Copyright
©The Author(s) 2020.
World J Hepatol. Oct 27, 2020; 12(10): 738-753
Published online Oct 27, 2020. doi: 10.4254/wjh.v12.i10.738
Published online Oct 27, 2020. doi: 10.4254/wjh.v12.i10.738
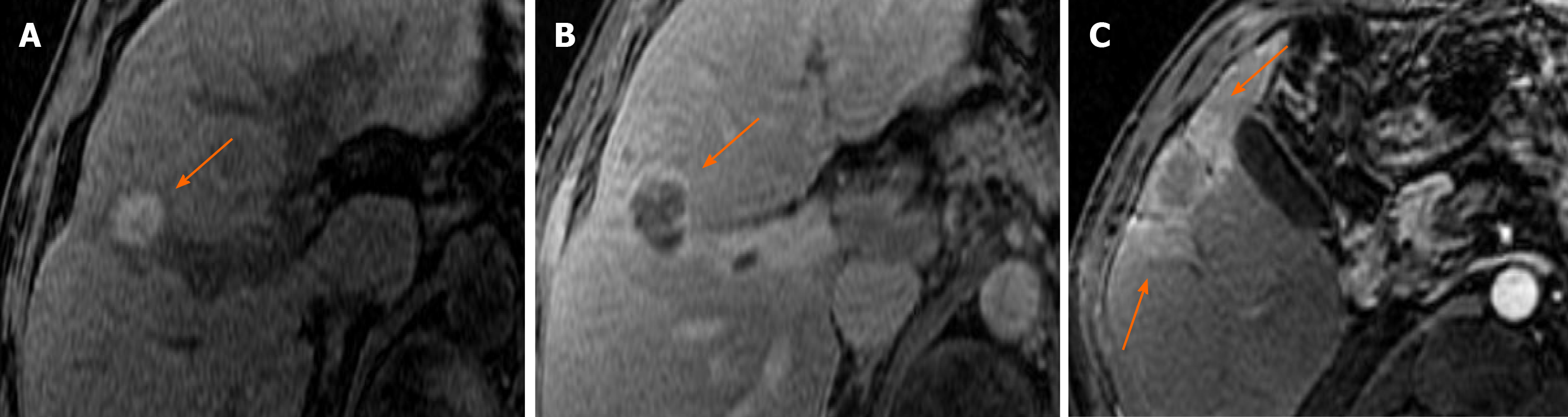
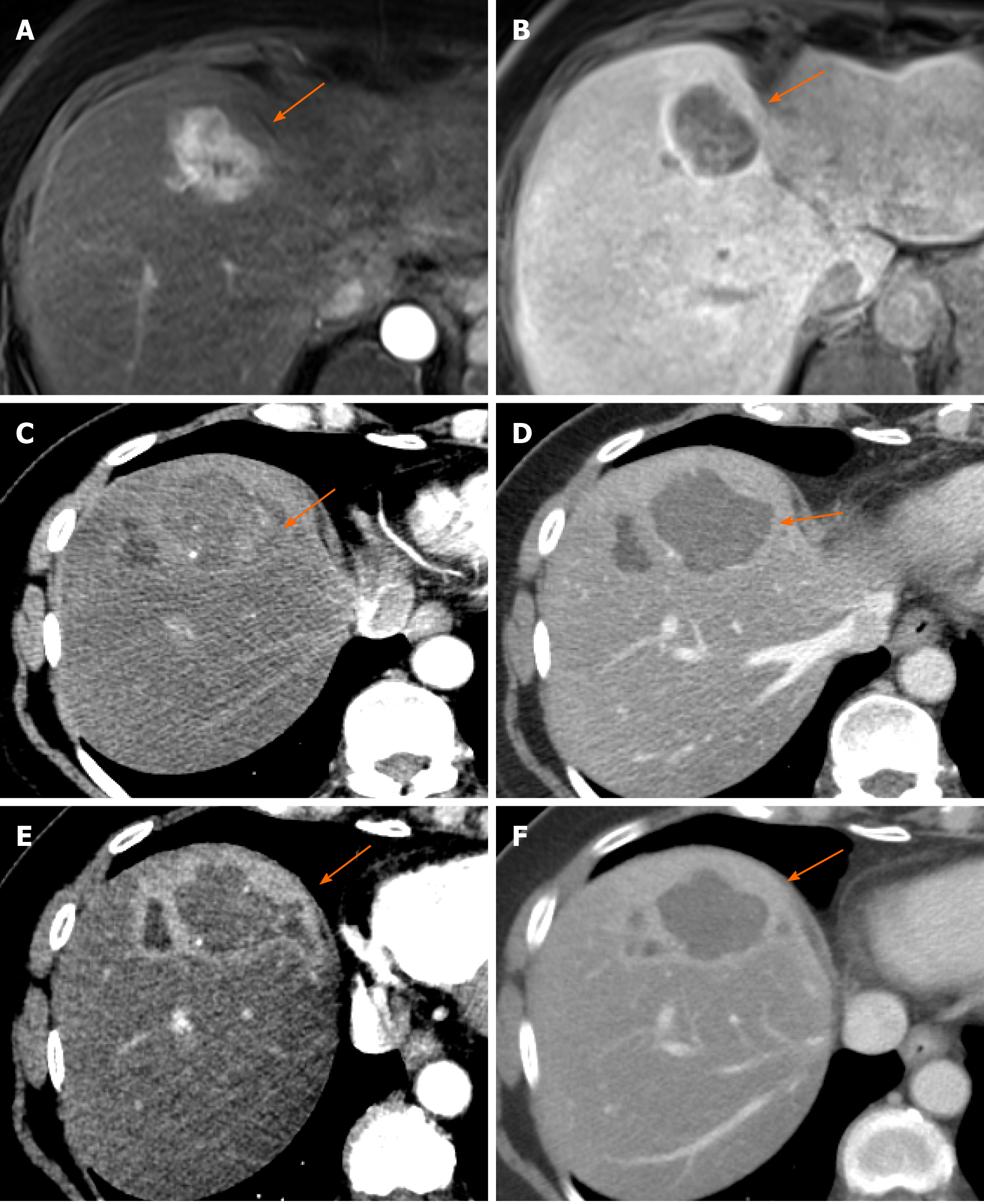
Figure 1 Spectrum of expected post treatment imaging appearances after successful LR TR Nonviable microwave ablation of LR 5 hepatocellular carcinoma in different patients.
A: Hyperintense signal on pre-contrast T1 weighted image, which does not enhance (subtraction not shown); B: Thin continuous smooth rim of enhancement surrounding the ablation zone on portal venous phase of imaging; C: