Copyright
©The Author(s) 2015.
World J Gastrointest Endosc. Jun 25, 2015; 7(7): 675-687
Published online Jun 25, 2015. doi: 10.4253/wjge.v7.i7.675
Published online Jun 25, 2015. doi: 10.4253/wjge.v7.i7.675
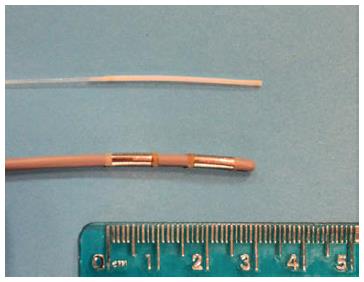
Figure 1 Endoscopic retrograde cholangiopancreatography-directed ablative therapies.
Photodynamic therapy is applied via a laser fiber (above), whereas radiofrequency ablation is delivered using an 8-Fr catheter with two sets of bipolar rings (below).
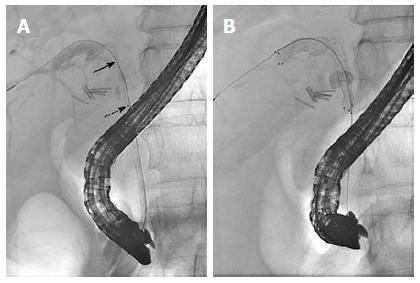
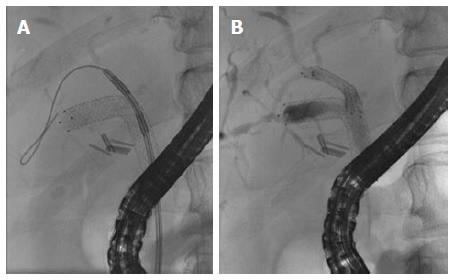
Figure 2 Endoscopic retrograde cholangiopancreatography-directed photodynamic therapy followed by unilateral metal stenting.
A: Fluoroscopic view of a photodynamic therapy laser fiber delivered through a 10-Fr-bougie catheter during endoscopic retrograde cholangiopancreatography. The portion of the fiber that emits laser light is demarcated by the black dot (dashed arrow). The proximal-most tip of the fiber is not visible fluoroscopically (solid arrow) but is located near the biliary confluence; B: An 8 mm x 6 cm uncovered self-expandable metal stent was placed across a malignant stricture that involved the right hepatic duct and common hepatic duct.
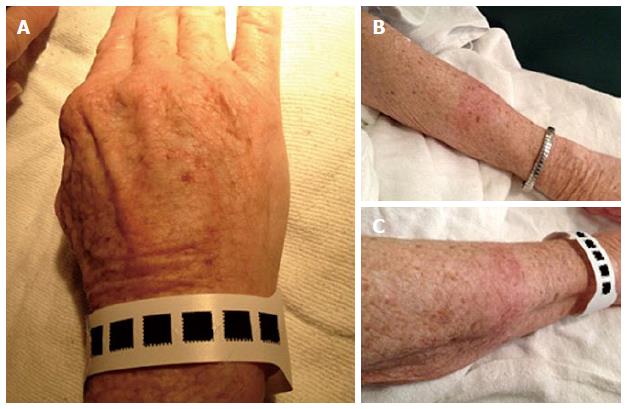
Figure 3 Photosensitivity following photodynamic therapy.
A patient with unresectable cholangiocarcinoma was treated with photodynamic therapy. After 4 wk, a test dose of 10 min of exposure to direct sunlight on small areas of uncovered skin resulted in moderate burns on hands (A) and forearms (B, C). Two additional weeks of avoidance to even indirect sunlight was required.
Figure 4 Endoscopic view of a radiofrequency ablation catheter being inserted into the bile duct by using a duodenoscope.
