修回日期: 2022-05-25
接受日期: 2022-06-21
在线出版日期: 2022-07-28
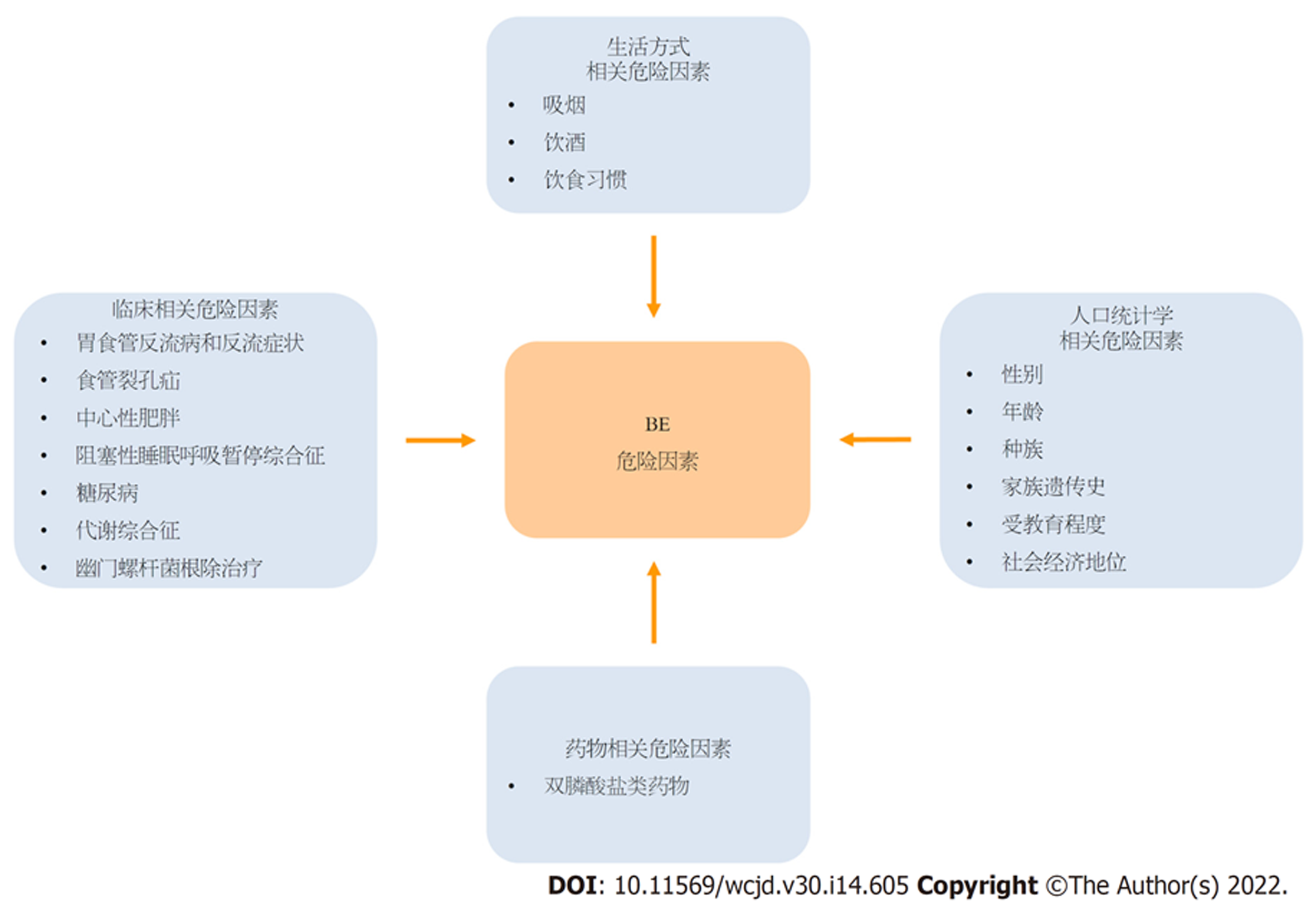
食管腺癌(esophageal adenocarcinoma, EAC)是西方国家最常见的食管恶性肿瘤. 近年来, 其发病率在我国也呈上升趋势. Barrett食管(Barrett's esophagus, BE)是指食管下段的鳞状上皮被化生的柱状上皮所取代的病理现象. BE与EAC的发生密切相关. 了解BE发生发展的相关危险因素对早期筛查和诊断BE及预防EAC具有重要意义. 本文主要从临床、人口统计学、生活习惯和药物使用四个方面阐述BE的危险因素, 以期为BE的临床防治提供更多有价值的科学依据.
核心提要: Barrett食管(Barrett's esophagus, BE)是食管腺癌(esophageal adenocarcinoma, EAC)的癌前病变. 充分了解BE的危险因素是十分必要的. 本文将从临床、人口统计学、生活习惯和药物四个方面阐述BE的危险因素, 以指导临床防治BE.
引文著录: 马韶泽, 陈鸿鑫, 梁振东, 祁兴顺. Barrett食管危险因素的研究进展. 世界华人消化杂志 2022; 30(14): 605-613
Revised: May 25, 2022
Accepted: June 21, 2022
Published online: July 28, 2022
Esophageal adenocarcinoma (EAC) is the most common malignant tumor of the esophagus in the West. During the past few decades, its morbidity has been increasing in China. Barrett's esophagus (BE) is defined as the replacement of normal squamous epithelium in the lower esophagus by metaplasia of columnar epithelium. BE is closely related to the occurrence of EAC. Knowledge regarding the risk factors for the occurrence and development of BE is of great significance for early screening and diagnosis of BE and prevention of EAC. In this paper, we review the clinical, demographics-related, lifestyle-related, and medications-related risk factors for BE to provide more valuable scientific evidence for the prevention and treatment of BE.
- Citation: Ma SZ, Chen HX, Liang ZD, Qi XS. Risk factors for Barrett's esophagus: Recent advances. Shijie Huaren Xiaohua Zazhi 2022; 30(14): 605-613
- URL: https://www.wjgnet.com/1009-3079/full/v30/i14/605.htm
- DOI: https://dx.doi.org/10.11569/wcjd.v30.i14.605
食管癌是常见的上消化道恶性肿瘤之一, 其发病率及死亡率分别居世界恶性肿瘤的第8位及第6位[1]. 在西方国家, 食管腺癌(esophageal adenocarcinoma, EAC)已替代食管鳞癌成为最常见的食管癌病理类型[2], 近年来, 其发病率在中国也呈上升趋势[3]. Barrett食管(Barrett's esophagus, BE)是指食管与胃黏膜交界处的连接线(齿状线, 又称Z线)1 cm以上的食管下段的正常复层鳞状上皮被化生的单层柱状上皮所取代的一种病理现象[4]. BE是目前唯一已知的EAC的癌前病变[5], 有报道显示[6], 80%的EAC与BE密切相关, BE患者罹患EAC的风险是正常人群的30-40倍[7]. 因此, 识别和了解BE发生发展的相关危险因素对其早期诊治及降低EAC的发病率具有重要意义. 本文通过全面概述BE发生发展的相关危险因素的临床研究证据, 为BE的临床防治提供更多有价值的科学依据.
