Copyright
©The Author(s) 2015.
World J Gastrointest Endosc. Oct 25, 2015; 7(15): 1170-1180
Published online Oct 25, 2015. doi: 10.4253/wjge.v7.i15.1170
Published online Oct 25, 2015. doi: 10.4253/wjge.v7.i15.1170
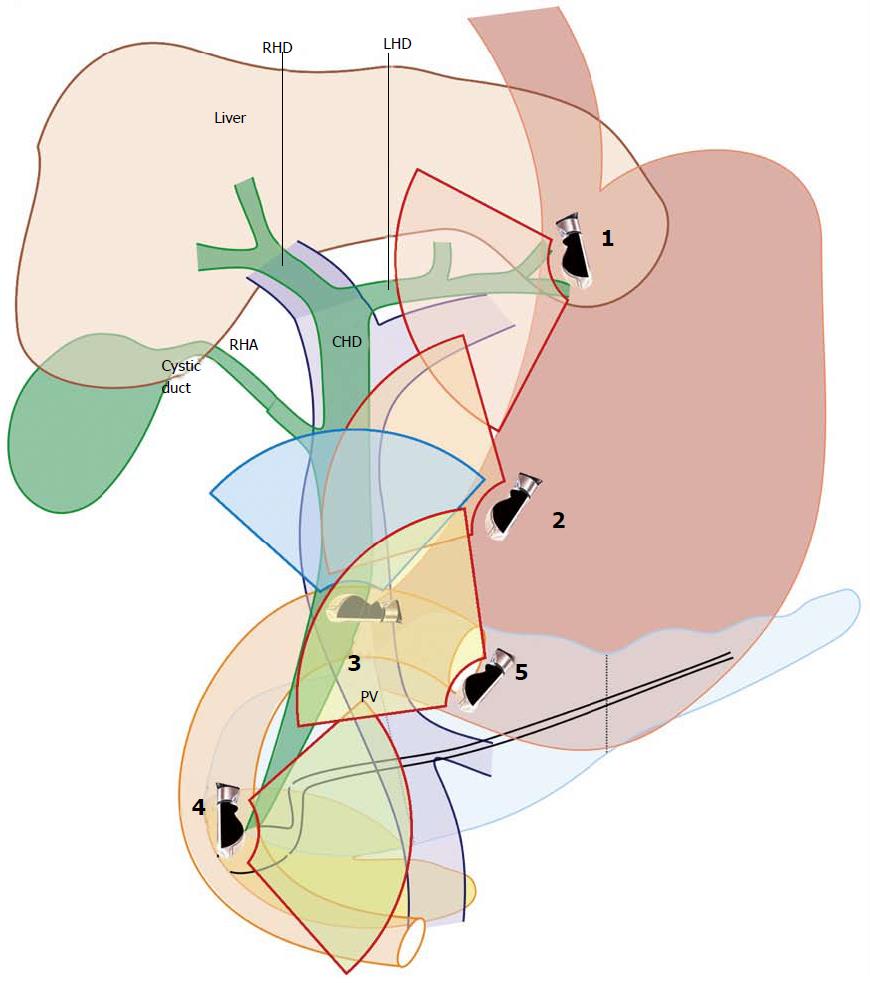
Figure 1 Five positions of Common bile duct imaging by endoscopic ultrasound are shown.
CHD: Common hepatic duct; RHA: Right hepatic artery; RHD: Right hepatic duct; LHD: Left Hepatic duct.
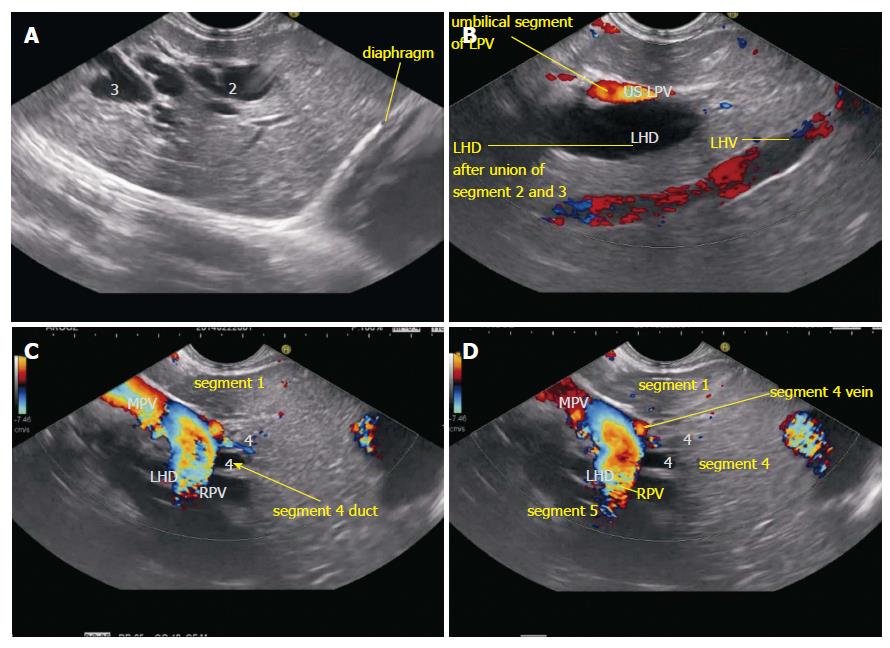
Figure 2 Segmental ducts as seen on endoscopic ultrasound.