Mild peri-tumoral ill-defined geographic areas of arterial phase hyperenhancement within the parenchyma adjacent to the treatment cavity on arterial phase image, which becomes isoenhancing to the parenchyma on delayed phase of imaging (not shown).
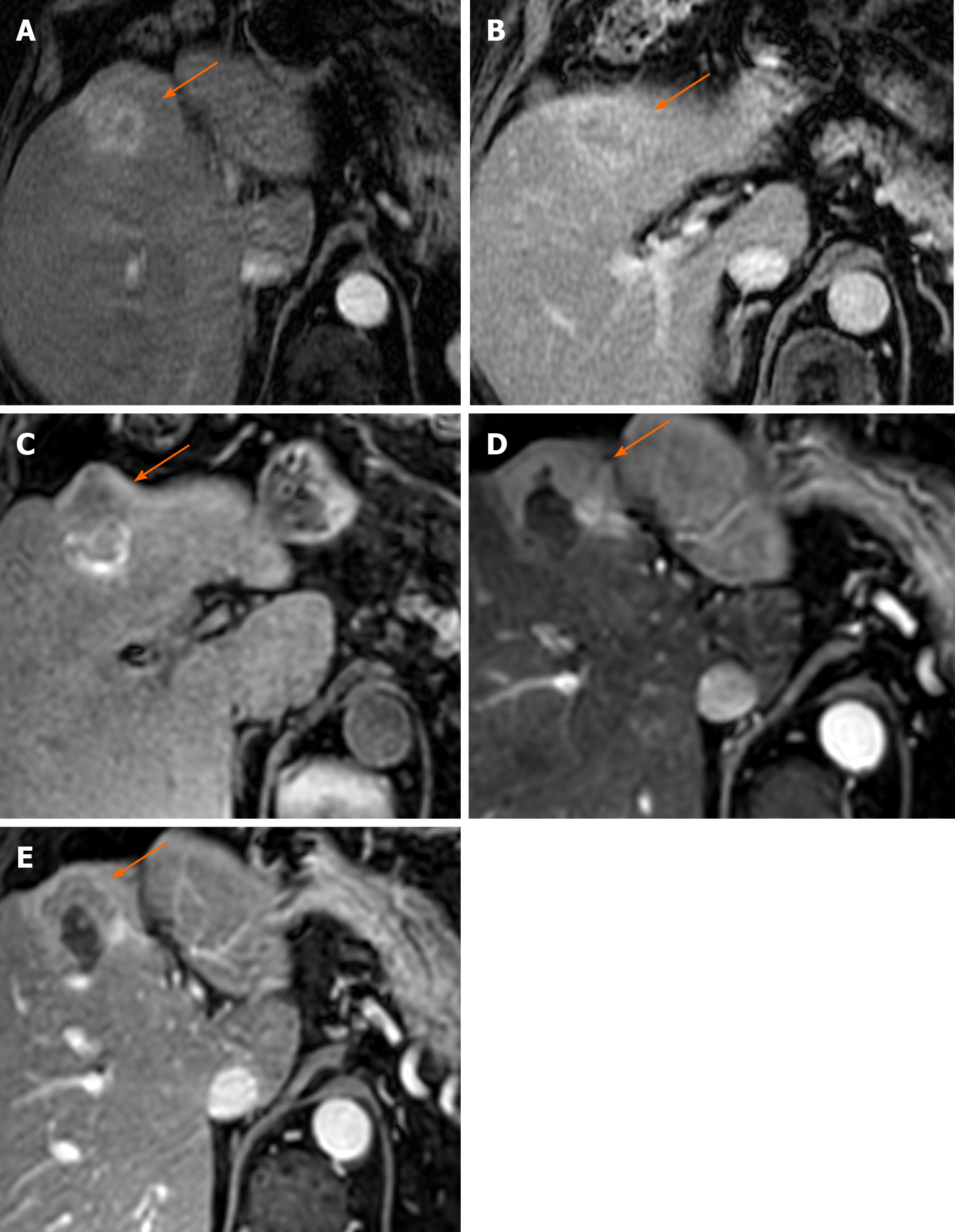
Figure 2 Eighty-three-year old male with nonalcoholic steatohepatitis related cirrhosis presented with a 3.
5 cm mass demonstrating arterial phase hyperenhancement (APHE) (A) and “washout” (B), compatible with an LR-5 hepatocellular carcinoma; C: Pre-contrast T1 images 6 mo post microwave ablation demonstrate a hypointense nodular area along the anterior margin of the ablation