Copyright
©The Author(s) 2015.
World J Gastrointest Endosc. Apr 16, 2015; 7(4): 295-307
Published online Apr 16, 2015. doi: 10.4253/wjge.v7.i4.295
Published online Apr 16, 2015. doi: 10.4253/wjge.v7.i4.295
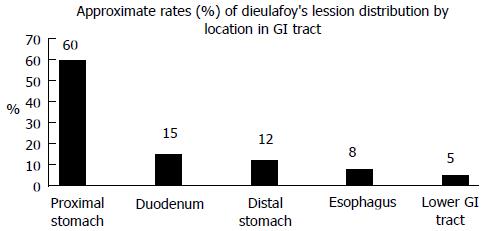
Figure 1 Segmental distribution of Dieulafoy’s lesion within the gastrointestinal tract in patients presenting with acute gastrointestinal bleeding.
GI: Gastrointestinal.
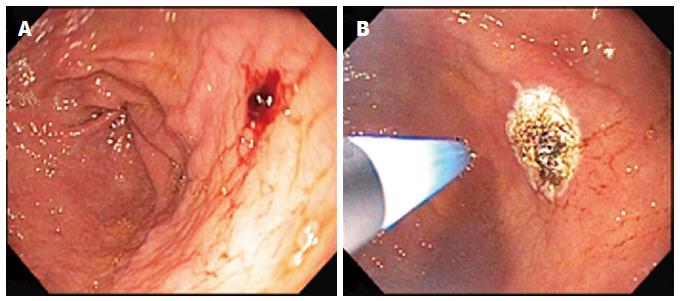
Figure 2 An 86-year-old woman who had undergone two esophagogastroduodenoscopies in the prior 2 years for 2 episodes of acute upper gastrointestinal bleeding that had not revealed any upper gastrointestinal lesions, presented with acute onset of melena and an acute hemoglobin level decline from 11.
0 g/dL to 8.6 g/dL. Esophagogastroduodenoscopy revealed an actively oozing, darkly red, 6-8 mm wide, raised, lesion without surrounding erosions or ulceration that was actively oozing along the greater curvature of the gastric body (A), findings characteristic of a Dieulafoy lesion. The lesion was successfully cauterized using 50 watts of argon plasma coagulation at 1 L/min (note probe hovering over cauterized lesion in (B) with cessation of active oozing. The patient was discharged four days later with no evidence of recurrent bleeding during the hospitalization and no further gastrointestinal bleeding during 4 mo of follow-up.
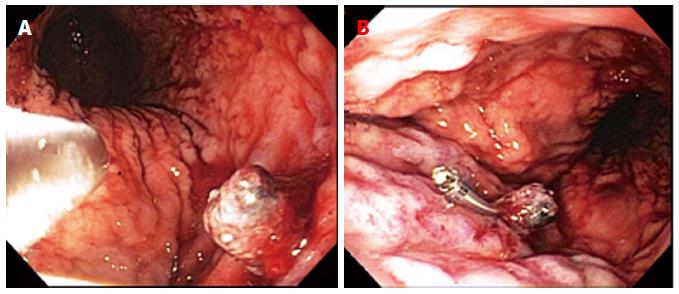
Figure 3 An 88-year-old woman with prior bleeding duodenal ulcer 40 years earlier, and actively administered aspirin, presented with acute onset of hematemesis and melena, with an acute decline in the hemoglobin level from 11.
2 g/dL to 9.2 g/dL. Esophagogastroduodenoscopy revealed an actively oozing, darkly red, 8-10 mm wide, raised, lesion without surrounding erosions or ulceration that was actively oozing in the gastric cardia (A), findings characteristic of a Dieulafoy lesion. The lesion was first injected with 7 mL of epinephrine (1:10000 solution), followed by successful placement of a single hemoclip around the protruding vessel (B), with cessation of active oozing. The patient was discharged three days later with no evidence of recurrent bleeding during the hospitalization.
Figure 4 An 81-year-old woman presented with nausea, coffee-ground emesis, and dizziness.
She underwent urgent esophagogastroduodenoscopy (EGD), despite a normal initial hemoglobin level of 13.0 g/dL, because of the hematemesis. EGD revealed a small blood clot, overlying a lesion without surrounding ulceration, located in proximal gastric body, which was slowly oozing red blood (A). After detachment of the blood clot with irrigation, a raised, darkly red, blood vessel was visualized consistent with a Dieulafoy lesion (B). The lesion was treated with 4 mL of 1:10000 solution of epinephrine and thermocoagulated via heater probe 5 pulses of 30 Joules/pulse without post-procedural bleeding (C). Patient remained stable after the EGD with no further bleeding and she was discharged 3 d later.
- Citation: Nojkov B, Cappell MS. Gastrointestinal bleeding from Dieulafoy’s lesion: Clinical presentation, endoscopic findings, and endoscopic therapy. World J Gastrointest Endosc 2015; 7(4): 295-307
- URL: https://www.wjgnet.com/1948-5190/full/v7/i4/295.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i4.295