A: The dilated ducts of segment 2 and 3 ducts are seen in an open position to left; B: On clockwise rotation the segment 2 and 3 ducts fuse together in front of umbilical part of left portal vein. The left hepatic vein is also identified going from 2 o’clock position to 7 o’clock position; C: On further clockwise rotation the fused part of segment 2 and 3 ducts is joined by segment 4 duct from the cranial aspect (arrow) in front of the transverse segment of left portal vein; D: On further clockwise rotation the right portal vein is seen joining the left portal vein and the liver segment lying below the plane of right portal vein belongs to segment 5. RPV: Right portal vein; LPV: Left portal vein; LHD: Left hepatic duct; LHV: Left hepatic vein.
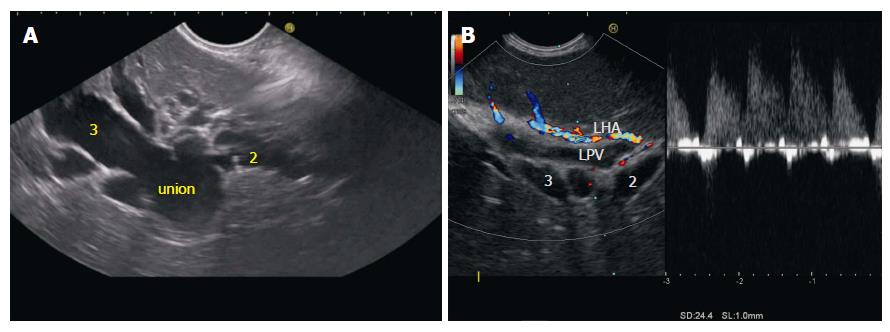
Figure 3 Union of segmental ducts.
A: Segment 2 is identified as duct coming from cranial part of liver segment and segment 3 duct is identified as duct coming from caudal part of liver segment; B: Sometimes the ducts are not dilated and in such situation the tributaries of left portal vein can be identified after application of color doppler and followed to the union and formation of umbilical part of portal vein. LPV: Left portal vein; LHA: Left hepatic artery.
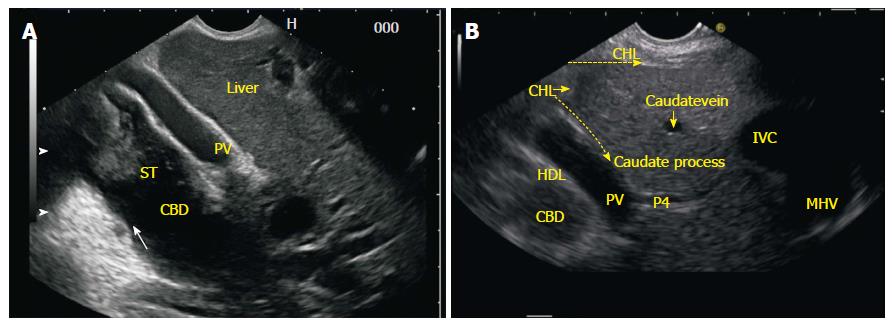
Figure 4 Common bile duct as seen from the gastroesophageal junction.
A: A clockwise rotation moves the axis of imaging from an anterior position in stomach to a lateral position where the liver hilum is placed and follows the segmental duct towards the confluence of both the right and left hepatic ducts; B: In this figure the two limbs of GHL are seen. One of the limb runs on the under surface of liver and the other limb goes in the area between abdominal part of esophagus and liver. As the rotation is executed the presence of hyperchaotic GHL between esophagus and liver and the hepatoduodenal ligament near the liver hilum may interfere with imaging of part of the left or right hepatic ducts near the confluence. CHD: Common hepatic duct; IVC: Inferior venacava; HDL: Hepatoduodenal ligament; IVC: Inferior venacava; GHL: Gastrohepatic ligament.