胃食管反流病(gastroeso-phageal reflux disease, GERD)是指胃十二指肠内容物反流至食管引起的相关症状和(或)并发症的疾病, 是公认发生BE最主要的危险因素[8]. 一项基于爱尔兰人群的病例对照研究证实, GERD与发生BE显著相关(OR = 12.0, 95%CI = 7.64-18.70)[9]. 然而, 并非所有的GERD患者均会出现反酸、胃灼热等反流症状[10,11]. 为此, 多项研究也进一步探讨了反流症状与发生BE之间的关系, 它们发现, 反流症状的发作频率和严重程度与BE的发生风险呈正相关[11-18]. 一项纳入了26项研究的荟萃分析发现, 反流症状与短段BE的发生风险无关(OR = 1.15, 95%CI = 0.76-1.73), 但与长段BE的发生风险显著相关(OR = 4.92, 95%CI = 2.01-12.00), 反流症状似乎只能作为长段BE的可靠预测指标[19]. 持续的胃酸反流可诱导食管鳞状上皮改变发育转录因子的表达模式, 使其逐步转化为柱状上皮和肠上皮, 最终发展为BE[20]. 除胃酸反流外, 胆汁反流在BE的发生发展中也可能起着重要作用. 由胆汁酸诱导的食管组织氧化应激和DNA损伤可激活BE细胞的抗凋亡通路并增加炎性反应, 从而促进BE的发生发展[21]. 当前指南认为, 长期GERD病史和(或)>5年的反流症状是BE的危险因素[4,22-25].
食管裂孔疝(hiatal hernia, HH)是指除食管以外的任何腹腔组织结构通过扩大的食管裂孔进入胸腔形成的疝[26]. BE患者中HH的发病率高达96%[27]. 一项横断面研究发现, BE患者HH的患病率显著高于非BE患者(79.8% vs 52.8%, P<0.01); 并且HH是BE的独立危险因素(OR = 3.04, 95%CI = 1.77-5.23, P<0.01)[28]. 一项纳入了13项研究的荟萃分析也证实, HH显著增加了BE的发生风险(OR = 2.74, 95%CI = 1.58-4.75)[29]. 这可能是因为HH可降低食管下括约肌(transient lower esophageal sphincter, LES)压力, 从而加重胃酸和胆汁反流, 最终增加BE的发生风险.
根据脂肪分布部位, 肥胖可分为全身性肥胖和中心性肥胖. 中心性肥胖是指以腹部或内脏脂肪积聚为主引起的肥胖, 比全身性肥胖对健康的危害更大, 是多种慢性病的重要危险因素[30]. 研究表明[15,31-33], 中心性肥胖是发生BE的独立预测因素. 两项病例对照研究比较了有无BE患者的脂肪分布、脂肪含量和体脂百分比, 以探讨肥胖类型与BE的关系; 结果显示, 腰围、腰臀比等中心性肥胖指标与BE的患病风险呈正相关, 而体重指数(body mass index, BMI)、脂肪含量、体脂百分比等全身性肥胖指标与BE的患病风险无关[15,32]. 此外, Nelsen等[33]发现内脏脂肪(OR = 4.88, 95%CI = 1.04-22.85, P<0.01)和胃食管交界处脂肪(OR = 5.97, 95%CI = 1.28-27.74, P<0.01)堆积也会增加BE的患病风险, 且不受BMI的影响. 多项荟萃分析也证实, 通过腰围、腰臀比和(或)内脏脂肪组织面积鉴定的中心性肥胖可独立预测BE的发生风险[34-36]. 这是由于中心性肥胖可以导致腹内压力增加并机械地破坏胃食管交界处屏障的完整性, 从而促进胃酸和胆汁反流, 进而加重反流性食管炎并诱导食管鳞状上皮化生, 最终导致BE形成[37-40]. 另一方面, 中心性肥胖患者内脏脂肪组织代谢活跃, 促进了白细胞介素-6(interleukin-6, IL-6)、白细胞介素-1β(interleukin-1β, IL-1β)、肿瘤坏死因子-α(tumor necrosis factor-α, TNF-α)等炎性细胞因子和脂联素(adiponectin, APN)、游离脂肪酸(free fatty acid, FFA)、瘦素(leptin, LEP)等脂肪因子的释放, 这些生物活性物质通过远距分泌和旁分泌的方式发挥全身慢性炎症作用, 独立或协同地促进BE的发生发展[40-45].
阻塞性睡眠呼吸暂停综合征(obstructive sleep apnea syndrome, OSAS)是指睡眠期间气道部分或完全阻塞, 导致以间歇性缺氧和低通气为主要临床表现的一种潜在致死性综合征[46]. OSAS患者睡眠时常因呼吸道阻塞导致吸气时胸腔负压和食管内负压增高, 且呼吸暂停后连续吸气会引起胸腔和LES压力降低, 从而加重胃食管反流并诱发BE[47,48]. 此外, OSAS患者多肥胖[49]; 相较于健康人群, 肥胖人群的腹内压力显著更高, 因此更容易引起胃食管返流, 最终导致BE的发生[41]. 最近, Hadi等[50]的研究结果显示, BE患者OSAS的患病率显著高于非BE患者(90.7% vs 72.4%, P<0.01). 当校正GERD和BMI后, OSAS仍显著增加了BE的发生风险(OR = 3.26, 95%CI = 1.72-6.85, P<0.01), 且随着OSAS的程度加重, BE的发生风险随之上升, 这可能与缺氧诱导的全身慢性炎症反应有关, 而不完全依赖于胃食管反流和肥胖[50].
仅少数研究探讨了糖尿病(diabetes mellitus, DM)与BE之间的关联, 且研究结果并不一致. 一项大型的病例对照研究发现, BE患者的DM患病率显著高于非BE患者(5.8% vs 5.3%, P<0.05); 校正BMI、GERD等危险因素后, DM仍显著增加了BE的发生风险 (OR = 1.49, 95%CI = 1.16-1.91, P<0.01)[51]. 然而, 另一项基于英国人群的病例对照研究发现, DM并不会增加BE的发病风险(OR = 1.07, 95%CI = 0.98-1.18)[52]. 最近一项荟萃分析也发现, DM与BE无关(OR = 0.93, 95%CI = 0.71-1.20), 但显著增加了EAC的发生风险(OR = 1.63, 95%CI = 1.19-2.22). 这些研究结果提示DM可能不会影响BE的发病, 但会促进BE进展至EAC[53].
代谢综合征(metabolic syndrome, MS)是以胰岛素抵抗、中心性肥胖、高脂血症及高血压等疾病为主的症候群[54]. 多项研究显示, MS是发生BE的高危因素[52,54,55]. 最近, 一项纳入了14项研究的荟萃分析也证实, MS显著增加了BE的发病风险(OR = 1.35, 95%CI = 1.15-1.60, P<0.01)[56]. 此外, 一项基于白人男性退伍军人的病例对照研究表明, MS的严重程度与BE的发生风险呈剂量-反应关系, 即BE的发病风险随着MS成分数量的增加而呈线性增加, 且高脂血症对BE的发生风险影响最大[57]. 除了脂肪因子可发挥全身慢性炎症作用外[45], MS患者血清中的高甘油三酯水平还会促进胆囊收缩素的分泌, 从而延缓胃排空并降低LES压力[58], 最终加重胃食管反流并诱导BE形成. 此外, 胰岛素样生长因子-1(insulin-like growth factor-I, IGF-1)与靶细胞表面的相应受体结合可调控食管上皮细胞的增殖和分化[59]. 因此, 继发于MS的血清高IGF-1水平可能会进一步增加MS患者发生BE的风险[60].