cavity, with thick irregular nodular APHE on arterial phase (D) and “washout” and “capsule” on portal venous phase (E), LR-TR Viable.
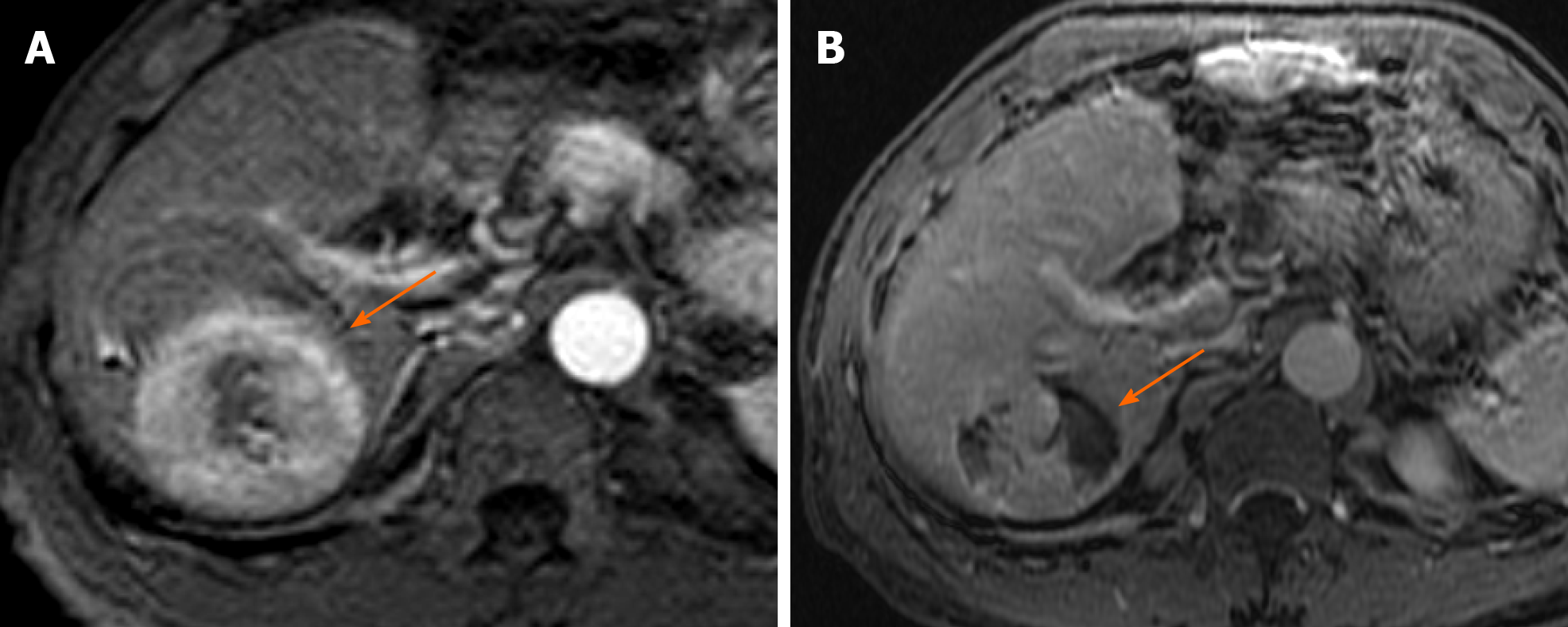
Figure 3 Fifty-four-year old male with hepatitis C virus presents with 5.
4 cm hepatocellular carcinoma in the right lobe of the liver demonstrating arterial phase hyperenhancement on arterial phase of imaging (A), LR 5; 1 mo post-transarterial chemoembolization there is significant residual viable enhancing tumor with areas of necrosis on arterial phase imaging (B), LR-TR Viable.
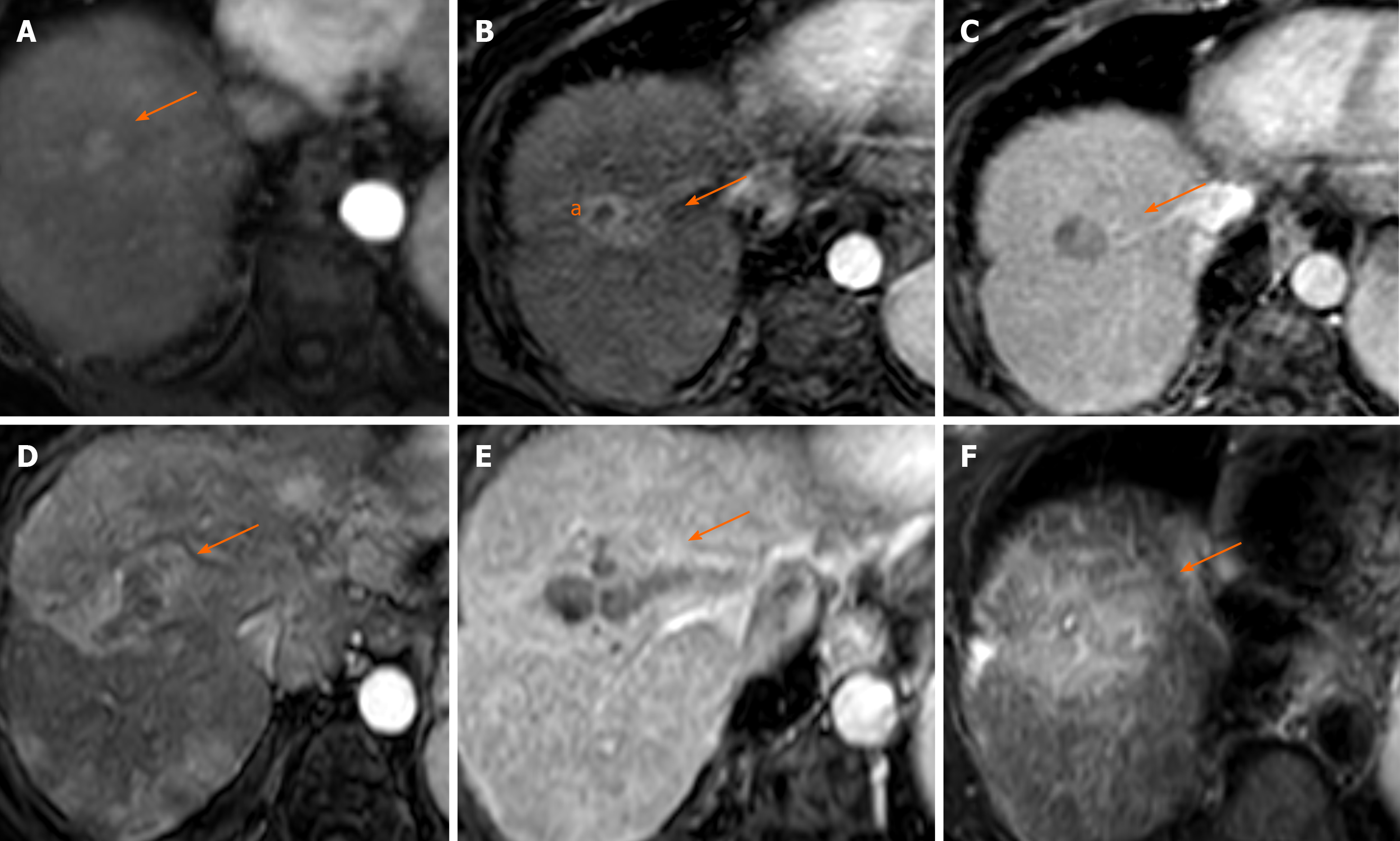
Figure 4 Seventy-three-year old woman with history of nonalcoholic steatohepatitis related cirrhosis presented with 1.