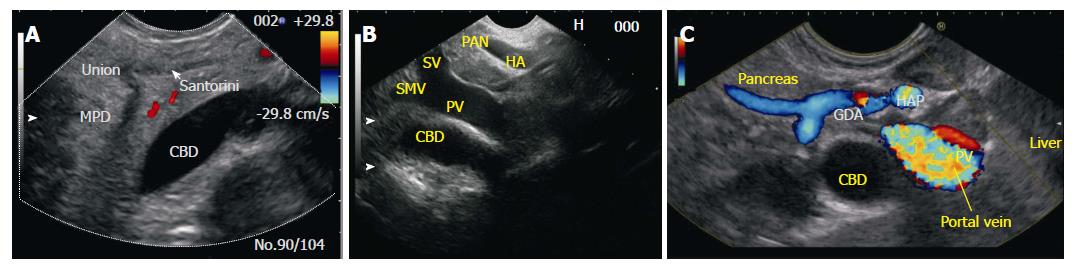
Figure 5 Following down from upper 1/3.
A: A dilated bile duct can be easily followed down and push of the scope in a forward direction along with slight rotation changes the window of imaging from the liver window to pancreatic window. The parenchyma of head of pancreas provides an excellent window for visualization of dilated CBD. With experience even a non-dilated duct can be easily visualized from this position; B: When the probe comes to lie in fundus of stomach the stack of hepatic artery, portal vein and common bile duct can be seen through the liver window. In this picture the hepatic artery lies closest to the transducer, the portal vein lies on the undersurface of liver and the CBD is seen beyond the portal vein. The portal vein and the bile duct can be followed down towards the pancreas from the liver. The portal vein is followed down as SMV; C: When the probe comes to lie anterior to head of pancreas the stack of gastroduodenal artery, portal vein and bile duct can be seen with the help of the pancreatic window. CBD: Common bile duct; SV: Splenic vein; PV: Portal vein; HA: Hepatic artery; MPD: Main pancreatic duct; SMV: Superior mesenteric vein.
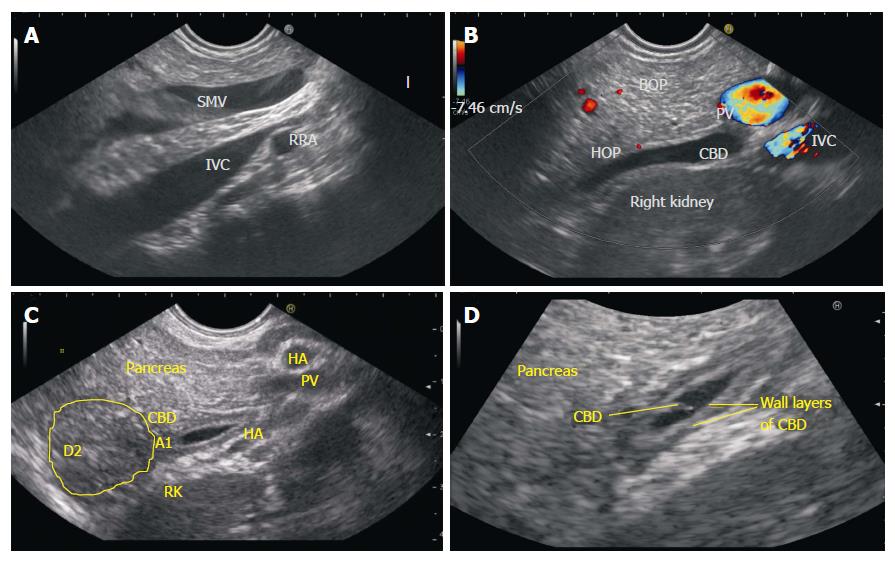
Figure 6 Lower Common bile duct imaging from D2-D3.