幽门螺杆菌(Helicobacter pylori, H. pylori)是一种定植于胃黏膜的微需氧革兰氏阴性菌, 1994年世界卫生组织将其认定为Ⅰ类致癌原[61]. 多数研究认为, H. pylori感染, 尤其是CagA阳性菌株感染, 与BE的发病风险呈负相关 [62-65]. 最近, 一项荟萃分析也表明, H. pylori感染可能是发生BE的保护因素(OR = 0.70, 95%CI = 0.51-0.96, P<0.05), 并且CagA阳性菌株感染对发生BE的保护作用更为明显(OR = 0.28, 95%CI= 0.15-0.54, P<0.01)[66]. 这可能是因为持续的H. pylori感染通过破坏壁细胞的功能、升高LES压力以及减少一过性食管下括约肌松弛(transient lower esophageal sphincter relaxations, TLESR)的频率及持续时间, 减少了胃酸的分泌和反流, 最终降低了BE的发生风险[37,67,68]. 目前, 仅有一项基于瑞典人群的前瞻性队列研究探讨了H. pylori根除治疗与BE发病风险的关系, 结果显示, H. pylori根除治疗后, 瑞典人群BE的发病率显著增加(SIR = 3.67, 95%CI = 3.15-4.25)[69], 提示H. pylori根除治疗可能是BE的危险因素.
男性BE的发病率是女性的1.5-4.0倍[70-72]. 性激素的差异可能在一定程度上解释了这一现象. 一项基于男性的病例对照研究发现, 游离睾酮(OR = 5.36, 95%CI = 2.21-13.03, P<0.01)和游离双氢睾酮(OR = 4.25, 95%CI = 1.87-9.66, P<0.01)可显著增加BE的发生风险, 睾酮可降低LES压力并增加TLESR的频率, 从而加重胃食管反流[73]. 一项动物实验也发现, 雌激素可通过抑制壁细胞的功能并减少壁细胞的数量, 以降低基础胃酸分泌, 从而降低BE的发生风险[74].
年龄是发生BE的独立危险因素. 年龄每增加10岁, 罹患BE的风险将增加1-2倍[13,75,76]. 一项来自英国和荷兰的多中心、回顾性队列研究比较了不同年龄段人群发生BE的风险; 结果显示, 在40岁-44岁组, 英国和荷兰BE的发病率分别为16/105和24/105; 在70岁-74岁组, 英国和荷兰BE的发病率分别增至85.6/105和87/105, BE的发病率与年龄呈线性相关[77]. 目前国内外多项指南也推荐, 年龄>50岁是发生BE的独立预测因素[4,22-25,78].
全球范围内, 白人种族BE的发病率最高[79]. 一项纳入20412例患者的观察性研究发现, 白人发生BE的风险是黄种人的6倍(OR = 6.03, 95%CI = 3.56-10.22)[72]; 同样, 一项来自美国的大型横断面研究表明, 白人BE的发病率是黑人的5倍[71]. 目前尚不清楚种族对BE发生发展的作用机制. 白人种族肥胖率更高可能是其BE高发病率的原因[80].
BE可能是具有遗传倾向的后天性疾病[81], BE及其相关癌症家族史可增加BE的发生风险. Chak等[82,83]发现, 约7.3%的BE患者有BE或EAC家族史. 目前, 几项全基因组关联研究已确定CRTC1、FOXP1、BARX1、TBX5、GDF7等是BE和EAC的易感基因[84-86].
吸烟可能会增加BE的发生风险. BE患者吸烟史的比例显著高于人群对照组, 且BE的发生风险与吸烟包年数呈正相关[91]. Balasubramanian等[92]进一步指出, 吸烟的GERD患者BE的患病率显著高于无吸烟史的GERD患者(5.2% vs 17.0%, P<0.01), 吸烟是GERD患者发生BE的独立危险因素; 随着戒烟时间的延长, BE的发生风险逐渐降低(P for trend<0.01). 此外, 一项随访16年的前瞻性队列研究也发现, 吸烟史和吸烟时长均显著增加了BE的发生风险[93]. 这是由于尼古丁可降低LES压力并导致频繁的TLESR, 从而促进胃食管反流, 最终诱导Barrett上皮生成[94].
多数研究未发现饮酒与BE之间存在直接关联[13,89,93,95-98]. 然而, 最近一项纳入了62项观察性研究的荟萃分析却表明, 饮酒可能是发生BE的危险因素(RR = 1.23, 95%CI = 1.13-1.34, P<0.01)[99]. 这可能是由于酒精会导致LES压力降低并加重反流症状, 从而引起食管黏膜损伤并诱导BE形成[98].
近期, 多项研究探讨了饮食习惯与BE的相关性. 随着糖类[100-102]和脂肪[102,103]摄入量的增加以及膳食纤维[104,105]和富含膳食抗氧化剂的蔬菜、水果[101,102,106-108]摄入量的减少, BE的发生风险将逐渐增加. 高糖高脂和低膳食纤维饮食通过损伤食管黏膜或影响其它危险因素, 如GERD、HH和中心性肥胖, 直接或间接地促进BE的发生发展[109]. 当蔬菜、水果的摄入量过少时, 人体便会缺乏某些抗氧化活性成分(维生素C、维生素E、硒、镁和β-胡萝卜素)[101,107,108], 从而诱导食管组织氧化应激和DNA损伤, 进而促进BE细胞增殖并增加炎性反应, 最终增加BE的发生风险[110-112].
仅少数研究探讨了药物和BE发病风险之间的相关性. 一项基于美国退伍军人的病例对照研究比较了有无BE患者双膦酸盐类药物的使用情况, 结果发现, BE患者双膦酸盐类药物的使用率显著高于非BE患者(4.6% vs 2.5%), 且口服双膦酸盐类药物可能是发生BE的危险因素(OR = 2.33, 95%CI = 1.11-4.88, P<0.01)[113]. 双膦酸盐是破骨细胞介导的骨质吸收的选择性抑制剂, 用于治疗和预防骨质疏松症[113]. 它可通过抑制甲羟戊酸途径干扰细胞周期进程, 从而影响食管上皮干细胞的增殖与分化, 最终加重胃食管反流引起的食管损伤并诱导Barrett上皮生成[114]. 此外, 有研究也发现, 非甾体类抗炎药[99,115]和他汀类药物[116]的使用可能会降低BE的发生风险.
作为目前唯一已知的EAC的癌前病变, BE在全球的发病率不断升高. 因此, 掌握BE发生发展的危险因素对于EAC的预防、风险分层、早期识别和诊治至关重要. 除性别、种族、遗传等不可变因素外, 以GERD、中心性肥胖、吸烟等为主的可变危险因素应引起重视(图1). 未来应正确引导人们认识这些危险因素, 提高人群健康意识, 保持良好的生活习惯, 从而降低BE和EAC的发病率.
