Copyright
©The Author(s) 2022.
World J Stem Cells. Jul 26, 2022; 14(7): 556-576
Published online Jul 26, 2022. doi: 10.4252/wjsc.v14.i7.556
Published online Jul 26, 2022. doi: 10.4252/wjsc.v14.i7.556
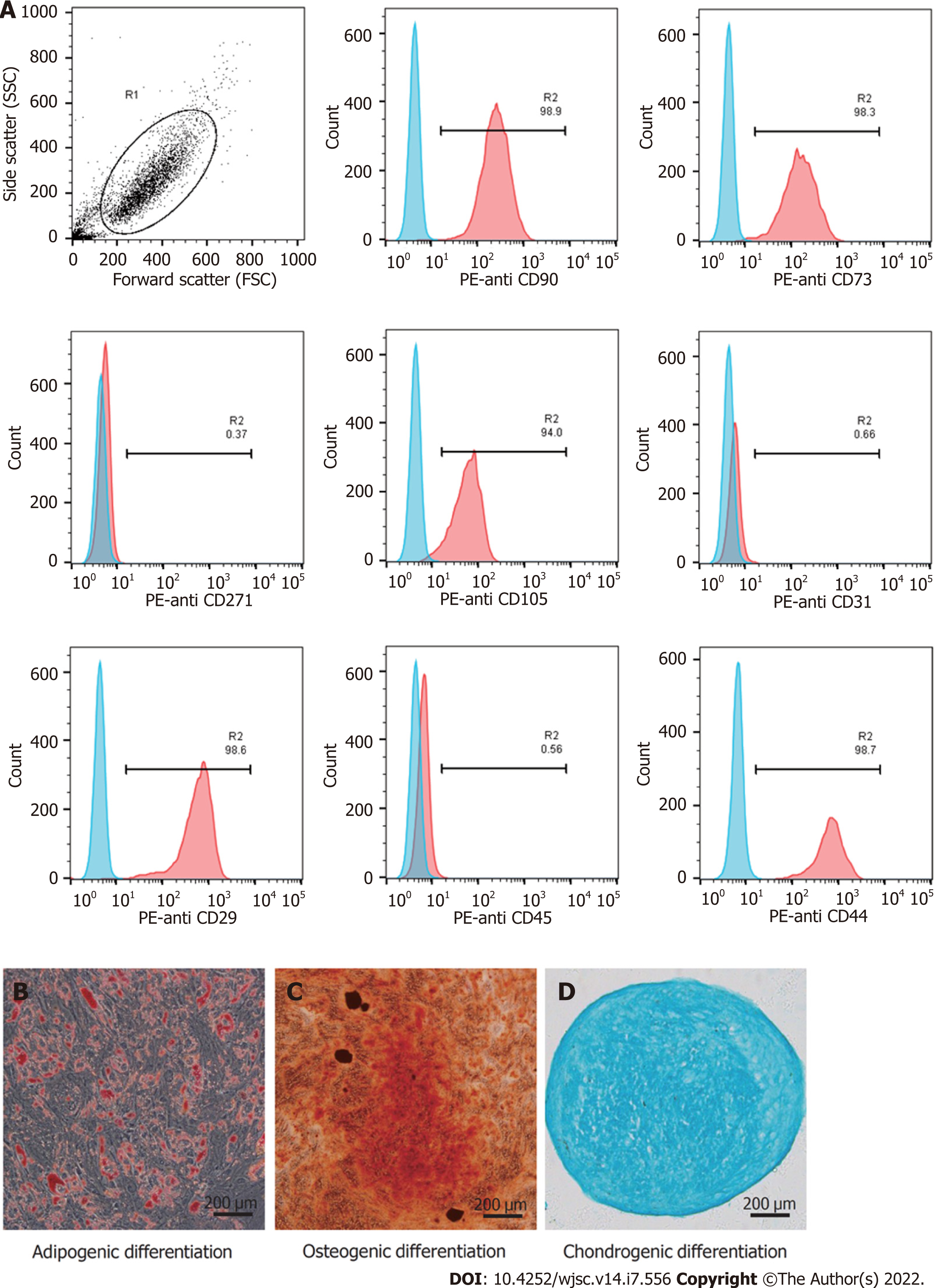
Figure 1 Identification of human umbilical cord-derived mesenchymal stem cells.
A: The human umbilical cord-derived mesenchymal stem cells (hUC-MSCs) showed high expression of CD29, CD44, CD73, CD90, and CD105, and did not express CD31, CD45, and CD271; B–D: hUC-MSCs were positive for Oil Red O, Alizarin red, and Alcian blue staining under the corresponding induction conditions (scale bars = 200 μm).
