesentery scattered with lymph nodes around the primary tumor (Figure 1A). A three-dimensional vascular reconstruction technique was used to observe the anatomy and variation of mesenteric vessels, and the anatomy of the vascular arch was clearly displayed (Figure 1B and C).
The final diagnosis was CRC with SIT.
On January 5, 2018, under general anesthesia, laparoscopic radical sigmoidectomy was performed and hyperthermic intraperitoneal chemotherapy was administered twice (Figure 1D and G). The surgical method of low ligation in combination with highly selective lymph node dissection was adopted to preserve the left colic artery in order to lower the postoperative incidence of anastomotic fistula. Postoperative pathological staging was T4aN0M0 based on the criteria proposed by the International Union Against Cancer (Figure 1H and I).
The patient recovered well after surgery, and regular chemotherapy (mFOLFOX6) was performed 8 times. During the regular 18 mo of follow-up, no tumor recurrence was observed and the patient’s general condition was good.
We searched the compact disc read-only memory database of Chinese biomedical literature and the PubMed-indexed for MEDLINE search system to retrieve reports on visceral transposition combined with intestinal cancer published from January 2000 to May 2019. The Chinese search terms used were “visceral transposition” and “intestinal cancer”, and the English search terms used were “colorectal cancer” and “situs inversus”. Finally, 2 Chinese articles and 11 English articles were identified (Table 1)[1-13].
| Ref. | Publication time | Number of examples | Sex/Age (yr) | Tumor location | Pathological examination | Therapy | Prognosis |
| Fang et al[2] | 2014 | 1 | Female/39 | Rectum | Moderately differentiated adenocarcinoma | Laparoscopic surgery | Good |
| Xu et al[3] | 2018 | 1 | Female/67 | Colon ascendens | Medium-poor differentiated adenocarcinoma | Laparoscopic surgery | Good |
| Takeda et al[4] | 2018 | 1 | Female/72 | Colon sigmoideum | Moderately differentiated adenocarcinoma | Laparoscopic surgery | Good |
| Sasaki et al[5] | 2017 | 1 | Female/75 | Colon ascendens | Moderately differentiated adenocarcinoma | Laparoscopic surgery | Good |
| Yaegashi et al[6] | 2015 | 1 | Female/71 | Colon sigmoideum | Well differentiated adenocarcinoma | Laparoscopic surgery | Good |
| Ito et al[7] | 2015 | 2 | Female/53; Male/60 | Rectum Ascending colon cancer | Moderately differentiated adenocarcinoma | Laparoscopic surgery | Good |
| Hirano et al[8] | 2015 | 1 | Male/87 | Carcinoma of the cecum | Moderately differentiated adenocarcinoma | Laparoscopic surgery | Good |
| Sumi et al[9] | 2013 | 1 | Male/83 | Carcinoma of the descending colon | Moderately differentiated adenocarcinoma | Laparoscopic surgery | Good |
| Kim et al[10] | 2011 | 1 | Male/63; Female/71 | Colon cancer of the hepatic flexure | Moderately differentiated adenocarcinoma | Laparoscopic surgery | Good |
| Han et al[11] | 2011 | 1 | Male/63 | Ascending colon cancer | Moderately differentiated adenocarcinoma | Laparoscopic surgery | Good |
| Fujiwara et al[12] | 2007 | 1 | Female/53 | Ascending colon cancer | Moderately differentiated adenocarcinoma | Laparoscopic surgery | Good |
| Goi et al[13] | 2003 | 1 | Female/72 | Ascending colon cancer | Moderately differentiated adenocarcinoma | Laparoscopic surgery | Good |
| Viscott et al[14] | 2011 | 1 | Female/71 | Rectal carcinoma gastric cancer | Moderately differentiated adenocarcinoma | Laparoscopic surgery | Good |
Visceral transposition can be divided into complete visceral transposition and partial visceral transposition. Patients with complete visceral transposition are known as “mirror people” and are extremely rare[14]. Some patients with visceral transposition often present with other complex malformations. The incidence of visceral transposition varies in different regions. In Japan, the incidence of visceral transposition is 0.125‰ to 0.250‰. Yang et al[15] reported that the incidence rate was 0.005‰ to 0.010‰ in China. Several reports of the combination of a malignant tumor and SIT, such as cancer of the liver, stomach, lung, and colon, have been described. Only 2 cases of laparoscopic-assisted resection of CRC have been reported in China[2,3]. The patient described here had sigmoid colon cancer and underwent laparoscopic radical surgery and postoperative intraperitoneal hyperthermic perfusion chemotherapy. The procedure was uneventful, and no tumor recurrence was found after 18 mo of follow-up.