A: In the hilum of liver the CBD lies anterior to the portal vein and both CBD and portal vein are positioned anterior to inferior vena cava. As the CBD is followed down towards ampulla the IVC remains goes posterior to head of pancreas whereas the SMV (followed down as a continuation of portal vein) comes to lie anterior to posterior part of head of pancreas. The CBD occupies the area of posterior part of head of pancreas between the SMV and IVC. This figure shows the typical appearance of SMV lying in front of IVC from stomach. If it is difficult to trace the course of CBD, the IVC, portal vein or superior mesenteric vein can be followed as a vascular home bases for tracing of CBD; B: In this figure the CBD is identified in posterior part of head of pancreas with slight anticlockwise rotation after visualizing the typical appearance of SMV lying in front of IVC; C: Once the Lower 1/3 of CBD is located it can be followed down towards the intrapancreatic part of CBD and zooming can help in imaging of papilla as well as 2nd part of duodenum; D: With selective zooming of bile duct the individual layers of bile duct can be identified. SMV: Superior mesenteric vein; CBD: Common bile duct; IVC: Inferior venacava; HOP: Head of pancreas; BOP: Body of pancreas; PV: Portal vein.
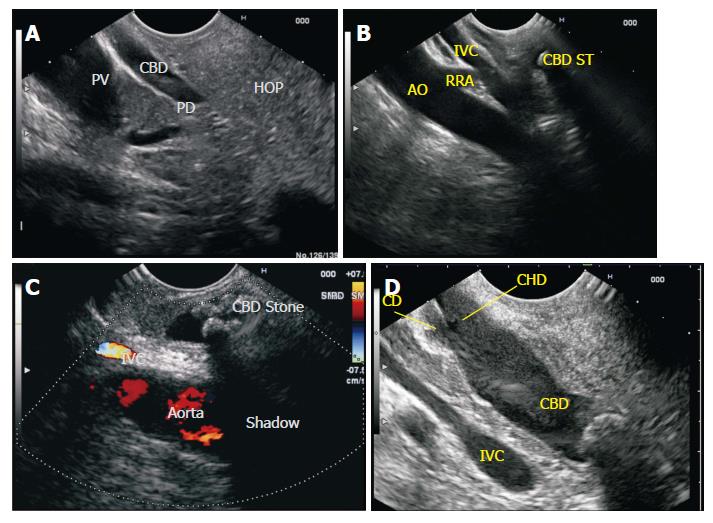
Figure 7 Common bile duct Imaging from duodenal bulb.
A: The portal vein is identified as the home based position from duodenal bulb. From the home base position a limited range of movement of 90 degree to either side traces the entire CBD. A clockwise rotation traces the CBD towards the ampulla and identifies the middle and lower 1/3 of CBD and anticlockwise rotation traces the CBD towards the upper 1/3 and the GB/CD/CHD are also identified near the liver hilum. In this image the CBD is seen in a long axis for a long distance and the PD and portal vein are seen in a long axis for a short distance. This has been called as reverse stack sign; B: In this figure the stack of bile duct (with a stone) aorta and IVC is seen from duodenal bulb. The right renal artery is seen going behind the IVC. The CBD in this case lies in the retropancreatic part anterior to IVC; C: Two stones are seen in the path of acoustic shadow. Although both stones have same acoustic impedance yet it is the second stone, which is causing acoustic shadow. The second stone is surrounded by fluid and the sound waves go through acoustic medium of different acoustic impedance; D: The pyramidal shaped neck of pancreas and pancreatic duct are commonly identified between the probe and portal vein. CBD: Common bile duct; CHD: Common hepatic duct; IVC: Inferior venacava; PV: Portal vein; PD: Pancreatic duct; HOP: Head of pancreas; RRA: Right renal artery; AO: Aorta.