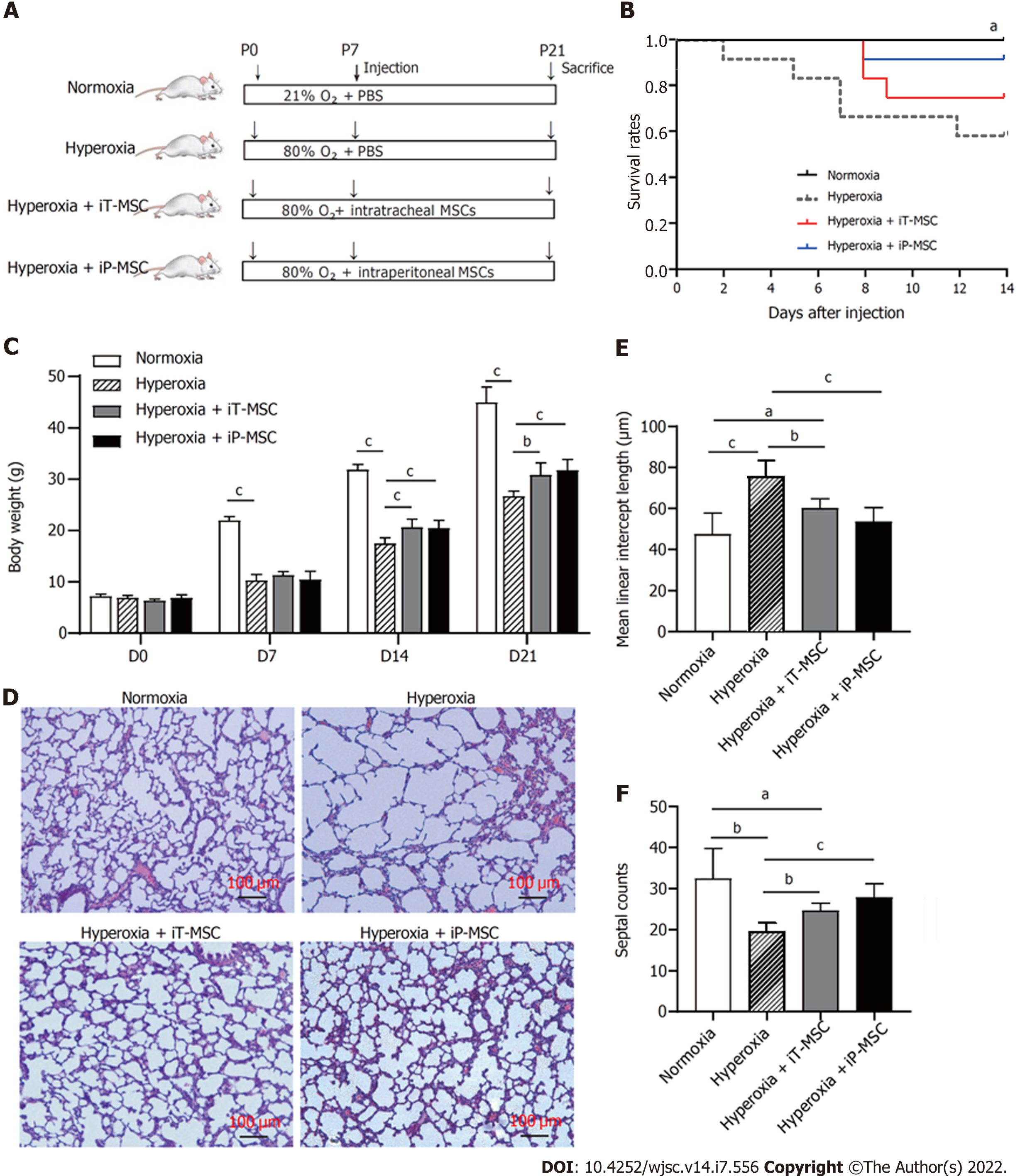
Figure 2 Human umbilical cord-derived mesenchymal stem cells administration increases survival rate and improves lung development.
A: Schematic diagram of the overall experimental design process and grouping; B: Kaplan-Meier survival curves of rat pups treated as indicated; C: Body weight alterations of rat pups treated as indicated; D: Representative images of harvested lung sections stained with hematoxylin and eosin for morphometric analyses (scale bars = 100 μm); E and F: Mean linear intercept and septal counts in lungs treated as indicated (n = 5 for each group, 10 fields/animal). aP < 0.05; bP < 0.01; cP < 0.001. iT: Intratracheal; iP: Intraperitoneal; P: Postnatal day; PBS: Phosphate-buffered saline; MSC: Mesenchymal stem cell.