To date, the mechanism of visceral translocation is still unclear, and some scholars believe that it is related to fetal ectopic and chromosomal abnormalities during embryonic development[16]. Whether internal visceral translocation is related to tumor onset is still inconclusive. Studies have shown that there may be a correlation between internal visceral translocation and tumor onset; however, further research is needed[17]. Due to the different pathological types and tumor sites, the clinical manifestations of patients vary, especially in patients with visceral transposition, which is prone to misdiagnosis. Therefore, comprehensive examinations should be completed, such as gastrointestinal endoscopy, computed tomography, and revascularization.
As internal visceral transposition is often accompanied by congenital anatomic abnormalities, surgery can be challenging. The main difficulty is distinguishing the blood vessels. In this case, the main branch vessels supplying the intestine were clearly distinguished by revascularization before surgery, which provided a guarantee for a smooth surgical procedure. In addition, it is necessary to consider the handedness of the surgeon to determine the position of the device, operator, and trocars. Oms and other researchers have found that laparoscopic techniques in visceral transposition patients are more difficult for right-handed surgeons, and are more advantageous for left-handed surgeons[18]. The same effect can be achieved by changing the position of the operator during surgery[6].
For the diagnosis and treatment of patients with visceral transposition combined with gastrointestinal cancer, the possibility of visceral inversion should always be considered. The presence of cardiopulmonary disease should be eliminated to ensure a smooth surgical procedure. Relevant imaging examinations should be improved, and if necessary, revascularization should be performed to determine whether there are obvious vascular variations. An understanding of the anatomical location and variation involved in the operation is essential, and research on the surgical approach and possible problems during surgery should be conducted. Compared with traditional laparotomy, laparoscopic techniques have minimally invasive benefits for patients while also presenting challenges. With the continuous development of technology, there will be a further understanding of the diagnosis and treatment of patients with visceral transposition, especially those with tumor diseases. In addition, because patients with stage T4 are prone to postoperative peritoneal metastasis, hyperthermic intraperitoneal chemotherapy and adjuvant chemotherapy were used to prevent tumor peritoneum relapse[19].
CRC and SIT can be diagnosed according to colonoscopy and imaging examination. Radical resection is the most effective method for treating CRC. A clear diagnosis before surgery can reduce the risk of surgery.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mitsui K, Suzuki H S-Editor: Zhang L L-Editor: Wang TQ P-Editor: Wang LL
| 1. | Iwamura T, Shibata N, Haraguchi Y, Hisashi Y, Nishikawa T, Yamada H, Hayashi T, Toyoda K. Synchronous double cancer of the stomach and rectum with situs inversus totalis and polysplenia syndrome. J Clin Gastroenterol. 2001;33:148-153. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 47] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Fang JF, Wei B, Zheng ZH, Lei PR, Wei HB. Laparoscopic surgery for low visceral transposition of rectal cancer. Zhonghua Weichang Waike Zazhi. 2014;22:830-831. [DOI] [Cited in This Article: ] |
| 3. | Xu ZF, Li JJ, Zhang BG. Diagnosis and treatment of complete visceral transposition combined with intestinal tumors and literature review. Zhonghua Zhenduanxue Dianzi Zazhi. 2018;23:61-64. [DOI] [Cited in This Article: ] |