5 cm mass in segment 8 with arterial phase hyperenhancement (APHE) (A) and washout (not shown), LR 5; 1 mo post transarterial chemoembolization (TACE) there is central necrosis with a smooth rim of enhancement (a) (B); however, along the medial edge of the treatment cavity is new ill-defined APHE (arrow) (B) with washout (C), LR TR Viable; 3 mo post re-TACE, there was interval development of infiltrative tumor with APHE on arterial phase (D), “washout” on portal venous phase (E) and T2W hyperintensity (F). In addition, new tumor thrombus was seen in the right portal vein (E), LR TR Viable with tumor in vein.
Figure 5 Sixty-two-year old female with LR 5 hepatocellular carcinoma within segment 4a of the liver, demonstrating arterial phase hyperenhancement (APHE) (A) and “washout” (B); 3 mo post transarterial radioembolization (TARE) there is persistent arterial phase nodular enhancement (arrow) (C) with associated “washout” on portal venous phase (D) within the largely necrotic treatment cavity, LR TR Equivocal; 6 mo post-TARE, the treatment cavity decreases in size and the nodular area of APHE is no longer identified on arterial phase (E) and portal venous phase (F), LR TR Nonviable; geographic APHE in the surrounding parenchyma is compatible with post-radiation changes (E and F).