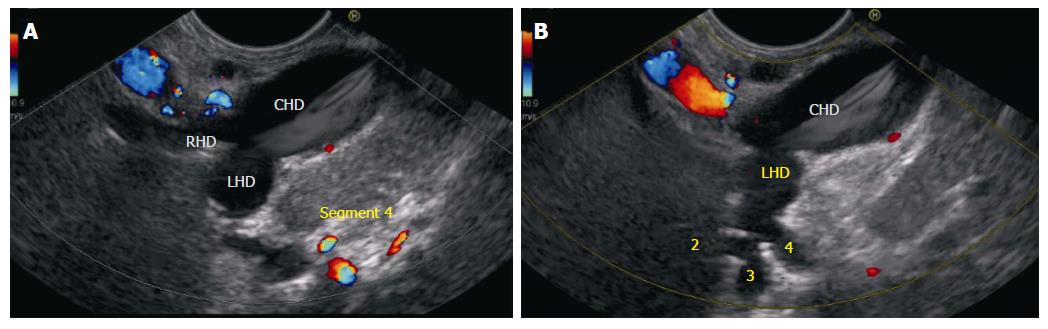
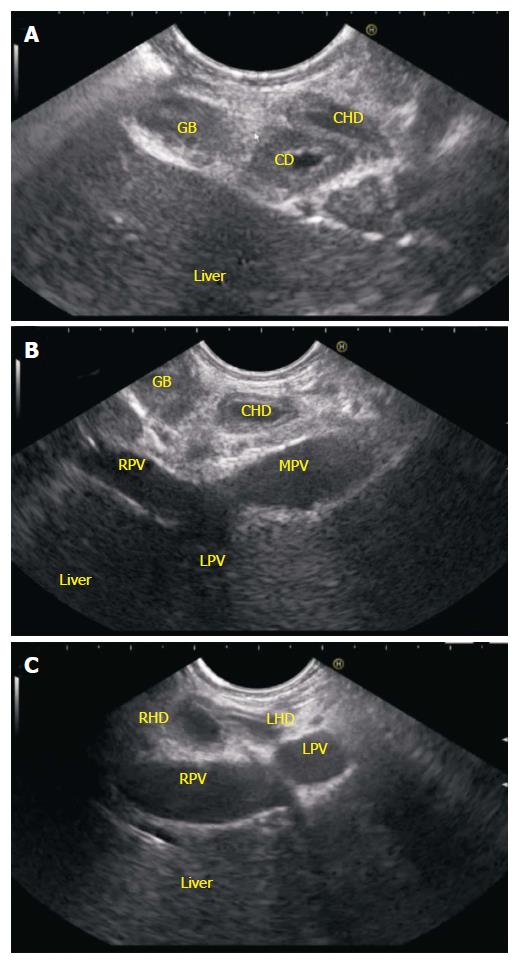
Figure 8 Hilum imaging from duodenal bulb.
A: Imaging from duodenal bulb shows the proximity of CBD to the probe. The middle and upper 1/3rd of CBD and CHD dividing into RHD and LHD are seen. The RHD (average length 0.9 cm) and left hepatic duct (Average length 1.7 cm) unite in the hilar plate, close to the right end of porta in front of right branch of portal vein, to form the CHD; B: In this case it is possible to see the segmental ducts to segment 2, 3 and 4 through upper 1/3rd of CBD. CBD: Common bile duct; CHD: Common hepatic duct; RHD: Right hepatic duct; LHD: Left hepatic duct.
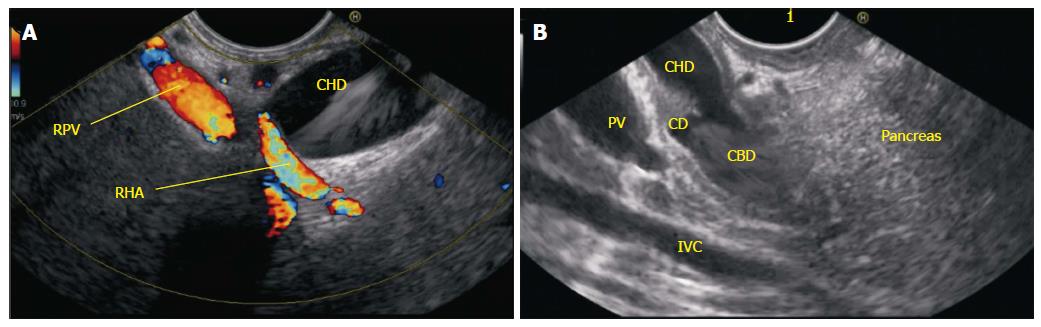
Figure 9 Hepatocystic triangle seen from the duodenal bulb.
A: Imaging from duodenal bulb shows the relationship of right hepatic artery which goes behind the CHD to come and lie in the hepatocystic triangle; B: The bulb provides an opportunity to visualize the mid 1/3rd of CBD and usually provides an excellent window to see the division of CBD into CHD and CD. Most of the time the structure lying farther away from the screen is CD and can be traced towards the gall bladder. CBD: Common bile duct; CHD: Common hepatic duct; CD: Cystic duct; RPV: Right portal vein; RHA: Right hepatic artery; IVC: Inferior venacava.
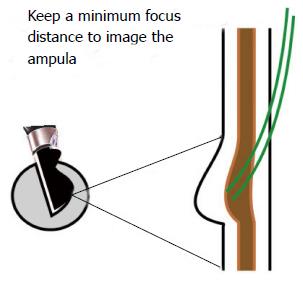
Figure 10 Imaging of Common hepatic duct at papilla can be done after apposition of transducer with the papilla, which is the main endoscopic landmark.