| 4. | Takeda T, Haraguchi N, Yamaguchi A, Uemura M, Miyake M, Miyazaki M, Ikeda M, Sekimoto M. Laparoscopic sigmoidectomy in a case of sigmoid colon cancer with situs inversus totalis. Asian J Endosc Surg. 2019;12:111-113. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Sasaki K, Nozawa H, Kawai K, Hata K, Kiyomatsu T, Tanaka T, Nishikawa T, Otani K, Kaneko M, Emoto S, Murono K, Watanabe T. Laparoscopic hemicolectomy for a patient with situs inversus totalis: A case report. Int J Surg Case Rep. 2017;41:93-96. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Yaegashi M, Kimura T, Sakamoto T, Sato T, Kawasaki Y, Otsuka K, Wakabayashi G. Laparoscopic sigmoidectomy for a patient with situs inversus totalis: effect of changing operator position. Int Surg. 2015;100:638-642. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Ito T, Saito M, Kobayashi Y, Chika N, Amano K, Matsuzawa T, Ishiguro T, Fukuchi M, Kumagai Y, Ishibashi K, Kumamoto K, Oki S, Mochiki E, Takenoshita S, Ishida H. [Two Cases of Digestive Organ Cancer in Patients with Situs Inversus Treated with Laparoscopic Surgery]. Gan To Kagaku Ryoho. 2015;42:2130-2132. [PubMed] [Cited in This Article: ] |
| 8. | Hirano Y, Hattori M, Douden K, Hashizume Y. Single-incision laparoscopic surgery for colon cancer in patient with situs inversus totalis: report of a case. Indian J Surg. 2015;77:26-28. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Sumi Y, Tomono A, Suzuki S, Kuroda D, Kakeji Y. Laparoscopic hemicolectomy in a patient with situs inversus totalis after open distal gastrectomy. World J Gastrointest Surg. 2013;5:22-26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 12] [Cited by in F6Publishing: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Kim HJ, Choi GS, Park JS, Lim KH, Jang YS, Park SY, Jun SH. Laparoscopic right hemicolectomy with D3 lymph node dissection for a patient with situs inversus totalis: report of a case. Surg Today. 2011;41:1538-1542. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Han HJ, Choi SB, Kim CY, Kim WB, Song TJ, Choi SY. Single-incision multiport laparoscopic cholecystectomy for a patient with situs inversus totalis: report of a case. Surg Today. 2011;41:877-880. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Fujiwara Y, Fukunaga Y, Higashino M, Tanimura S, Takemura M, Tanaka Y, Osugi H. Laparoscopic hemicolectomy in a patient with situs inversus totalis. World J Gastroenterol. 2007;13:5035-5037. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 49] [Cited by in F6Publishing: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Goi T, Kawasaki M, Yamazaki T, Koneri K, Katayama K, Hirose K, Yamaguchi A. Ascending colon cancer with hepatic metastasis and cholecystolithiasis in a patient with situs inversus totalis without any expression of UVRAG mRNA: report of a case. Surg Today. 2003;33:702-706. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 48] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Viscott DS. Situs inversus totalis. Dtsch Med Wochenschr. 2011;176:840-843. [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Yang N, Lu JH, Zhang HB. One case of liver transplantation for visceral total transposition liver cancer and its complications. Dier Junyi Daxue Xuebao. 2008;29:606-608. [DOI] [Cited in This Article: ] |
| 16. | Elbeshry TM, Ghnnam WM. Retrograde (fundus first) Laparoscopic Cholecystectomy in Situs Inversus Totalis. Sultan Qaboos Univ Med J. 2012;12:113-115. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Haruki T, Maeta Y, Nakamura S, Sawata T, Shimizu T, Kishi K, Miyasaka S, Maeta H, Morimoto K, Taniguchi I. Advanced cancer with situs inversus totalis associated with KIF3 complex deficiency: report of two cases. Surg Today. 2010;40:162-166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Oms LM, Badia JM. Laparoscopic cholecystectomy in situs inversus totalis: The importance of being left-handed. Surg Endosc. 2003;17:1859-1861. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 69] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 19. | Klaver CEL, Stam R, Sloothaak DAM, Crezee J, Bemelman WA, Punt CJA, Tanis PJ. Colorectal cancer at high risk of peritoneal metastases: long term outcomes of a pilot study on adjuvant laparoscopic HIPEC and future perspectives. Oncotarget. 2017;8:51200-51209. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |