Copyright
©The Author(s) 2019.
World J Stem Cells. Aug 26, 2019; 11(8): 519-534
Published online Aug 26, 2019. doi: 10.4252/wjsc.v11.i8.519
Published online Aug 26, 2019. doi: 10.4252/wjsc.v11.i8.519
Figure 1 Role of stem cells in normal colon and CRC.
Within the normal colon, ISCs constantly divide to give rise to the differentiated cells within the epithelium that have a multitude of functions. In colorectal cancer, the ISCs can develop into CSCs that lead to tumor formation. Moreover, the transient amplifying cells as well as the differentiated intestinal cells can mutate into mature tumor cells that can subsequently dedifferentiate to form CSCs. Owing to genetic, epigenetic or environmental signals, the stationary CSCs can transform into migratory CSCs that pass via circulation to target organs and colonize. Critical pathways and genetic events have been shown for the entire process of CRC tumorigenesis and progression. Moreover, key biomarkers have been shown for the ISCs and the CRC based CSCs, although there is some overlap in this panel. CRC: Colorectal cancer; CSC: Cancer stem cells; ISC: Intestinal stem cell; EMT: Epithelial mesenchymal transition; Wnt: Wingless/integrated; APC: Adenomatous polyposis coli; KRAS: Kirsten rat sarcoma viral oncogene homolog; BMP: Bone morphogenetic protein; TGF-β: Transforming growth factor-β; VEGF: Vascular endothelial growth factor; MMP: Matrix metalloproteinase.
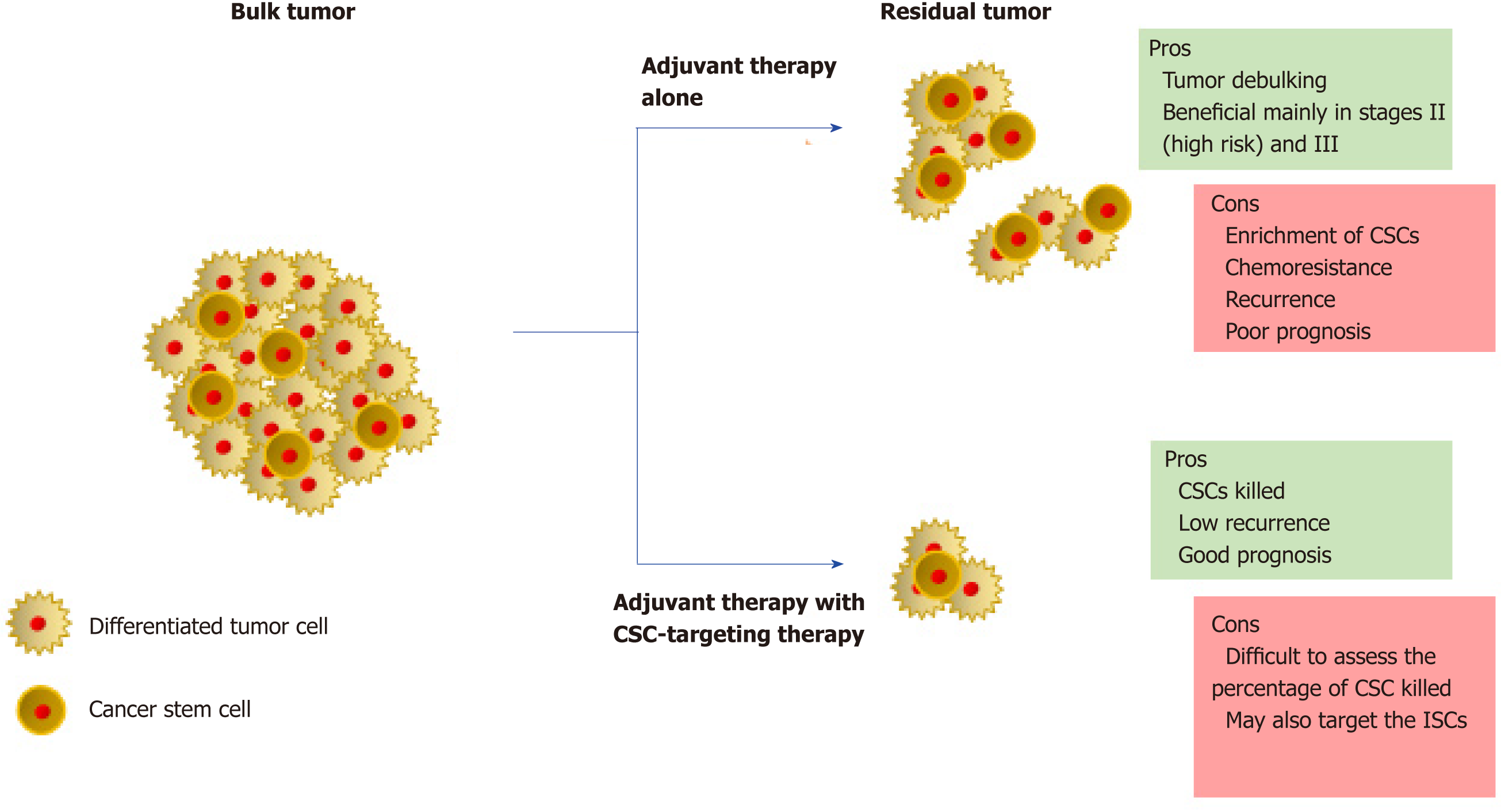
Figure 2 Therapeutic strategies in colorectal cancer.
Targeting the tumor bulk in colorectal cancer with adjuvant therapy leads to tumor regression, although CSCs may escape cell death. Such a chemoresistance event leads to tumor recurrence and overall poor prognosis. In contrast, treatment with a combination of adjuvant therapy and CSC-targeting therapy would also eradicate the CSC population, along with the tumor bulk. In the long term, reduction in CSC volume would kill the tumor. CSC: Cancer stem cells; ISC: Intestinal stem cells.
- Citation: Iyer DN, Sin WY, Ng L. Linking stemness with colorectal cancer initiation, progression, and therapy. World J Stem Cells 2019; 11(8): 519-534
- URL: https://www.wjgnet.com/1948-0210/full/v11/i8/519.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v11.i8.519