It is appreciated as a thickening of the duodenal wall and a rounded 5-layered structure. Good views of papilla require three things: (1) transducer perpendicular to papilla; (2) good water coupling; (3) and motionless duodenum). If a balloon is used only a small amount of water should be filled in balloon to avoid smashing the delicate papilla. The imaging of papilla after instillation of about 50 to 100 mL water keeps the transducer away from papilla, increases the focal distance of imaging of transducer from papilla and places the papilla as well as lower 1/3 of CBD in the optimum focal distance of imaging (usually about 1 cm). CHD: Common hepatic duct.
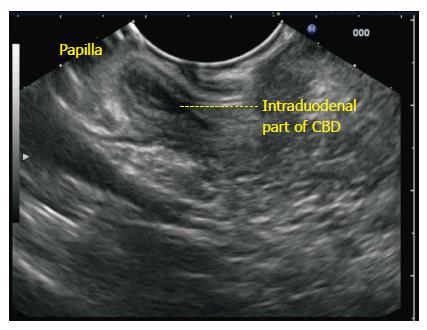
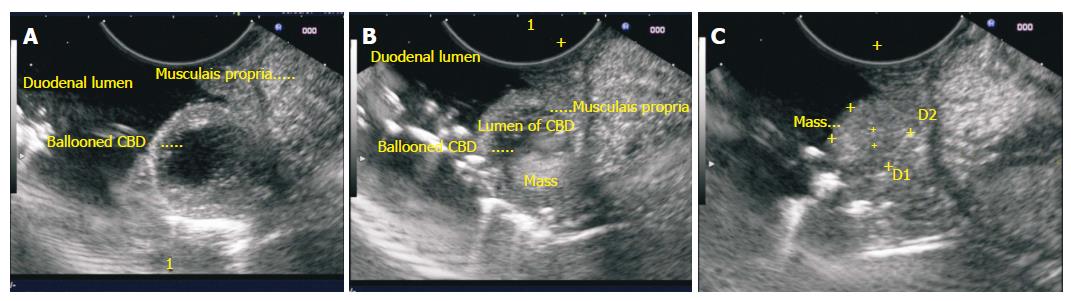
Figure 11 The papilla is the protruding structure in the lumen of the duodenum and is covered on both sides by the muscular layer of the wall.
At the point of the entry of papilla into the duodenal bulb the continuity of muscular layer as a smooth duodenal fall is absent. At the point of union of bile duct and pancreatic duct the dilation of both ducts is named as ampulla. An attempt should be made to trace the intra papillary part of pancreatic duct all the way to the tip of the papilla or into a common ampulla. This can help in identifying the three patterns of opening of the bile duct and pancreatic duct, i.e., common channel, V shaped or separate opening. CBD: Common bile duct.
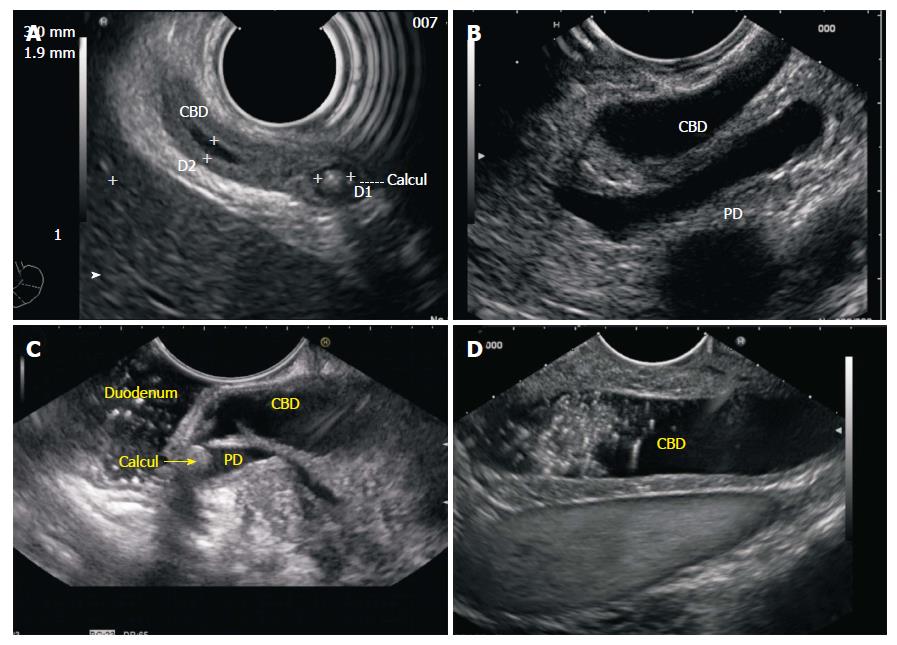
Figure 12 Imaging from 2nd part of duodenum.
