Copyright
©The Author(s) 2021.
World J Stem Cells. Aug 26, 2021; 13(8): 971-984
Published online Aug 26, 2021. doi: 10.4252/wjsc.v13.i8.971
Published online Aug 26, 2021. doi: 10.4252/wjsc.v13.i8.971
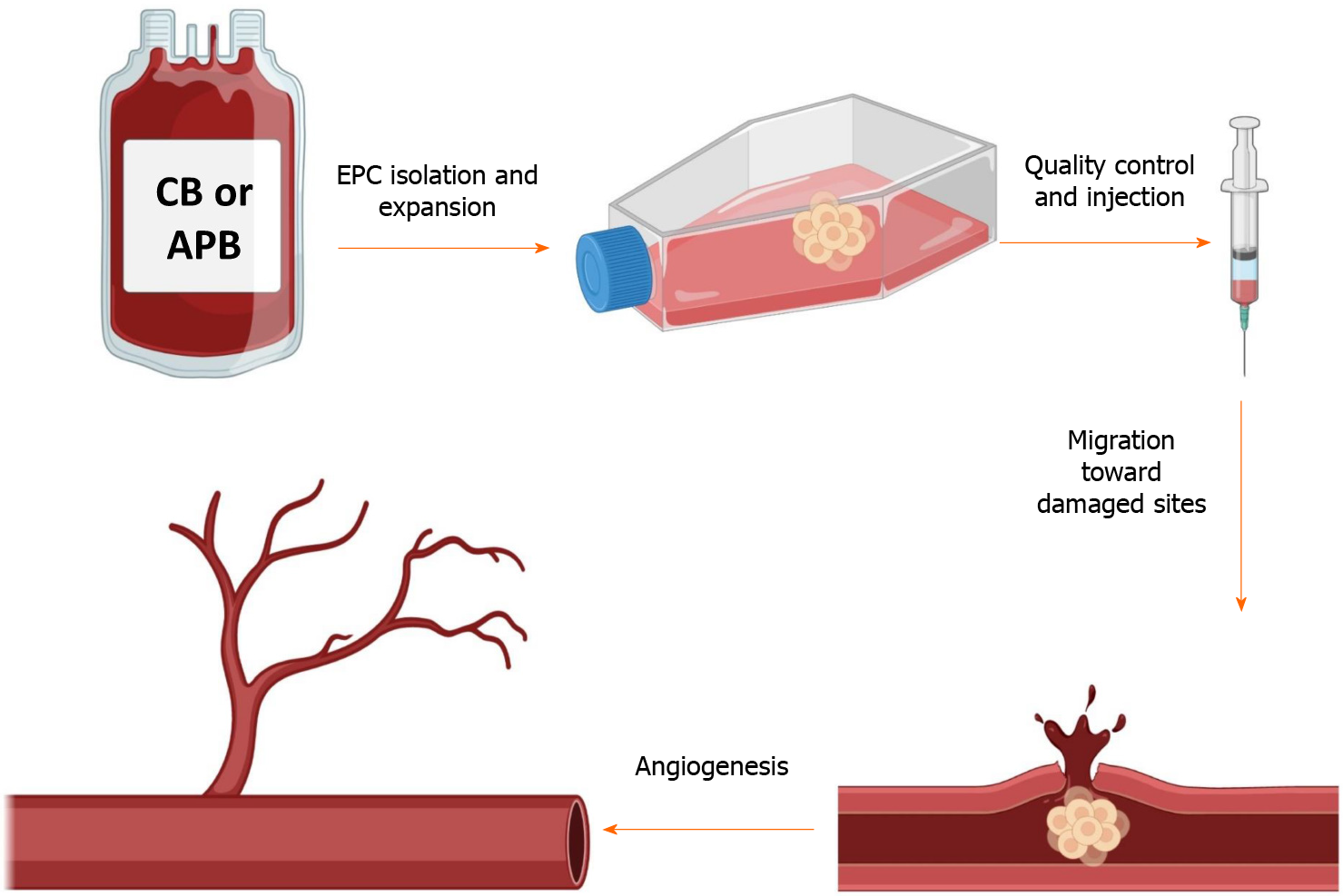
Figure 1 This schematic depicts the simplified procedure from isolation to the application of endothelial progenitor cells.
Briefly, endothelial progenitor cells (EPCs) are isolated from the cord blood or adult peripheral blood and are seeded on a culture flask. After the appearance of the first colonies (around 3 wk), cells are passaged and expanded to reach the desired numbers. After several verifications, EPCs could be injected into patients with cardiovascular disorders to take advantage of their regenerative and proangiogenic properties. The graphical images were created with BioRender.com. APB: Adult peripheral blood; CB: Cord blood.