学科分类: 胃肠病学和肝病学
手稿来源地: 辽宁省
同行评议报告学术质量分类
A级 (优秀): 0
B级 (非常好): B
C级 (良好): C
D级 (一般): 0
E级 (差): 0
科学编辑: 张砚梁 制作编辑:张砚梁
| 1. | Domper Arnal MJ, Ferrández Arenas Á, Lanas Arbeloa Á. Esophageal cancer: Risk factors, screening and endoscopic treatment in Western and Eastern countries. World J Gastroenterol. 2015;21:7933-7943. [PubMed] [DOI] |
| 2. | Pennathur A, Gibson MK, Jobe BA, Luketich JD. Oesophageal carcinoma. Lancet. 2013;381:400-412. [PubMed] [DOI] |
| 3. | Yeh C, Hsu CT, Ho AS, Sampliner RE, Fass R. Erosive esophagitis and Barrett's esophagus in Taiwan: a higher frequency than expected. Dig Dis Sci. 1997;42:702-706. [PubMed] [DOI] |
| 4. | Fitzgerald RC, di Pietro M, Ragunath K, Ang Y, Kang JY, Watson P, Trudgill N, Patel P, Kaye PV, Sanders S, O'Donovan M, Bird-Lieberman E, Bhandari P, Jankowski JA, Attwood S, Parsons SL, Loft D, Lagergren J, Moayyedi P, Lyratzopoulos G, de Caestecker J; British Society of Gastroenterology. British Society of Gastroenterology guidelines on the diagnosis and management of Barrett's oesophagus. Gut. 2014;63:7-42. [PubMed] [DOI] |
| 5. | Thrift AP. Barrett's Esophagus and Esophageal Adenocarcinoma: How Common Are They Really? Dig Dis Sci. 2018;63:1988-1996. [PubMed] [DOI] |
| 6. | Wilson KT, Fu S, Ramanujam KS, Meltzer SJ. Increased expression of inducible nitric oxide synthase and cyclooxygenase-2 in Barrett's esophagus and associated adenocarcinomas. Cancer Res. 1998;58:2929-2934. [PubMed] |
| 7. | Desai TK, Krishnan K, Samala N, Singh J, Cluley J, Perla S, Howden CW. The incidence of oesophageal adenocarcinoma in non-dysplastic Barrett's oesophagus: a meta-analysis. Gut. 2012;61:970-976. [PubMed] [DOI] |
| 8. | Mikolašević I, Bokun T, Filipec Kanižaj T. Gastroesophageal reflux disease, Barrett esophagus, and esophageal adenocarcinoma - where do we stand? Croat Med J. 2018;59:97-99. [PubMed] [DOI] |
| 9. | Anderson LA, Watson RG, Murphy SJ, Johnston BT, Comber H, Mc Guigan J, Reynolds JV, Murray LJ. Risk factors for Barrett's oesophagus and oesophageal adenocarcinoma: results from the FINBAR study. World J Gastroenterol. 2007;13:1585-1594. [PubMed] [DOI] |
| 10. | Shaheen NJ, Weinberg DS, Denberg TD, Chou R, Qaseem A, Shekelle P; Clinical Guidelines Committee of the American College of Physicians. Upper endoscopy for gastroesophageal reflux disease: best practice advice from the clinical guidelines committee of the American College of Physicians. Ann Intern Med. 2012;157:808-816. [PubMed] [DOI] |
| 11. | Quach DT, Pham QTT, Tran TLT, Vu NTH, Le QD, Nguyen DTN, Dang NLB, Le HM, Le NQ, Sharma P, Ho KY. Prevalence, clinical characteristics, and risk factors of Barrett esophagus in Vietnamese patients with upper gastrointestinal symptoms. Medicine (Baltimore). 2020;99:e21791. [PubMed] [DOI] |
| 12. | Asreah RH, Abdullhameed A. Risk factors of erosive esophagitis and barrett's esophagus in patients with reflux symptoms. Med J Islam Repub Iran. 2021;35:75. [PubMed] [DOI] |
| 13. | Eloubeidi MA, Provenzale D. Clinical and demographic predictors of Barrett's esophagus among patients with gastroesophageal reflux disease: a multivariable analysis in veterans. J Clin Gastroenterol. 2001;33:306-309. [PubMed] [DOI] |
| 14. | Johansson J, Håkansson HO, Mellblom L, Kempas A, Johansson KE, Granath F, Nyrén O. Risk factors for Barrett's oesophagus: a population-based approach. Scand J Gastroenterol. 2007;42:148-156. [PubMed] [DOI] |
| 15. | Kendall BJ, Macdonald GA, Prins JB, O'Brien S, Whiteman DC; Study of Digestive Health. Total body fat and the risk of Barrett's oesophagus - a bioelectrical impedance study. Cancer Epidemiol. 2014;38:266-272. [PubMed] [DOI] |
| 16. | Liu X, Wong A, Kadri SR, Corovic A, O'Donovan M, Lao-Sirieix P, Lovat LB, Burnham RW, Fitzgerald RC. Gastro-esophageal reflux disease symptoms and demographic factors as a pre-screening tool for Barrett's esophagus. PLoS One. 2014;9:e94163. [PubMed] [DOI] |
| 17. | Campos GM, DeMeester SR, Peters JH, Oberg S, Crookes PF, Hagen JA, Bremner CG, Sillin LF, Mason RJ, DeMeester TR. Predictive factors of Barrett esophagus: multivariate analysis of 502 patients with gastroesophageal reflux disease. Arch Surg. 2001;136:1267-1273. [PubMed] [DOI] |
| 18. | Thrift AP, Kramer JR, Qureshi Z, Richardson PA, El-Serag HB. Age at onset of GERD symptoms predicts risk of Barrett's esophagus. Am J Gastroenterol. 2013;108:915-922. [PubMed] [DOI] |
| 19. | Taylor JB, Rubenstein JH. Meta-analyses of the effect of symptoms of gastroesophageal reflux on the risk of Barrett's esophagus. Am J Gastroenterol. 2010;105:1729, 1730-7; quiz 1738. [PubMed] [DOI] |
| 20. | Wang DH, Clemons NJ, Miyashita T, Dupuy AJ, Zhang W, Szczepny A, Corcoran-Schwartz IM, Wilburn DL, Montgomery EA, Wang JS, Jenkins NA, Copeland NA, Harmon JW, Phillips WA, Watkins DN. Aberrant epithelial-mesenchymal Hedgehog signaling characterizes Barrett's metaplasia. Gastroenterology. 2010;138:1810-1822. [PubMed] [DOI] |
| 21. | Dvorak K, Payne CM, Chavarria M, Ramsey L, Dvorakova B, Bernstein H, Holubec H, Sampliner RE, Guy N, Condon A, Bernstein C, Green SB, Prasad A, Garewal HS. Bile acids in combination with low pH induce oxidative stress and oxidative DNA damage: relevance to the pathogenesis of Barrett's oesophagus. Gut. 2007;56:763-771. [PubMed] [DOI] |
| 22. | Weusten B, Bisschops R, Coron E, Dinis-Ribeiro M, Dumonceau JM, Esteban JM, Hassan C, Pech O, Repici A, Bergman J, di Pietro M. Endoscopic management of Barrett's esophagus: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy. 2017;49:191-198. [PubMed] [DOI] |
| 23. | Shaheen NJ, Falk GW, Iyer PG, Gerson LB; American College of Gastroenterology. ACG Clinical Guideline: Diagnosis and Management of Barrett's Esophagus. Am J Gastroenterol. 2016;111:30-50; quiz 51. [PubMed] [DOI] |