A: The intrapapillary part of CBD and the lower 1/3 of CBD is sometimes best visualized with the radial EUS scope as they provide a long axis of imaging of the entire bile duct in a long axis; B: However good view of CBD in a long axis can be also obtained by linear EUS scope. This image shows the dilated CBD and PD in a long axis in a case of periampullary carcinoma; C: The distended CBD may not provide room for good visualization as it comes very close to probe in a pathology involving papilla. This figure shows good view of CBD after instillation of 100 mL water which provides good coupling and also provides adequate focal distance. The stone is impacted in the common channel where it is also obstructing and dilating the pancreatic duct; D: The dilated CBD with sludge is seen from 2nd part of duodenum. On the far side of screen the IVC is also seen beyond the IVC. CHD: Common hepatic duct; EUS: Endoscopic ultrasound; IVC: Inferior venacava; CBD: Common bile duct; PD: Pancreatic duct.
Figure 13 Imaging of common hepatic duct from second part of duodenum.
A: A distended CBD is seen after good water coupling from 2nd part of duodenum but this image does not provide a clue to the diagnosis; B: An Ampulloma is seen within the distended intraduodenal part of bile duct; C: The tumor is seen within the intraduodenal part of CBD but it appears separate from the muscularis propria layer. CBD: Common bile duct.
Figure 14 Hilum imaging from D2.
A: Anticlockwise rotation from the 2nd part of duodenum traces the CBD towards the hilum. The cystic duct is seen taking origin from the aspect away from transducer and the gall bladder is visualized; B: When imaging is done from below upwards the imaging shows the CHD going towards the right portal vein; C: Further anticlockwise rotation towards hilum can show the left and right hepatic duct. The division of CHD into RHD and LHD occurs in front of right branch of portal vein. CBD: Common bile duct; CHD: Common hepatic duct; RHD: Right hepatic duct; LHD: Left hepatic duct; LPV: Left portal vein; RPV: Right portal vein.
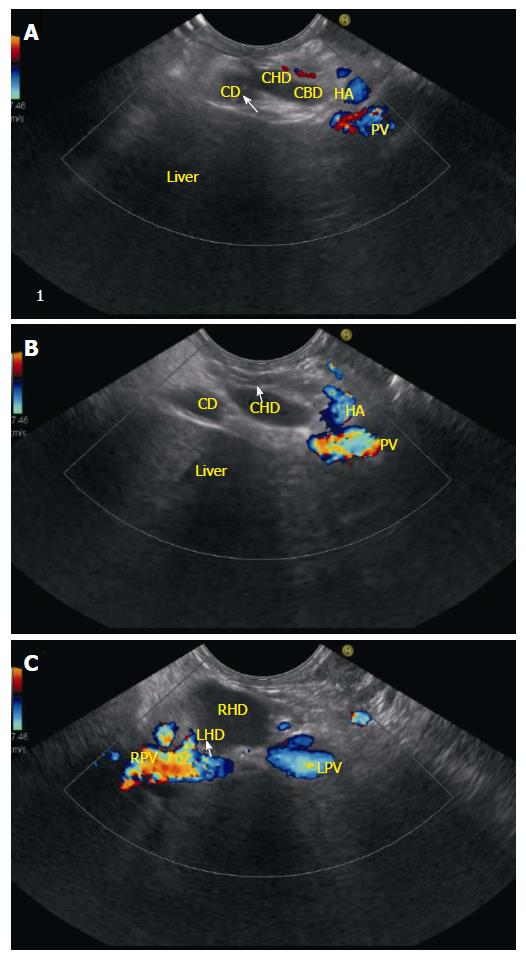
Figure 15 Cystic duct and common hepatic duct imaging.
A and B: The cystic duct terminates at the right wall of the common hepatic duct in 85 to 90% of cases. In this case the CD is seen joining the right aspect of CHD; C: When the CHD is followed up it divides into right and left hepatic duct and this bifurcation generally lies in front of the right branch of the portal vein. As the echoendoscope is rotated counter clockwise the portal vein is followed up to its bifurcation and the RPV is seen on the right side of the screen. CHD: Common hepatic duct; CD: Cystic duct; CBD: Common bile duct; PV: Portal vein; HA: Hepatic artery; RHD: Right hepatic duct; LHD: Left Hepatic duct; LPV: Left portal vein; RPV: Right portal vein.