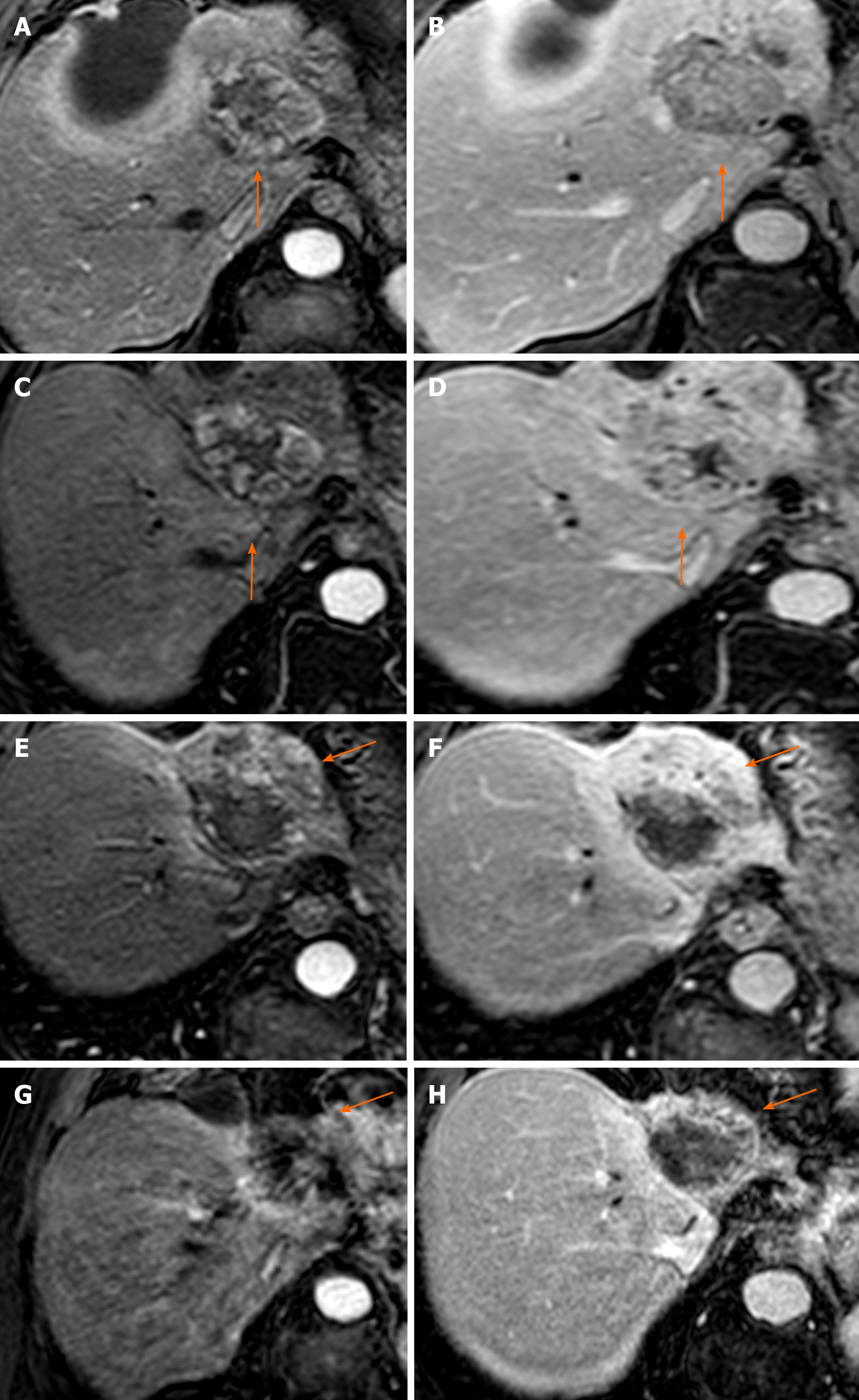
Figure 6 Fifty-eight-year old male presenting 3 mo post transarterial chemoembolization for follow up of a 7.
2 cm LR 5 hepatocellular carcinoma. Persistent thick nodular peripheral arterial phase hyperenhancement (APHE) of the treated tumor (A) with “washout” on portal venous phase (B), LR-TR Viable. This lesion was subsequently treated with stereotactic body radiotherapy (SBRT). Three months post SBRT there is persistent APHE on arterial phase (C) and “washout” on portal venous phase (D), with no change in size, LR-TR Viable or Equivocal. Six months post SBRT, there is decreasing size of the tumor to 6.3 cm with decreasing APHE and increasing necrosis, albeit persistent APHE (E) and “washout” (F), LR-TR Equivocal. Fifteen months post SBRT, further decrease in size to 5.1 cm, now with minimal residual APHE (G) and “washout” (H), LR-TR Nonviable.
- Citation: Aslam A, Do RKG, Kambadakone A, Spieler B, Miller FH, Gabr AM, Charalel RA, Kim CY, Madoff DC, Mendiratta-Lala M. Hepatocellular carcinoma Liver Imaging Reporting and Data Systems treatment response assessment: Lessons learned and future directions. World J Hepatol 2020; 12(10): 738-753
- URL: https://www.wjgnet.com/1948-5182/full/v12/i10/738.htm
- DOI: https://dx.doi.org/10.4254/wjh.v12.i10.738