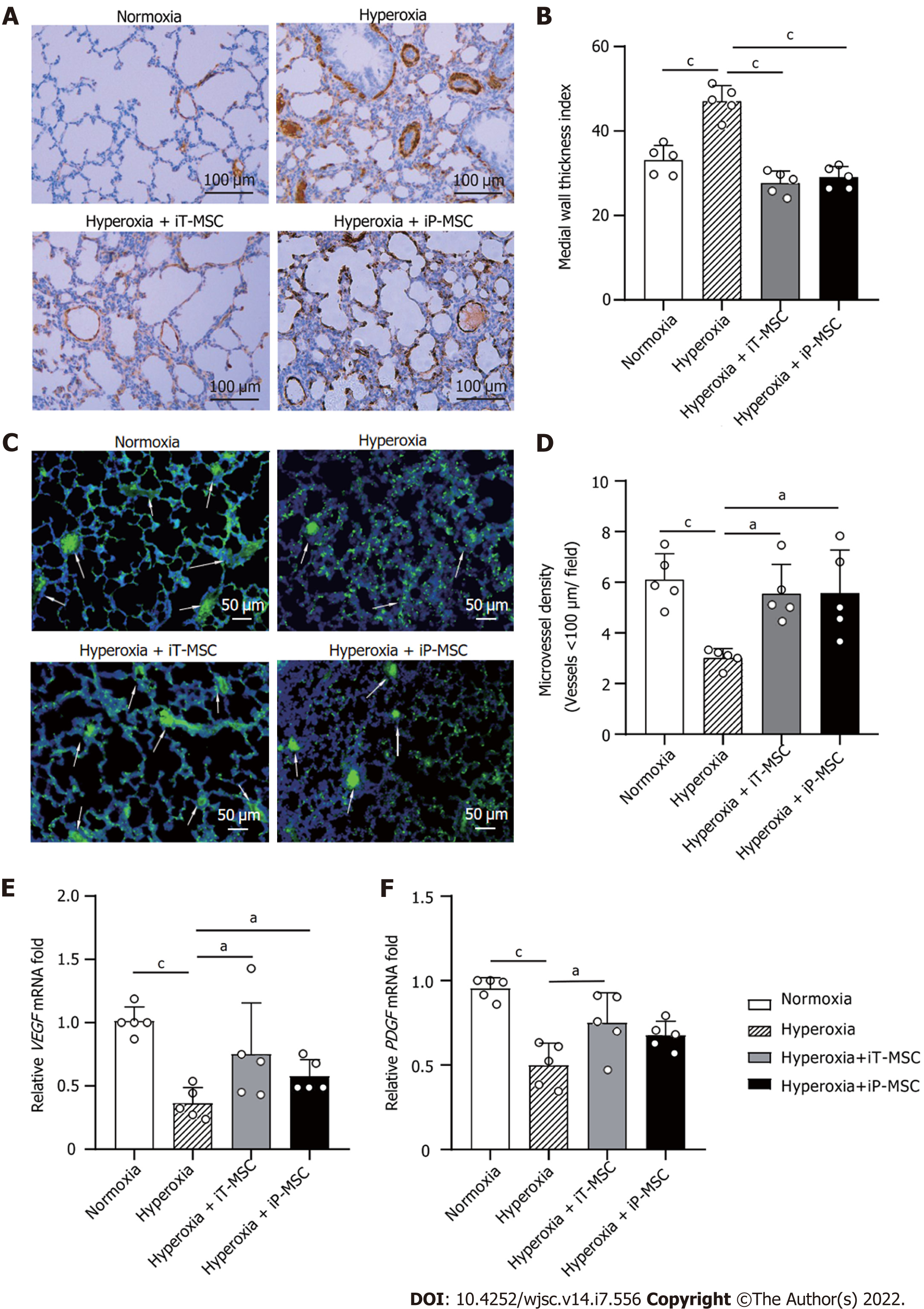
Figure 3 Human umbilical cord-derived mesenchymal stem cells treatment rescues hyperoxia-induced loss of peripheral pulmonary blood vessels and peripheral pulmonary arterial remodeling.
A: Representative photomicrographs of lung sections of rats harvested at postnatal day 21 stained with α smooth muscle actin antibody in normal air or hyperoxia exposure groups, with or without human umbilical cord-derived mesenchymal stem cells administration (scale bars = 100 μm); B and D: Medial thickness index and microvessel density in lungs treated as indicated were calculated to assess hyperoxia-induced peripheral pulmonary vascular remodeling and loss of blood vessels in the peripheral microvasculature (n = 5 for each group, 5 fields/animal); C: Representative lung slides with von Willebrand factor- immunofluorescence staining obtained at 200 × magnification. White arrows highlight stained pulmonary vessels (scale bars = 50 μm); E and F: Vascular endothelial-derived growth factor and platelet-derived growth factor mRNA expression in the lung tissues in the indicated groups. aP < 0.05; bP < 0.01; cP < 0.001. iT: Intratracheal; iP: Intraperitoneal; VEGF: Vascular endothelial-derived growth factor; PDGF: Platelet-derived growth factor; MSC: Mesenchymal stem cell.
