修回日期: 2017-02-14
接受日期: 2017-02-20
在线出版日期: 2017-04-08
肝细胞癌(hepatocellular carcinoma, HCC)是全球的最常见的肿瘤之一. 虽经持续不懈地根除或改进多种治疗技术, 肝癌患者的预后仍很差. 如何监测肝细胞的恶性转化或早期诊断HCC仍是医学难题. HCC发病机制复杂, 多种致病因素包括乙型肝炎病毒或丙型肝炎病毒的慢性持续感染、脂质积聚和黄曲霉素摄入等致使抗癌基因失活或癌基因复活, 诱发肝细胞癌变; HCC患者的早期筛查有益于延长生存期. 血甲胎蛋白(alpha-fetoprotein, AFP)和肝癌特异性AFP或AFP-L3作为肿瘤标志虽已常规应用, 但他们诊断肝癌仍存在假阳性结果且灵敏度及特异性欠佳. 肝癌的有效治疗取决于早期诊断, 急需研发比较准确有效标志物用于肝癌患者的早期临床分期, 治疗监测与预后判断. 近来, 积累的资料已显示新的血源性标志物如循环血肿瘤细胞, 相关通路关键信号分子、癌胚型特异蛋白、长链非编码RNA和微小RNA对肝癌诊断的潜在价值. 本文述评了肝癌特异诊断相关分子标志发现及其应用前景.
核心提要: 针对外周血甲胎蛋白水平及B超检查, 对小肝癌诊断价值有限, 本文重点评述了近来肝癌相关通路关键信号分子、癌胚型特异蛋白、长链非编码RNA、微小RNA和循环DNA等分子标志, 监测肝细胞恶性转化及特异诊断肝癌技术的研发与临床应用前景.
引文著录: 方淼, 郑文杰, 姚敏, 董志珍, 姚登福. 肝癌特异诊断新标志物发现及其临床应用前景. 世界华人消化杂志 2017; 25(10): 865-873
Revised: February 14, 2017
Accepted: February 20, 2017
Published online: April 8, 2017
Hepatocellular carcinoma (HCC) is one of the most common cancers worldwide. Despite continuous global efforts aimed at HCC eradication and improvements in various treatment techniques, the prognosis of HCC remains very poor. How to monitor malignant transformation of hepatocytes or diagnose HCC at early stage is still a medical challenge. A growing understanding of the multiple pathogenic factors including hepatitis B virus or hepatitis C virus infection, lipid accumulation, aflatoxin B1 intake and so on suggests that hepatocarcinogenesis is a multistep process. A large number of oncogenes or tumor suppressor genes have been identified. Early screening of HCC patients has been reported to confer a survival benefit. Although serum alpha-fetoprotein (AFP) and hepatoma-specific AFP have been used as conventional tumor markers, they often show false-positive results and lack sufficient sensitivity and specificity. In order to provide optimal treatment for each patient with HCC, more precise and effective biomarkers are urgently needed in all phases of management from early detection to staging, treatment monitoring, and prognosis evaluation. Recently, numerous studies have shown the clinical utility of novel blood-based biomarkers, such as circulating tumor cells, key signal molecules or specific proteins, long non-coding RNAs, and microRNAs. In this article, we will review some novel HCC-related biomarkers and discuss their future perspective on clinical applications.
- Citation: Fang M, Zheng WJ, Yao M, Dong ZZ, Yao DF. Novel specific markers for hepatocellular carcinoma: Perspective on clinical applications. Shijie Huaren Xiaohua Zazhi 2017; 25(10): 865-873
- URL: https://www.wjgnet.com/1009-3079/full/v25/i10/865.htm
- DOI: https://dx.doi.org/10.11569/wcjd.v25.i10.865
肝细胞癌(hepatocellular carcinoma, HCC)或肝癌发生的主要病原因素, 除公认的乙型肝炎病毒(hepatitis B virus, HBV)和/或丙型肝炎病毒(hepatitis C virus, HCV)的慢性持续性感染、黄曲霉素及化学致癌物摄入外[1-3], 近几年非酒精性脂肪肝病相关肝癌正在持续增长[4]. 在正常肝细胞发生恶性转化过程中, 上述相关因素致使抗癌基因失活或癌基因复活, 诱发肝细胞发生癌变. 肝癌临床确诊时已中、晚期, 多数丧失根治性切除机会; 即使早期发现肝癌, 以手术切除局部病灶, 但术后复发率高, 预后极差; 综合治疗虽包括血管栓塞、射频、放疗、化疗和生物治疗等, 但在慢性肝病进展为肝癌的过程中多药耐药(multidrug resistance, MDR)的形成, 以及肝癌组织缺氧微环境中新血管生成等因素使治疗效果不佳[5,6]. HCC发病机制复杂, 与多种因素相关, HCC早期诊断极其重要[7,8]. 已知HCC患者的早期筛查有益于延长生存期, 但如何监测肝细胞的恶性转化或早期诊断HCC仍是医学难题. 常规应用的血甲胎蛋白(alpha-fetoprotein, AFP)和肝癌特异性AFP或AFP-L3诊断肝癌仍存在假阳性结果且灵敏度及特异性欠佳. 近来, 积累的资料已显示新的血源性标志物如循环血肿瘤细胞(circulating tumor cell, CTC), 相关通路关键信号分子、癌胚型特异蛋白、长链非编码RNA(long non-coding RNA, lncRNA)和微小RNA(microRNA, miRNA)对肝癌诊断的潜在价值. 本文述评了肝癌特异诊断相关分子标志发现及其应用前景.