| 24. | ASGE Standards of Practice Committee, Evans JA, Early DS, Fukami N, Ben-Menachem T, Chandrasekhara V, Chathadi KV, Decker GA, Fanelli RD, Fisher DA, Foley KQ, Hwang JH, Jain R, Jue TL, Khan KM, Lightdale J, Malpas PM, Maple JT, Pasha SF, Saltzman JR, Sharaf RN, Shergill A, Dominitz JA, Cash BD; Standards of Practice Committee of the American Society for Gastrointestinal Endoscopy. The role of endoscopy in Barrett's esophagus and other premalignant conditions of the esophagus. Gastrointest Endosc. 2012;76:1087-1094. [PubMed] [DOI] |
| 25. | American Gastroenterological Association, Spechler SJ, Sharma P, Souza RF, Inadomi JM, Shaheen NJ. American Gastroenterological Association medical position statement on the management of Barrett's esophagus. Gastroenterology. 2011;140:1084-1091. [PubMed] [DOI] |
| 26. | Sfara A, Dumitrascu DL. The management of hiatal hernia: an update on diagnosis and treatment. Med Pharm Rep. 2019;92:321-325. [PubMed] [DOI] |
| 27. | Cameron AJ. Barrett's esophagus: prevalence and size of hiatal hernia. Am J Gastroenterol. 1999;94:2054-2059. [PubMed] [DOI] |
| 28. | Chen YH, Yu HC, Lin KH, Lin HS, Hsu PI. Prevalence and risk factors for Barrett's esophagus in Taiwan. World J Gastroenterol. 2019;25:3231-3241. [PubMed] [DOI] |
| 29. | Eusebi LH, Telese A, Cirota GG, Haidry R, Zagari RM, Bazzoli F, Ford AC. Systematic review with meta-analysis: risk factors for Barrett's oesophagus in individuals with gastro-oesophageal reflux symptoms. Aliment Pharmacol Ther. 2021;53:968-976. [PubMed] [DOI] |
| 30. | Dhawan D, Sharma S. Abdominal Obesity, Adipokines and Non-communicable Diseases. J Steroid Biochem Mol Biol. 2020;203:105737. [PubMed] [DOI] |
| 31. | Usui G, Shinozaki T, Jinno T, Fujibayashi K, Morikawa T, Gunji T, Matsuhashi N. Association between visceral abdominal obesity and long-segment Barrett's esophagus in a Japanese population. J Gastroenterol. 2020;55:189-197. [PubMed] [DOI] |
| 32. | Thrift AP, Kramer JR, Alsarraj A, El-Serag HB. Fat mass by bioelectrical impedance analysis is not associated with increased risk of Barrett esophagus. J Clin Gastroenterol. 2014;48:218-223. [PubMed] [DOI] |
| 33. | Nelsen EM, Kirihara Y, Takahashi N, Shi Q, Lewis JT, Namasivayam V, Buttar NS, Dunagan KT, Prasad GA. Distribution of body fat and its influence on esophageal inflammation and dysplasia in patients with Barrett's esophagus. Clin Gastroenterol Hepatol. 2012;10:728-34; quiz e61-2. [PubMed] [DOI] |
| 34. | Singh S, Sharma AN, Murad MH, Buttar NS, El-Serag HB, Katzka DA, Iyer PG. Central adiposity is associated with increased risk of esophageal inflammation, metaplasia, and adenocarcinoma: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2013;11:1399-1412.e7. [PubMed] [DOI] |
| 35. | Kubo A, Cook MB, Shaheen NJ, Vaughan TL, Whiteman DC, Murray L, Corley DA. Sex-specific associations between body mass index, waist circumference and the risk of Barrett's oesophagus: a pooled analysis from the international BEACON consortium. Gut. 2013;62:1684-1691. [PubMed] [DOI] |
| 36. | Di J, Cheng Y, Chang D, Liu Y. A Meta-Analysis of the Impact of Obesity, Metabolic Syndrome, Insulin Resistance, and Microbiome on the Diagnosis of Barrett's Esophagus. Dig Dis. 2020;38:165-177. [PubMed] [DOI] |
| 37. | Corley DA, Kubo A, Levin TR, Block G, Habel L, Zhao W, Leighton P, Quesenberry C, Rumore GJ, Buffler PA. Abdominal obesity and body mass index as risk factors for Barrett's esophagus. Gastroenterology. 2007;133:34-41; quiz 311. [PubMed] [DOI] |
| 38. | El-Serag HB, Ergun GA, Pandolfino J, Fitzgerald S, Tran T, Kramer JR. Obesity increases oesophageal acid exposure. Gut. 2007;56:749-755. [PubMed] [DOI] |
| 39. | Pandolfino JE, El-Serag HB, Zhang Q, Shah N, Ghosh SK, Kahrilas PJ. Obesity: a challenge to esophagogastric junction integrity. Gastroenterology. 2006;130:639-649. [PubMed] [DOI] |
| 40. | Paris S, Ekeanyanwu R, Jiang Y, Davis D, Spechler SJ, Souza RF. Obesity and its effects on the esophageal mucosal barrier. Am J Physiol Gastrointest Liver Physiol. 2021;321:G335-G343. [PubMed] [DOI] |
| 41. | Ryan AM, Duong M, Healy L, Ryan SA, Parekh N, Reynolds JV, Power DG. Obesity, metabolic syndrome and esophageal adenocarcinoma: epidemiology, etiology and new targets. Cancer Epidemiol. 2011;35:309-319. [PubMed] [DOI] |
| 42. | Kendall BJ, Macdonald GA, Hayward NK, Prins JB, Brown I, Walker N, Pandeya N, Green AC, Webb PM, Whiteman DC; Study of Digestive Health. Leptin and the risk of Barrett's oesophagus. Gut. 2008;57:448-454. [PubMed] [DOI] |
| 43. | Rubenstein JH, Kao JY, Madanick RD, Zhang M, Wang M, Spacek MB, Donovan JL, Bright SD, Shaheen NJ. Association of adiponectin multimers with Barrett's oesophagus. Gut. 2009;58:1583-1589. [PubMed] [DOI] |
| 44. | Zahorska-Markiewicz B, Janowska J, Olszanecka-Glinianowicz M, Zurakowski A. Serum concentrations of TNF-alpha and soluble TNF-alpha receptors in obesity. Int J Obes Relat Metab Disord. 2000;24:1392-1395. [PubMed] [DOI] |
| 45. | Almers LM, Graham JE, Havel PJ, Corley DA. Adiponectin May Modify the Risk of Barrett's Esophagus in Patients With Gastroesophageal Reflux Disease. Clin Gastroenterol Hepatol. 2015;13:2256-64.e1-3. [PubMed] [DOI] |
| 46. | Lee JJ, Sundar KM. Evaluation and Management of Adults with Obstructive Sleep Apnea Syndrome. Lung. 2021;199:87-101. [PubMed] [DOI] |
| 47. | Jaimchariyatam N, Tantipornsinchai W, Desudchit T, Gonlachanvit S. Association between respiratory events and nocturnal gastroesophageal reflux events in patients with coexisting obstructive sleep apnea and gastroesophageal reflux disease. Sleep Med. 2016;22:33-38. [PubMed] [DOI] |
| 48. | Elfanagely Y, Atsawarungruangkit A, Scharfen J, Pavlech L, Moss SF. Association Between Obstructive Sleep Apnea and Barrett's Esophagus: A Systematic Review and Meta-Analysis. Dig Dis Sci. 2021;66:3689-3697. [PubMed] [DOI] |
| 49. | Orr WC, Robert JJ, Houck JR, Giddens CL, Tawk MM. The effect of acid suppression on upper airway anatomy and obstruction in patients with sleep apnea and gastroesophageal reflux disease. J Clin Sleep Med. 2009;5:330-334. [PubMed] |