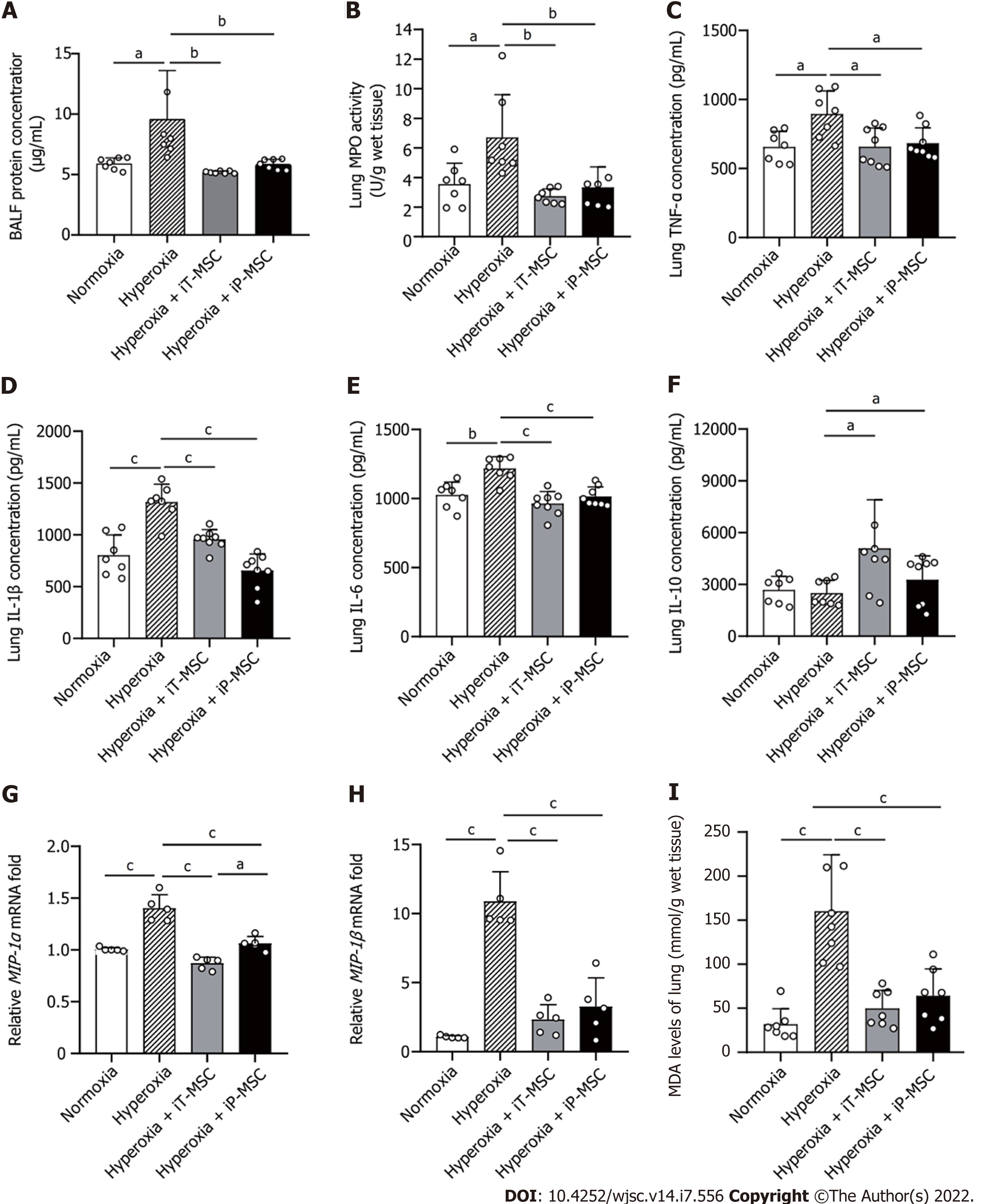
Figure 4 Human umbilical cord-derived mesenchymal stem cells treatment modulates the hyperoxia-induced lung inflammation and oxidative stress.
A: Statistical analyses of overall protein concentration in bronchoalveolar lavage fluid in the four groups (n = 7); B-F: Statistical analyses of myeloperoxidase, tumor necrosis factor-alpha, interleukin (IL)-1β, IL-6, and IL-10 levels in the lung tissues in the indicated groups (n = 7); G and H: Macrophage inflammatory protein (MIP)-1α and MIP-1β mRNA expression in the indicated groups (n = 5); I: Malondialdehyde levels were measured to evaluate the degree of oxidative reaction in the lung tissues (n = 7). aP < 0.05; bP < 0.01; cP < 0.001. iT: Intratracheal; iP: Intraperitoneal; BALF: Bronchoalveolar lavage fluid; MPO: Myeloperoxidase; TNF-α: Tumor necrosis factor-alpha; IL: Interleukin; MIP: Macrophage inflammatory protein; MDA: Malondialdehyde; MSC: Mesenchymal stem cell.