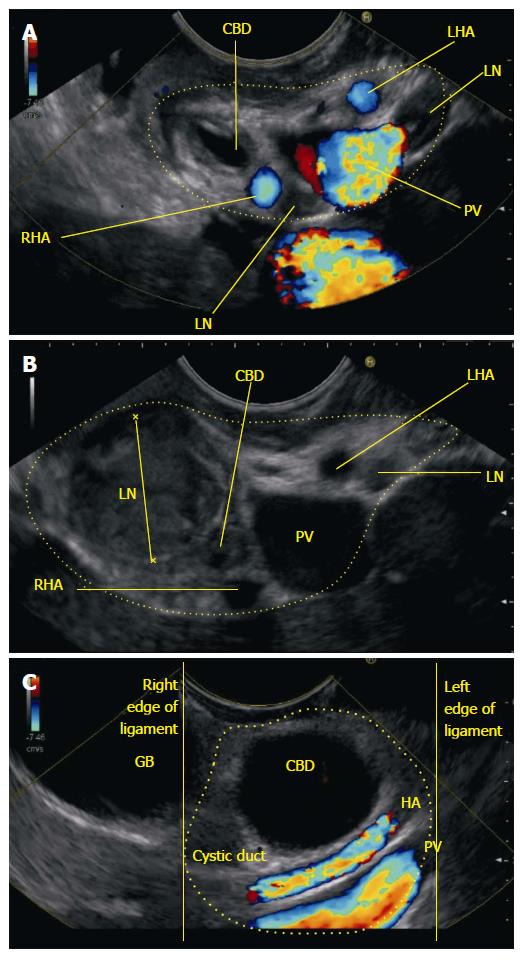
Figure 16 Hepatoduodenal ligament.
A: The anticlockwise rotation takes the probe towards the hilum of liver the bile duct is demonstrated in a transverse axis. The HDL contains the structures of portal triad; B: Further anticlockwise rotation shows an abnormal lymph node within the hepatoduodenal ligament which is causing obstruction of CBD; C: On further anticlockwise rotation the probe moves towards the hilum of liver and the dilated bile duct is demonstrated in a transverse axis along with cystic duct and gall bladder. The portal vein and hepatic artery are demonstrated in long axis. All these structures shown lie in the hepatoduodenal ligament near the hilum except the gallbladder. CBD: Common bile duct; CHD: Common hepatic duct; RHA: Right hepatic artery; LHA: Left hepatic artery; LN: Lymph node; PV: Portal vein; HDL: Hepatoduodenal ligament.
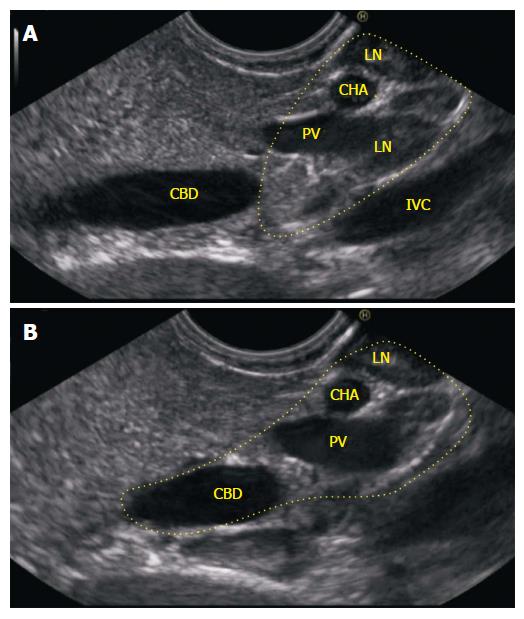
Figure 17 When the scope comes to lie in antrum the splenic vein can be followed towards the portal venous confluence easily.
Once the portal venous confluence is identified a slight anticlockwise torque with push generally identifies the lower 1/3 of CBD in head of pancreas. Once the duct is identified the adjustment of focus, on the far side of screen with adjustment to lower frequency may be required for proper visualization of CBD behind the confluence. CBD: Common bile duct; LN: Lymph node; CHA: Common hepatic artery; PV: Portal vein; LN: Lymph node; IVC: Inferior venacava.
- Citation: Sharma M, Pathak A, Shoukat A, Rameshbabu CS, Ajmera A, Wani ZA, Rai P. Imaging of common bile duct by linear endoscopic ultrasound. World J Gastrointest Endosc 2015; 7(15): 1170-1180
- URL: https://www.wjgnet.com/1948-5190/full/v7/i15/1170.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i15.1170