| 50. | Hadi YB, Khan AA, Naqvi SFZ, Kupec JT. Independent association of obstructive sleep apnea with Barrett's esophagus. J Gastroenterol Hepatol. 2020;35:408-411. [PubMed] [DOI] |
| 51. | Iyer PG, Borah BJ, Heien HC, Das A, Cooper GS, Chak A. Association of Barrett's esophagus with type II Diabetes Mellitus: results from a large population-based case-control study. Clin Gastroenterol Hepatol. 2013;11:1108-1114.e5. [PubMed] [DOI] |
| 52. | Drahos J, Li L, Jick SS, Cook MB. Metabolic syndrome in relation to Barrett's esophagus and esophageal adenocarcinoma: Results from a large population-based case-control study in the Clinical Practice Research Datalink. Cancer Epidemiol. 2016;42:9-14. [PubMed] [DOI] |
| 53. | Petrick JL, Li N, Anderson LA, Bernstein L, Corley DA, El Serag HB, Hardikar S, Liao LM, Liu G, Murray LJ, Rubenstein JH, Schneider JL, Shaheen NJ, Thrift AP, van den Brandt PA, Vaughan TL, Whiteman DC, Wu AH, Zhao WK, Gammon MD, Cook MB. Diabetes in relation to Barrett's esophagus and adenocarcinomas of the esophagus: A pooled study from the International Barrett's and Esophageal Adenocarcinoma Consortium. Cancer. 2019;125:4210-4223. [PubMed] [DOI] |
| 54. | Drahos J, Ricker W, Parsons R, Pfeiffer RM, Warren JL, Cook MB. Metabolic syndrome increases risk of Barrett esophagus in the absence of gastroesophageal reflux: an analysis of SEER-Medicare Data. J Clin Gastroenterol. 2015;49:282-288. [PubMed] [DOI] |
| 55. | Lee SW, Lien HC, Chang CS, Lee TY, Peng YC, Yeh HZ. Association of metabolic syndrome with erosive esophagitis and Barrett's esophagus in a Chinese population. J Chin Med Assoc. 2017;80:15-18. [PubMed] [DOI] |
| 56. | Karimian M, Salamati M, Azami M. The relationship between metabolic syndrome and increased risk of Barrett's esophagus: an updated systematic review and meta-analysis. BMC Gastroenterol. 2020;20:138. [PubMed] [DOI] |
| 57. | Thrift AP, Hilal J, El-Serag HB. Metabolic syndrome and the risk of Barrett's oesophagus in white males. Aliment Pharmacol Ther. 2015;41:1182-1189. [PubMed] [DOI] |
| 58. | Babaei A, Mittal R. Cholecystokinin induces esophageal longitudinal muscle contraction and transient lower esophageal sphincter relaxation in healthy humans. Am J Physiol Gastrointest Liver Physiol. 2018;315:G734-G742. [PubMed] [DOI] |
| 59. | Frysak Z, Schovanek J, Iacobone M, Karasek D. Insulin-like Growth Factors in a clinical setting: Review of IGF-I. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2015;159:347-351. [PubMed] [DOI] |
| 60. | Greer KB, Thompson CL, Brenner L, Bednarchik B, Dawson D, Willis J, Grady WM, Falk GW, Cooper GS, Li L, Chak A. Association of insulin and insulin-like growth factors with Barrett's oesophagus. Gut. 2012;61:665-672. [PubMed] [DOI] |
| 61. | Fallone CA, Chiba N, van Zanten SV, Fischbach L, Gisbert JP, Hunt RH, Jones NL, Render C, Leontiadis GI, Moayyedi P, Marshall JK. The Toronto Consensus for the Treatment of Helicobacter pylori Infection in Adults. Gastroenterology. 2016;151:51-69.e14. [PubMed] [DOI] |
| 62. | Rubenstein JH, Inadomi JM, Scheiman J, Schoenfeld P, Appelman H, Zhang M, Metko V, Kao JY. Association between Helicobacter pylori and Barrett's esophagus, erosive esophagitis, and gastroesophageal reflux symptoms. Clin Gastroenterol Hepatol. 2014;12:239-245. [PubMed] [DOI] |
| 63. | Rajendra S, Ackroyd R, Robertson IK, Ho JJ, Karim N, Kutty KM. Helicobacter pylori, ethnicity, and the gastroesophageal reflux disease spectrum: a study from the East. Helicobacter. 2007;12:177-183. [PubMed] [DOI] |
| 64. | Ackermark P, Kuipers EJ, Wolf C, Breumelhof R, Seldenrijk CA, Timmer R, Segeren KC, Kusters JG, Smout AJ. Colonization with cagA-positive Helicobacter pylori strains in intestinal metaplasia of the esophagus and the esophagogastric junction. Am J Gastroenterol. 2003;98:1719-1724. [PubMed] [DOI] |
| 65. | Wang Z, Shaheen NJ, Whiteman DC, Anderson LA, Vaughan TL, Corley DA, El-Serag HB, Rubenstein JH, Thrift AP. Helicobacter pylori Infection Is Associated With Reduced Risk of Barrett's Esophagus: An Analysis of the Barrett's and Esophageal Adenocarcinoma Consortium. Am J Gastroenterol. 2018;113:1148-1155. [PubMed] [DOI] |
| 66. | Du YL, Duan RQ, Duan LP. Helicobacter pylori infection is associated with reduced risk of Barrett's esophagus: a meta-analysis and systematic review. BMC Gastroenterol. 2021;21:459. [PubMed] [DOI] |
| 67. | Hackelsberger A, Günther T, Schultze V, Peitz U, Malfertheiner P. Role of aging in the expression of Helicobacter pylori gastritis in the antrum, corpus, and cardia. Scand J Gastroenterol. 1999;34:138-143. [PubMed] [DOI] |
| 68. | Kandulski A, Malfertheiner P. Helicobacter pylori and gastroesophageal reflux disease. Curr Opin Gastroenterol. 2014;30:402-407. [PubMed] [DOI] |
| 69. | Doorakkers E, Lagergren J, Santoni G, Engstrand L, Brusselaers N. Helicobacter pylori eradication treatment and the risk of Barrett's esophagus and esophageal adenocarcinoma. Helicobacter. 2020;25:e12688. [PubMed] [DOI] |
| 70. | van Blankenstein M, Looman CW, Johnston BJ, Caygill CP. Age and sex distribution of the prevalence of Barrett's esophagus found in a primary referral endoscopy center. Am J Gastroenterol. 2005;100:568-576. [PubMed] [DOI] |
| 71. | Corley DA, Kubo A, Levin TR, Block G, Habel L, Rumore G, Quesenberry C, Buffler P. Race, ethnicity, sex and temporal differences in Barrett's oesophagus diagnosis: a large community-based study, 1994-2006. Gut. 2009;58:182-188. [PubMed] [DOI] |
| 72. | Ford AC, Forman D, Reynolds PD, Cooper BT, Moayyedi P. Ethnicity, gender, and socioeconomic status as risk factors for esophagitis and Barrett's esophagus. Am J Epidemiol. 2005;162:454-460. [PubMed] [DOI] |
| 73. | Cook MB, Wood SN, Cash BD, Young P, Acosta RD, Falk RT, Pfeiffer RM, Hu N, Su H, Wang L, Wang C, Gherman B, Giffen C, Dykes C, Turcotte V, Caron P, Guillemette C, Dawsey SM, Abnet CC, Hyland PL, Taylor PR. Association between circulating levels of sex steroid hormones and Barrett's esophagus in men: a case-control analysis. Clin Gastroenterol Hepatol. 2015;13:673-682. [PubMed] [DOI] |