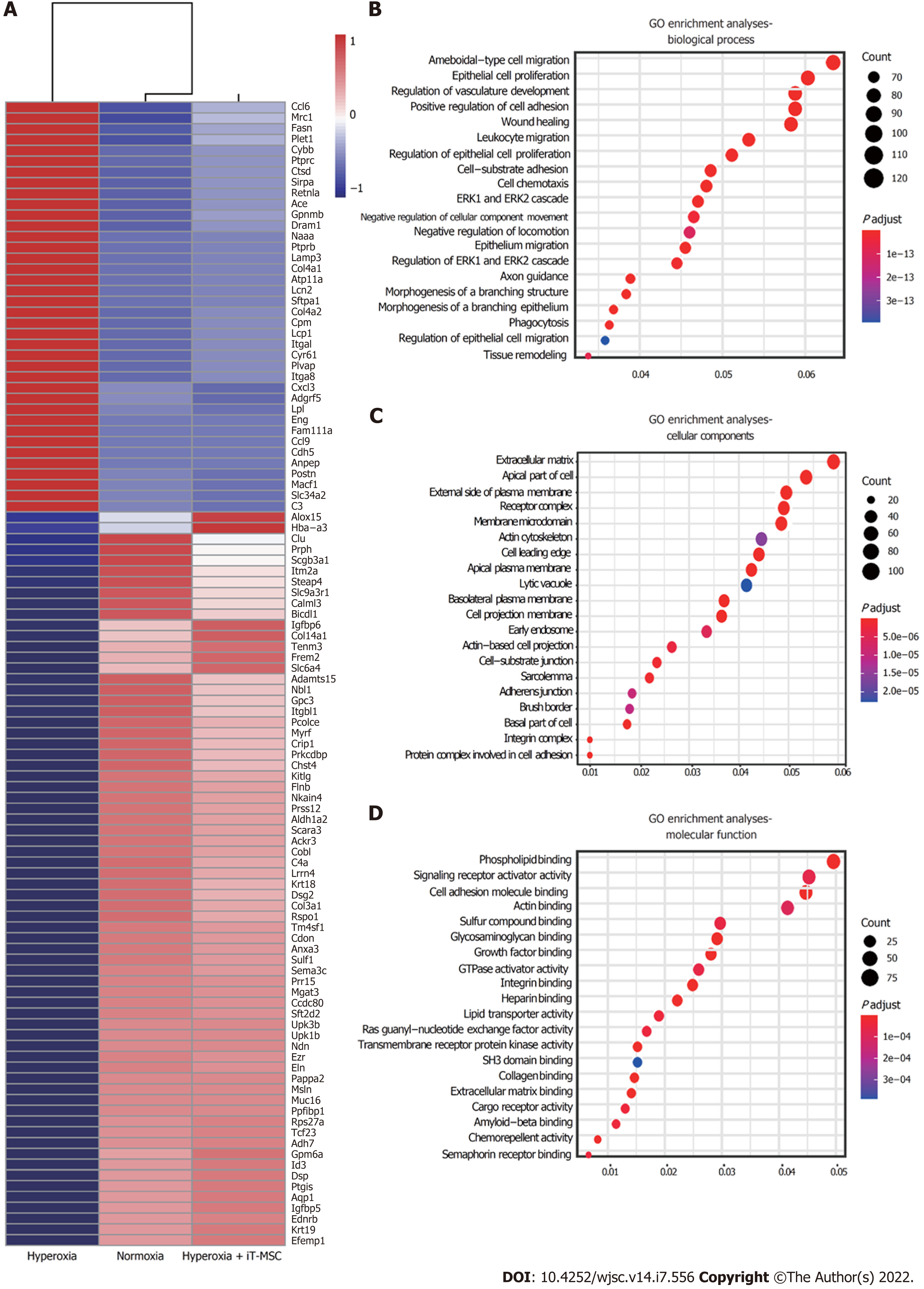
Figure 5 Human umbilical cord-derived mesenchymal stem cells treatment modulates the lung transcriptome.
A: The heatmap shows the top 100 differentially expressed genes in lung tissues from the normoxia, hyperoxia, and hyperoxia + intratracheal-mesenchymal stem cell groups. The expression levels of up- and downregulated genes are shown in red and blue, respectively; B-D: Gene ontology analyses of the most significantly affected pathways related to biological process, cellular components, and molecular function. iT: Intratracheal; MSC: Mesenchymal stem cell; GO: Gene ontology.
