Copyright
©The Author(s) 2015.
World J Hepatol. Jul 18, 2015; 7(14): 1884-1893
Published online Jul 18, 2015. doi: 10.4254/wjh.v7.i14.1884
Published online Jul 18, 2015. doi: 10.4254/wjh.v7.i14.1884
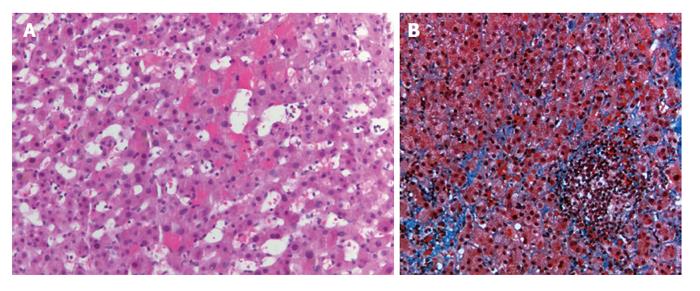
Figure 1 Hemotoxylin-eosin stains of a core liver biopsy from a patient with venous outflow obstruction shows hemorrhage within sinusoidal spaces (A) as well as evidence of sinusoidal fibrosis on a trichrome stain (B).
Figure 2 Flowchart presenting number of treatments and recurrence of hepatic venous obstruction in all patients.
HVOO: Hepatic venous obstruction; PTA: Percutaneous transluminal angioplasty.
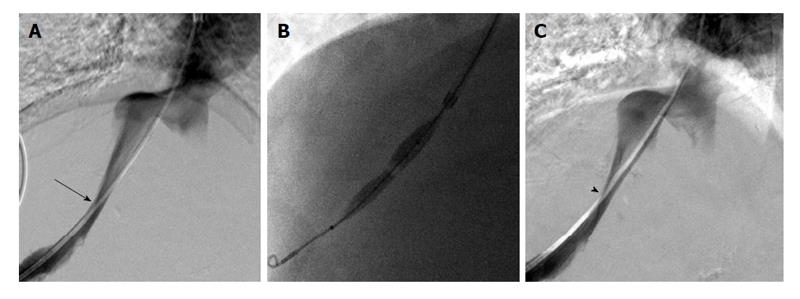
Figure 3 Fifty years old woman with elevated LFTs after liver transplantation and biopsy findings of venous outflow obstruction found to have a right hepatic vein stenosis (A, arrow); following angioplasty with a 10 mm × 4 cm balloon (B), there was decrease in pressure gradient from 8 mmHg to 1 mmHg, though the venographic appearance remained the same (C, arrowhead).
Late biopsy demonstrated no evidence of venous outflow obstruction and the patient was doing well at 1 year follow-up.
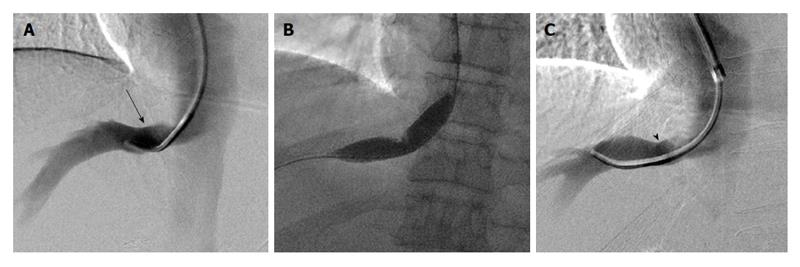
Figure 4 Sixty-six years old man with elevated LFTs after liver transplantation and biopsy consistent with venous outflow obstruction found with right hepatic vein stenosis (A, arrow); following angioplasty with 6, 8, 10, and 12 mm × 4 cm balloons (B), mild improvement was seen in luminal diameter on venography (C, arrowhead).
On late biopsy, the patient had persistent evidence of venous outflow obstruction and repeat angioplasty was performed.
- Citation: Sarwar A, Ahn E, Brennan I, Brook OR, Faintuch S, Malik R, Khwaja K, Ahmed M. Utility of liver biopsy in predicting clinical outcomes after percutaneous angioplasty for hepatic venous obstruction in liver transplant patients. World J Hepatol 2015; 7(14): 1884-1893
- URL: https://www.wjgnet.com/1948-5182/full/v7/i14/1884.htm
- DOI: https://dx.doi.org/10.4254/wjh.v7.i14.1884