| 74. | Adeniyi KO. Gastric acid secretion and parietal cell mass: effect of sex hormones. Gastroenterology. 1991;101:66-69. [PubMed] [DOI] |
| 75. | Locke GR, Zinsmeister AR, Talley NJ. Can symptoms predict endoscopic findings in GERD? Gastrointest Endosc. 2003;58:661-670. [PubMed] [DOI] |
| 76. | Rubenstein JH, Morgenstern H, Appelman H, Scheiman J, Schoenfeld P, McMahon LF, Metko V, Near E, Kellenberg J, Kalish T, Inadomi JM. Prediction of Barrett's esophagus among men. Am J Gastroenterol. 2013;108:353-362. [PubMed] [DOI] |
| 77. | Masclee GM, Coloma PM, de Wilde M, Kuipers EJ, Sturkenboom MC. The incidence of Barrett's oesophagus and oesophageal adenocarcinoma in the United Kingdom and The Netherlands is levelling off. Aliment Pharmacol Ther. 2014;39:1321-1330. [PubMed] [DOI] |
| 79. | Schneider JL, Corley DA. The Troublesome Epidemiology of Barrett's Esophagus and Esophageal Adenocarcinoma. Gastrointest Endosc Clin N Am. 2017;27:353-364. [PubMed] [DOI] |
| 80. | Liu B, Du Y, Wu Y, Snetselaar LG, Wallace RB, Bao W. Trends in obesity and adiposity measures by race or ethnicity among adults in the United States 2011-18: population based study. BMJ. 2021;372:n365. [PubMed] [DOI] |
| 81. | Fahmy N, King JF. Barrett's esophagus: an acquired condition with genetic predisposition. Am J Gastroenterol. 1993;88:1262-1265. [PubMed] |
| 82. | Chak A, Ochs-Balcom H, Falk G, Grady WM, Kinnard M, Willis JE, Elston R, Eng C. Familiality in Barrett's esophagus, adenocarcinoma of the esophagus, and adenocarcinoma of the gastroesophageal junction. Cancer Epidemiol Biomarkers Prev. 2006;15:1668-1673. [PubMed] [DOI] |
| 83. | Chak A, Lee T, Kinnard MF, Brock W, Faulx A, Willis J, Cooper GS, Sivak MV, Goddard KA. Familial aggregation of Barrett's oesophagus, oesophageal adenocarcinoma, and oesophagogastric junctional adenocarcinoma in Caucasian adults. Gut. 2002;51:323-328. [PubMed] [DOI] |
| 84. | Levine DM, Ek WE, Zhang R, Liu X, Onstad L, Sather C, Lao-Sirieix P, Gammon MD, Corley DA, Shaheen NJ, Bird NC, Hardie LJ, Murray LJ, Reid BJ, Chow WH, Risch HA, Nyrén O, Ye W, Liu G, Romero Y, Bernstein L, Wu AH, Casson AG, Chanock SJ, Harrington P, Caldas I, Debiram-Beecham I, Caldas C, Hayward NK, Pharoah PD, Fitzgerald RC, Macgregor S, Whiteman DC, Vaughan TL. A genome-wide association study identifies new susceptibility loci for esophageal adenocarcinoma and Barrett's esophagus. Nat Genet. 2013;45:1487-1493. [PubMed] [DOI] |
| 85. | Palles C, Chegwidden L, Li X, Findlay JM, Farnham G, Castro Giner F, Peppelenbosch MP, Kovac M, Adams CL, Prenen H, Briggs S, Harrison R, Sanders S, MacDonald D, Haigh C, Tucker A, Love S, Nanji M, deCaestecker J, Ferry D, Rathbone B, Hapeshi J, Barr H, Moayyedi P, Watson P, Zietek B, Maroo N, Gay L, Underwood T, Boulter L, McMurtry H, Monk D, Patel P, Ragunath K, Al Dulaimi D, Murray I, Koss K, Veitch A, Trudgill N, Nwokolo C, Rembacken B, Atherfold P, Green E, Ang Y, Kuipers EJ, Chow W, Paterson S, Kadri S, Beales I, Grimley C, Mullins P, Beckett C, Farrant M, Dixon A, Kelly S, Johnson M, Wajed S, Dhar A, Sawyer E, Roylance R, Onstad L, Gammon MD, Corley DA, Shaheen NJ, Bird NC, Hardie LJ, Reid BJ, Ye W, Liu G, Romero Y, Bernstein L, Wu AH, Casson AG, Fitzgerald R, Whiteman DC, Risch HA, Levine DM, Vaughan TL, Verhaar AP, van den Brande J, Toxopeus EL, Spaander MC, Wijnhoven BP, van der Laan LJ, Krishnadath K, Wijmenga C, Trynka G, McManus R, Reynolds JV, O'Sullivan J, MacMathuna P, McGarrigle SA, Kelleher D, Vermeire S, Cleynen I, Bisschops R, Tomlinson I, Jankowski J. Polymorphisms near TBX5 and GDF7 are associated with increased risk for Barrett's esophagus. Gastroenterology. 2015;148:367-378. [PubMed] [DOI] |
| 86. | Becker J, May A, Gerges C, Anders M, Veits L, Weise K, Czamara D, Lyros O, Manner H, Terheggen G, Venerito M, Noder T, Mayershofer R, Hofer JH, Karch HW, Ahlbrand CJ, Arras M, Hofer S, Mangold E, Heilmann-Heimbach S, Heinrichs SK, Hess T, Kiesslich R, Izbicki JR, Hölscher AH, Bollschweiler E, Malfertheiner P, Lang H, Moehler M, Lorenz D, Müller-Myhsok B, Ott K, Schmidt T, Whiteman DC, Vaughan TL, Nöthen MM, Hackelsberger A, Schumacher B, Pech O, Vashist Y, Vieth M, Weismüller J, Neuhaus H, Rösch T, Ell C, Gockel I, Schumacher J. Supportive evidence for FOXP1, BARX1, and FOXF1 as genetic risk loci for the development of esophageal adenocarcinoma. Cancer Med. 2015;4:1700-1704. [PubMed] [DOI] |
| 87. | Kendall BJ, Macdonald GA, Hayward NK, Prins JB, O'Brien S, Whiteman DC; Study of Digestive Health. The risk of Barrett's esophagus associated with abdominal obesity in males and females. Int J Cancer. 2013;132:2192-2199. [PubMed] [DOI] |
| 88. | Cain KK, Flanigan JL, Dalrymple WA, Patrie J, Harrison MB, Barrett MJ. The Effect of Education on Symptom Onset and Severity of Huntington's Disease. Mov Disord Clin Pract. 2021;8:555-562. [PubMed] [DOI] |
| 89. | Wang SE, Kendall BJ, Hodge AM, Dixon-Suen SC, Dashti SG, Makalic E, Williamson EM, Thomas RJS, Giles GG, English DR. Demographic and lifestyle risk factors for gastroesophageal reflux disease and Barrett's esophagus in Australia. Dis Esophagus. 2022;35. [PubMed] [DOI] |
| 90. | Eini-Zinab H, Shoaibinobarian N, Ranjbar G, Norouzian Ostad A, Sobhani SR. Association between the socio-economic status of households and a more sustainable diet. Public Health Nutr. 2021;24:6566-6574. [PubMed] [DOI] |
| 91. | Cook MB, Shaheen NJ, Anderson LA, Giffen C, Chow WH, Vaughan TL, Whiteman DC, Corley DA. Cigarette smoking increases risk of Barrett's esophagus: an analysis of the Barrett's and Esophageal Adenocarcinoma Consortium. Gastroenterology. 2012;142:744-753. [PubMed] [DOI] |
| 92. | Balasubramanian G, Gupta N, Giacchino M, Singh M, Kanakadandi V, Gaddam S, Wani SB, Higbee AD, Rastogi A, Bansal A, Sharma P. Cigarette smoking is a modifiable risk factor for Barrett's oesophagus. United European Gastroenterol J. 2013;1:430-437. [PubMed] [DOI] |