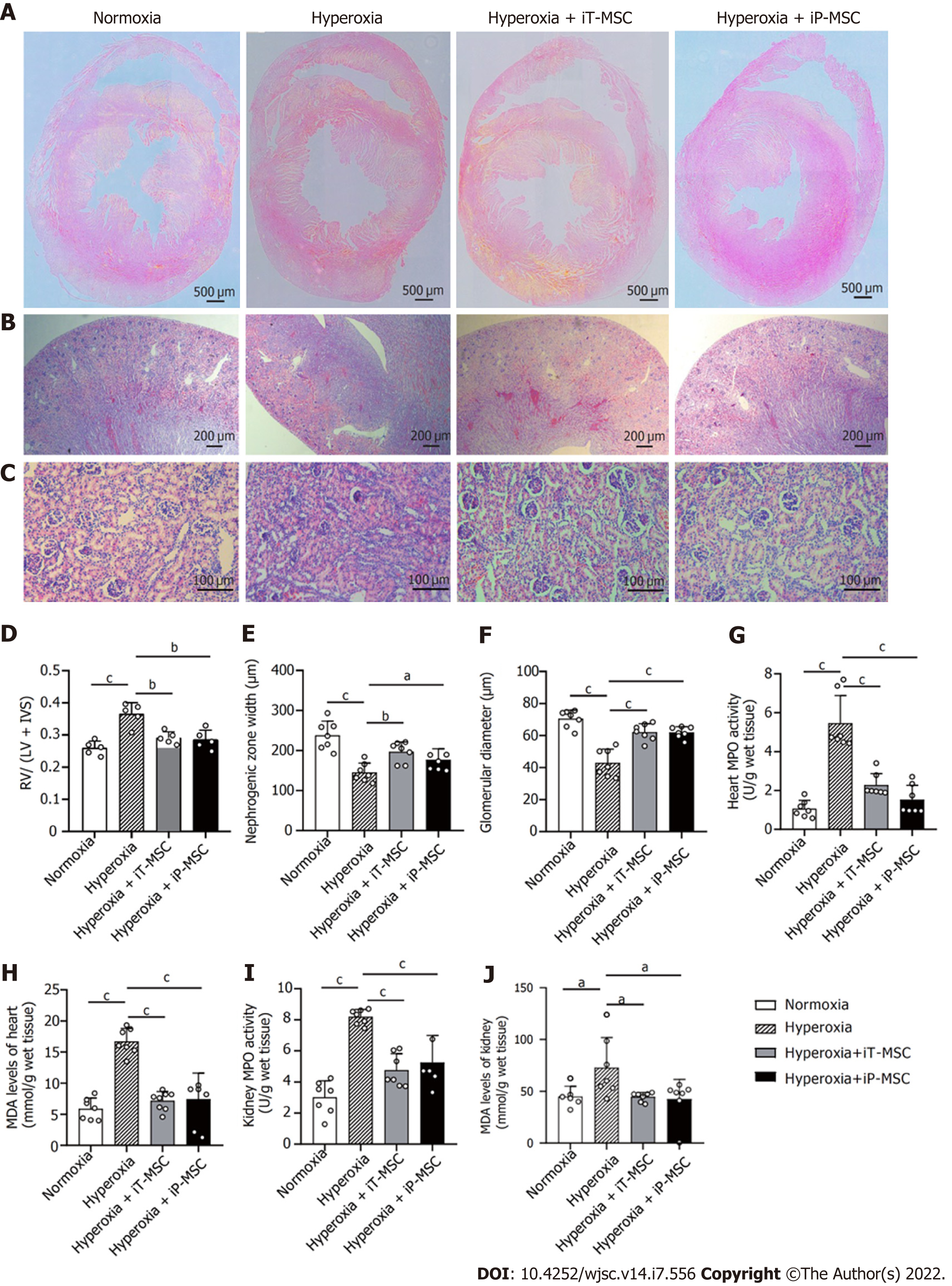
Figure 6 Beneficial effects of human umbilical cord-derived mesenchymal stem cells administration in the heart and kidneys of hyperoxic neonatal rats.
A: Representative images of harvested heart sections stained with HE for morphometric analyses (scale bars = 500 μm); B and C: Representative photomicrographs of the hematoxylin and eosin stained sections of kidneys obtained at 40 × magnification (scale bars = 200 μm) and 200 × magnification (scale bars = 100 μm) respectively; D: Fulton’s index (right ventricle/left ventricle + interventricular septum) was measured to quantify the degree right ventricular hypertrophy (n = 5); E and F: Nephrogenesis was assessed through measuring the width of the nephrogenic zone and the glomerular diameter (n = 7); G–J: Myeloperoxidase and malondialdehyde levels were measured to evaluate the degree of inflammatory and oxidative reaction in heart and kidney tissues respectively (n = 7). aP < 0.05; bP < 0.01; cP < 0.001. iT: Intratracheal; iP: Intraperitoneal; RV: Right ventricle; LV: Left ventricle; IVS: Interventricular septum; MPO: Myeloperoxidase; MDA: Malondialdehyde; MSC: Mesenchymal stem cell.