A biliary sphincterotomy had been performed during a prior endoscopic retrograde cholangiopancreatography procedure in this patient with an unresectable cholangiocarcinoma to enable easier access to the bile duct. Note: this is not a depiction of radiofrequency ablation (RFA) actively being performed, as RFA is not typically applied with the bipolar coils exposed in the duodenal lumen, in order to avoid thermal injury to the duodenal wall.
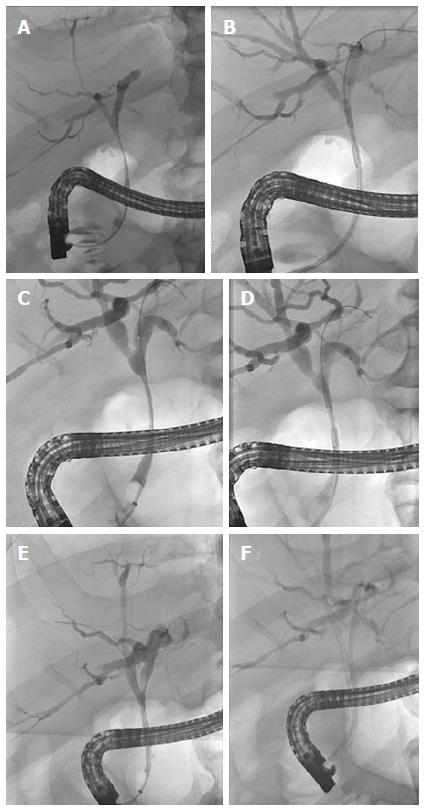
Figure 5 Effect of repeated endoscopic retrograde cholangiopancreatography-directed radiofrequency ablation on a malignant extrahepatic biliary stricture in a patient with unresectable cholangiocarcinoma.
A long perihilar stricture is seen involving the extrahepatic duct (A) in a patient who had exploratory laparotomy that showed locally advanced and unresectable Bismuth I cholangiocarcinoma. A cholecystectomy had been performed at the time of laparotomy. Endoscopic retrograde cholangiopancreatography (ERCP)-directed radiofrequency ablation (RFA) was applied to this malignant stricture (B) followed by biliary stenting (not shown). Following two rounds of RFA done at about 3 mo intervals, a third ERCP showed moderate improvement in the stricture’s diameter (C). Repeat ERCP-directed RFA was performed (D). After 4 rounds of RFA therapy, an ERCP 1 year later showed marked improvement of the extrahepatic bile duct with no high-grade stricture seen (E), and RFA was not repeated during this procedure. A 10-Fr plastic stent was placed into the right hepatic duct and a 7-Fr plastic stent was placed into the left hepatic duct for more durable biliary drainage (F), as this was an otherwise healthy patient with excellent functional status who would likely outlive metal stenting. While patients with Bismuth I cholangiocarcinoma often do well with a single extrahepatic biliary stent, this patient had previously had premature stent failure and cholangitis with a single plastic stent, thus two biliary stents were required.
Figure 6 A patient with unresectable cholangiocarcinoma was previously treated with photodynamic therapy followed by placement of an uncovered metal stent (see Figure 2).
For persistent symptomatic biliary obstruction due to undrained segments in the right liver, a wire was passed into the previously undrained segments which allowed for 6-Fr bougie dilation followed by 4-mm balloon dilation across the lattices of the existing large-cell uncovered self-expandable metal stent (SEMS) (not shown). After dilation, the 8-Fr radiofrequency ablation (RFA) catheter was deployed over the wire and through the SEMS, and RFA was applied to a malignant stricture that was obstructing drainage (A). Lastly an 8-mm uncovered SEMS was deployed through the previously placed 8-mm uncovered SEMS (B) enabling durable drainage of more of the right liver.
- Citation: Uppal DS, Wang AY. Advances in endoscopic retrograde cholangiopancreatography for the treatment of cholangiocarcinoma. World J Gastrointest Endosc 2015; 7(7): 675-687
- URL: https://www.wjgnet.com/1948-5190/full/v7/i7/675.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i7.675