| 93. | Steevens J, Schouten LJ, Driessen AL, Huysentruyt CJ, Keulemans YC, Goldbohm RA, van den Brandt PA. A prospective cohort study on overweight, smoking, alcohol consumption, and risk of Barrett's esophagus. Cancer Epidemiol Biomarkers Prev. 2011;20:345-358. [PubMed] [DOI] |
| 94. | Kadakia SC, Kikendall JW, Maydonovitch C, Johnson LF. Effect of cigarette smoking on gastroesophageal reflux measured by 24-h ambulatory esophageal pH monitoring. Am J Gastroenterol. 1995;90:1785-1790. [PubMed] |
| 95. | Anderson LA, Cantwell MM, Watson RG, Johnston BT, Murphy SJ, Ferguson HR, McGuigan J, Comber H, Reynolds JV, Murray LJ. The association between alcohol and reflux esophagitis, Barrett's esophagus, and esophageal adenocarcinoma. Gastroenterology. 2009;136:799-805. [PubMed] [DOI] |
| 96. | Thrift AP, Kramer JR, Richardson PA, El-Serag HB. No significant effects of smoking or alcohol consumption on risk of Barrett's esophagus. Dig Dis Sci. 2014;59:108-116. [PubMed] [DOI] |
| 97. | Thrift AP, Cook MB, Vaughan TL, Anderson LA, Murray LJ, Whiteman DC, Shaheen NJ, Corley DA. Alcohol and the risk of Barrett's esophagus: a pooled analysis from the International BEACON Consortium. Am J Gastroenterol. 2014;109:1586-1594. [PubMed] [DOI] |
| 98. | Filiberti RA, Fontana V, De Ceglie A, Blanchi S, Grossi E, Della Casa D, Lacchin T, De Matthaeis M, Ignomirelli O, Cappiello R, Rosa A, Foti M, Laterza F, D'Onofrio V, Iaquinto G, Conio M. Alcohol consumption pattern and risk of Barrett's oesophagus and erosive oesophagitis: an Italian case-control study. Br J Nutr. 2017;117:1151-1161. [PubMed] [DOI] |
| 99. | Zhao Z, Yin Z, Zhang C. Lifestyle interventions can reduce the risk of Barrett's esophagus: a systematic review and meta-analysis of 62 studies involving 250,157 participants. Cancer Med. 2021;10:5297-5320. [PubMed] [DOI] |
| 100. | Li N, Petrick JL, Steck SE, Bradshaw PT, McClain KM, Niehoff NM, Engel LS, Shaheen NJ, Corley DA, Vaughan TL, Gammon MD. Dietary sugar/starches intake and Barrett's esophagus: a pooled analysis. Eur J Epidemiol. 2017;32:1007-1017. [PubMed] [DOI] |
| 101. | Dai Q, Cantwell MM, Murray LJ, Zheng W, Anderson LA, Coleman HG; FINBAR study group. Dietary magnesium, calcium:magnesium ratio and risk of reflux oesophagitis, Barrett's oesophagus and oesophageal adenocarcinoma: a population-based case-control study. Br J Nutr. 2016;115:342-350. [PubMed] [DOI] |
| 102. | Filiberti RA, Fontana V, De Ceglie A, Blanchi S, Lacchin T, De Matthaeis M, Ignomirelli O, Cappiello R, Rosa A, D'Onofrio V, Iaquinto G, Conio M. Dietary Habits and Risk of Esophagitis and Barrett's Esophagus: A Multicenter Italian Case-Control Study. Dig Dis Sci. 2021;66:3448-3460. [PubMed] [DOI] |
| 103. | Jiao L, Kramer JR, Chen L, Rugge M, Parente P, Verstovsek G, Alsarraj A, El-Serag HB. Dietary consumption of meat, fat, animal products and advanced glycation end-products and the risk of Barrett's oesophagus. Aliment Pharmacol Ther. 2013;38:817-824. [PubMed] [DOI] |
| 104. | Mulholland HG, Cantwell MM, Anderson LA, Johnston BT, Watson RG, Murphy SJ, Ferguson HR, McGuigan J, Reynolds JV, Comber H, Murray LJ. Glycemic index, carbohydrate and fiber intakes and risk of reflux esophagitis, Barrett's esophagus, and esophageal adenocarcinoma. Cancer Causes Control. 2009;20:279-288. [PubMed] [DOI] |
| 105. | Zhang X, Anandasabapathy S, Abrams J, Othman M, Badr HJ. Lifestyle Risk Factors, Quality of Life, and Intervention Preferences of Barrett's Esophagus Patients: A Prospective Cohort Study. Glob Adv Health Med. 2021;10:21649561211001346. [PubMed] [DOI] |
| 106. | Veugelers PJ, Porter GA, Guernsey DL, Casson AG. Obesity and lifestyle risk factors for gastroesophageal reflux disease, Barrett esophagus and esophageal adenocarcinoma. Dis Esophagus. 2006;19:321-328. [PubMed] [DOI] |
| 107. | Kubo A, Levin TR, Block G, Rumore GJ, Quesenberry CP, Buffler P, Corley DA. Dietary antioxidants, fruits, and vegetables and the risk of Barrett's esophagus. Am J Gastroenterol. 2008;103:1614-23; quiz 1624. [PubMed] [DOI] |
| 108. | Ibiebele TI, Hughes MC, Nagle CM, Bain CJ, Whiteman DC, Webb PM; Study of Digestive Health and Australian Cancer Study. Dietary antioxidants and risk of Barrett's esophagus and adenocarcinoma of the esophagus in an Australian population. Int J Cancer. 2013;133:214-224. [PubMed] [DOI] |
| 109. | De Ceglie A, Fisher DA, Filiberti R, Blanchi S, Conio M. Barrett's esophagus, esophageal and esophagogastric junction adenocarcinomas: the role of diet. Clin Res Hepatol Gastroenterol. 2011;35:7-16. [PubMed] [DOI] |
| 110. | Luo Y, Henle ES, Linn S. Oxidative damage to DNA constituents by iron-mediated fenton reactions. The deoxycytidine family. J Biol Chem. 1996;271:21167-21176. [PubMed] |
| 111. | Barrett MT, Sanchez CA, Prevo LJ, Wong DJ, Galipeau PC, Paulson TG, Rabinovitch PS, Reid BJ. Evolution of neoplastic cell lineages in Barrett oesophagus. Nat Genet. 1999;22:106-109. [PubMed] [DOI] |
| 112. | Corley DA, Kubo A, Levin TR, Habel L, Zhao W, Leighton P, Rumore G, Quesenberry C, Buffler P, Block G. Iron intake and body iron stores as risk factors for Barrett's esophagus: a community-based study. Am J Gastroenterol. 2008;103:2997-3004. [PubMed] [DOI] |
| 113. | Lin D, Kramer JR, Ramsey D, Alsarraj A, Verstovsek G, Rugge M, Parente P, Graham DY, El-Serag HB. Oral bisphosphonates and the risk of Barrett's esophagus: case-control analysis of US veterans. Am J Gastroenterol. 2013;108:1576-1583. [PubMed] [DOI] |
| 114. | Rogers MJ, Crockett JC, Coxon FP, Mönkkönen J. Biochemical and molecular mechanisms of action of bisphosphonates. Bone. 2011;49:34-41. [PubMed] [DOI] |
| 115. | Schneider JL, Zhao WK, Corley DA. Aspirin and nonsteroidal anti-inflammatory drug use and the risk of Barrett's esophagus. Dig Dis Sci. 2015;60:436-443. [PubMed] [DOI] |
| 116. | Beales IL, Dearman L, Vardi I, Loke Y. Reduced Risk of Barrett's Esophagus in Statin Users: Case-Control Study and Meta-Analysis. Dig Dis Sci. 2016;61:238-246. [PubMed] [DOI] |