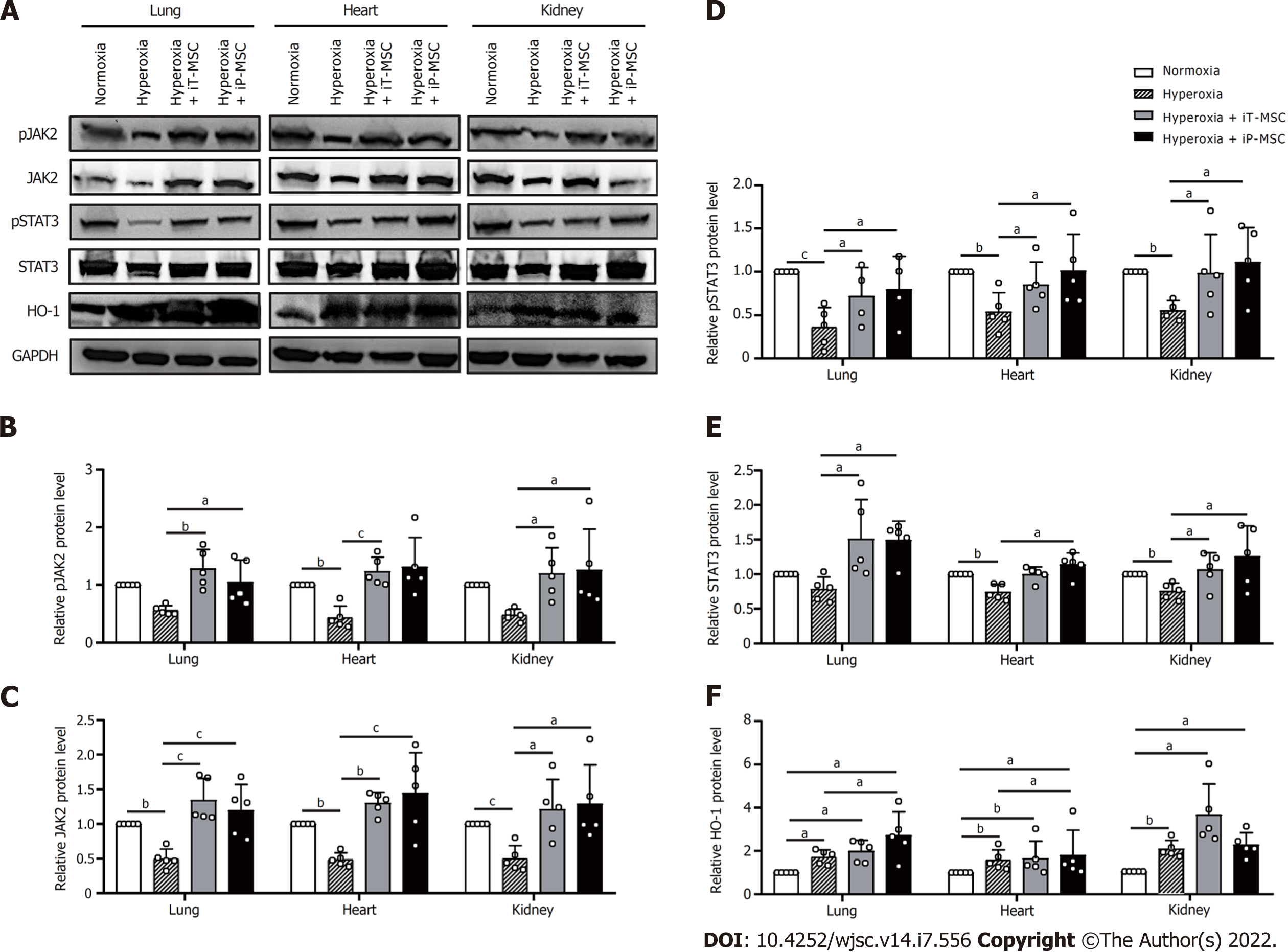
Figure 7 Human umbilical cord-derived mesenchymal stem cells activated the heme oxygenase-1 and JAK2/STAT3 signaling pathway to protect against hyperoxia-induced multiple-organ injury.
A: The protein extracted from tissue homogenates of the lungs, heart, and kidneys were collected for western blotting to detect heme oxygenase-1, JAK2, STAT3 protein expression levels, as well as their phosphorylation; B–F: Statistical analyses of protein expression levels of the above-mentioned genes. aP < 0.05; bP < 0.01; cP < 0.001. iT: Intratracheal; iP: Intraperitoneal; HO-1: Heme oxygenase-1; GAPDH: Glyceraldehyde-3-phosphate dehydrogenase; MSC: Mesenchymal stem cell.