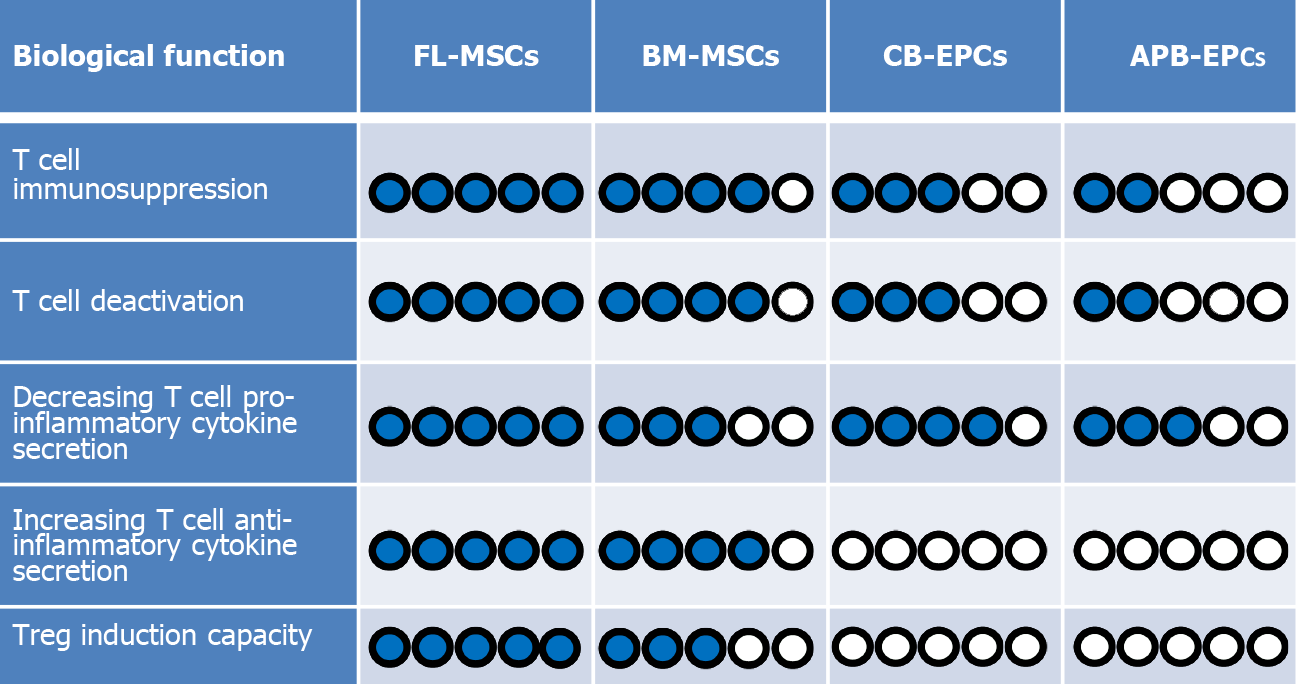
Figure 2 A comparison between immunoregulatory functions of mesenchymal stem cells and endothelial progenitor cells.
According to our evaluations, among the four cell types [fetal liver (FL) derived mesenchymal stem cells (MSCs), bone marrow-derived (BM)-MSCs, cord blood-derived (CB)-endothelial progenitor cells (EPCs), and adult peripheral blood-derived (APB)-EPCs]. Fetal liver-derived (FL)-MSCs are the most immunomodulatory cells because they: (1) suppress T cell proliferation; (2) decrease T cell activation phenotype; and (3) decrease T cell secretion of proinflammatory cytokines. On the other hand, they could more efficiently increase: (1) the secretion of anti-inflammatory cytokine; and (2) the induction of regulatory T cells (Tregs) more than the other cells. Therefore, we have considered FL-MSCs as the reference (5/5 blue points) regarding the measured criteria and compared the capacity of the other cells with them. In the case of CB-EPCs and APB-EPCs, because we did not notice any Treg induction or elevation of anti-inflammatory cytokine secretion we attributed a 0/5 score. Blue circles represent elevated levels while white circles represent the absence of the effect.
Figure 3 The comparison between mesenchymal stem cell and endothelial progenitor cell immunosuppressive activity in the presence and blockade of the tumor necrosis factor alpha-tumor necrosis factor receptor 2 signaling pathway.
Because the immunosuppressive function of mesenchymal stem cells (MSCs) is greater than endothelial progenitor cells (EPCs), we have kept them as the reference (5/5). In this case, in the presence of the tumor necrosis factor-alpha (TNFα)-tumor necrosis factor receptor 2 (TNFR2) signaling pathway (i.e. normal condition), MSCs have the highest immunosuppressive effect (5/5). On the other hand, in the presence of this signaling, EPCs have a less immunosuppressive effect (3/5). Interestingly, while blockade of this axis led to a complete loss of immunosuppressive function in EPC (0/5), MSCs kept suppressing T cells with less efficiency (2/5), showing that this axis is partially controlling their immunoregulatory properties.
- Citation: Razazian M, Khosravi M, Bahiraii S, Uzan G, Shamdani S, Naserian S. Differences and similarities between mesenchymal stem cell and endothelial progenitor cell immunoregulatory properties against T cells. World J Stem Cells 2021; 13(8): 971-984
- URL: https://www.wjgnet.com/1948-0210/full/v13/i8/971.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v13.i8.971