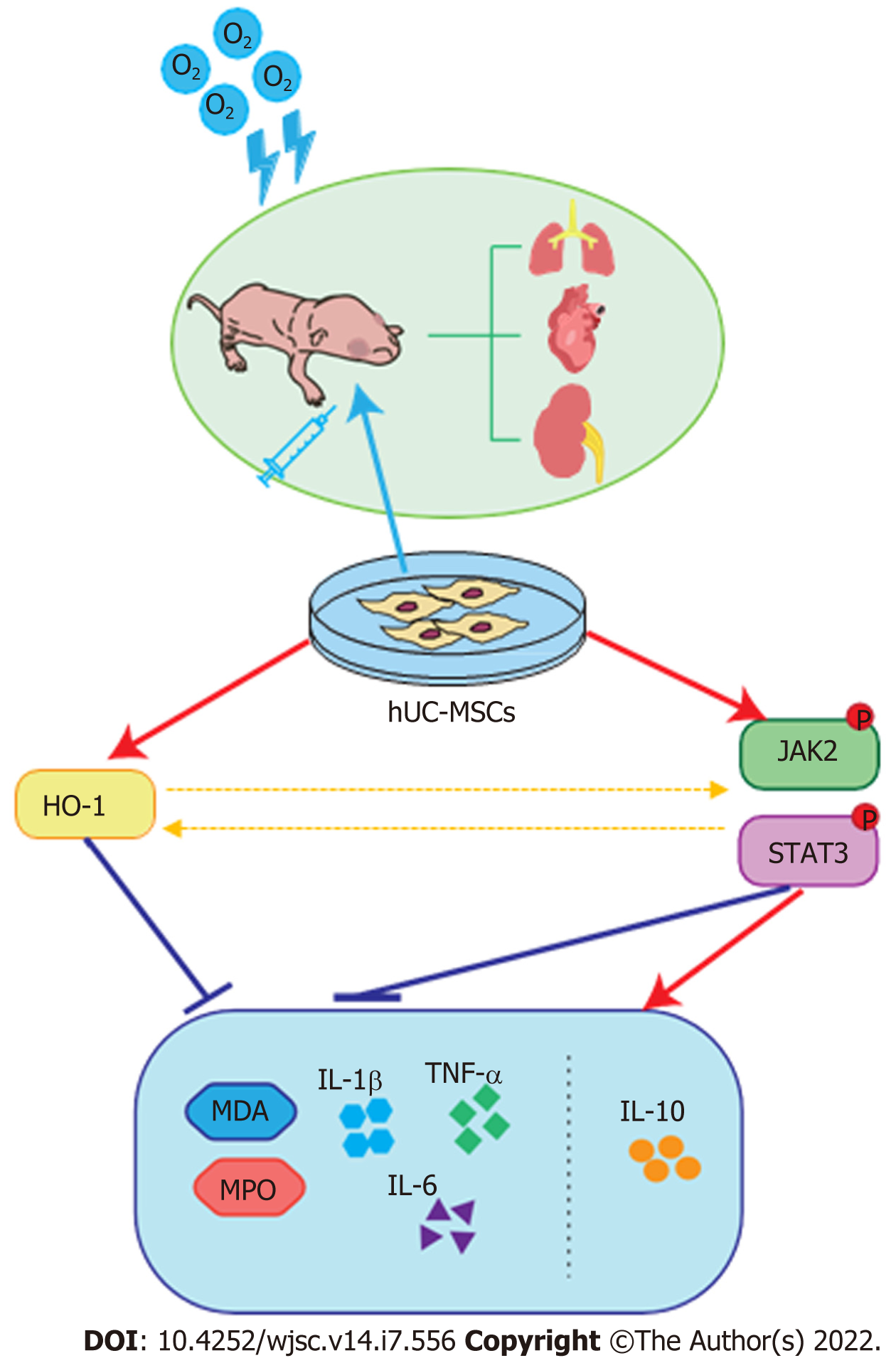
Figure 8 Proposed mechanism of therapeutic effects of human umbilical cord-derived mesenchymal stem cells in hyperoxia-induced multiple organ injury.
The administration of human umbilical cord-derived mesenchymal stem cells at postnatal day ameliorates hyperoxia-induced lung, heart, and kidney development, and reduces inflammatory and oxidative responses by activating heme oxygenase-1 expression and the JAK/STAT3 pathway. O2: Oxygen; hUC-MSCs: Human umbilical cord-derived mesenchymal stem cells; HO-1: Heme oxygenase-1; MPO: Myeloperoxidase; TNF-α: Tumor necrosis factor-alpha; IL: Interleukin; MDA: Malondialdehyde.
- Citation: Dong N, Zhou PP, Li D, Zhu HS, Liu LH, Ma HX, Shi Q, Ju XL. Intratracheal administration of umbilical cord-derived mesenchymal stem cells attenuates hyperoxia-induced multi-organ injury via heme oxygenase-1 and JAK/STAT pathways. World J Stem Cells 2022; 14(7): 556-576
- URL: https://www.wjgnet.com/1948-0210/full/v14/i7/556.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v14.i7.556