近年来, Wnt/β-catenin信号通路研究比较热门, 该通路异常激活与肝癌发生、发展密切相关, 通路中多个关键分子如Wnt家族蛋白, β-catenin和肝癌进展及不良预后相关[9]. 对HCC形成过程中Wnt信号通路关键蛋白的研究尤为重要. Wnt3a是Wnt经典通路的关键蛋白, 其在胚胎发育早期可被激活, 并在干细胞的更新和分化过程中也发挥重要作用, Wnt3a一旦被异常激活后可涉及多种恶性肿瘤的发生发展过程[10,11]. 体外研究发现Wnt3a为重要调节分子, 通过上游的硫酸酯酶-2和磷脂酰肌醇蛋白多糖-3(glypican-3, GPC-3)激活Wnt经典信号通路[12]; 体内研究显示Wnt3a能促进裸鼠皮下肝癌移植瘤的增殖, 可见癌胚性Wnt3a表达可能成为HCC诊断和治疗的潜在分子标记[13].
新发现Wnt3a是肝癌诊断或预后极有应用前景的新标志. 他于胚胎早期激活促进细胞增殖和分化[9]; 成人肝组织Wnt3a失活或低表达. 以组织芯片、免疫组织化学及特异性抗体检测癌及癌周组织, Wnt3a定位于胞浆和细胞膜, 癌组阳性率高达96.3%, 癌周组仅46.3%, 与分化、伴肝硬化、HBV感染和TNM分期均显著相关, 高表达者5年生存率显著降低, 为HCC预后独立预测因素. 肝癌组血Wnt3a约是肝硬化组4.0倍, 慢性肝炎组9.2倍, 健康对照组26.7倍, 与肝硬化、HBV感染、分化程度、TNM分期和肝外转移等显著相关; 诊断肝癌如以800 ng/L为上限时, 其诊断敏感度92.5%、诊断特异度94.3%、诊断准确度93.2%、阳性预测值96.1%和阴性预测值89.3%, 与AFP联检增至96.3%; Wnt3a的受试者工作特征(receive operating characteristic, ROC)曲线下面积为0.99, 显著高于AFP的0.71. 另在肝癌临床各分期中, Wnt3a的阳性度均较高, 显示Wnt通路中关键信号分子Wnt3a表达与肝癌的进展相关, 为肝癌特异诊断和预后标志物[13,14].
GPC-3属硫酸乙酰肝素蛋白聚糖家族的一种66 kDa蛋白, 位于人染色体Xq26.1区, 基因组全长结构>900 kb, 5'端朝向端粒区, 3'端朝向中心粒区, 由8个外显子和7个内含子组成, 启动子区有许多转录因子结合位点, 包括6个SP1结构, 7个AP2结构, 2个CAAT盒, 产生2130 bp的转录子, 编码含580个氨基酸残基的GPC-3蛋白质前体. 羧基端与糖基磷脂酰肌醇共价结合而锚定于细胞膜上, 氨基端游离于胞外, 以多个二硫键连接, 具球形立体结构, 蛋白聚糖由核心蛋白和糖胺聚糖(glycosaminoglycans, GAG)侧链构成, GAG侧链为肝素和硫酸乙酰肝素, 后者插入位点由羧基端50个氨基酸残基决定, 使该链靠近细胞膜, 分布于细胞表面和胞外基质[15]. 此外, GPC-3的氨基末端在A358和S359间被切开而获得一种分泌型信号蛋白. 新近发现GPC-3可通过调控Wnts、Hhs信号通路、成纤维生长因子、骨形态发生蛋白、Suifatase、胰岛素样生长因子Ⅱ在肿瘤增殖和分化中起重要作用. GPC-3在Wnt信号通路中发挥促进作用, 促进Wnt与受体蛋白Frizzled结合, 激活Wnt信号通路, 同时在Hh信号通路中发挥抑制作用, 与Patched竞争结合Hh, 阻断信号触发器Patched与Smoothened的结合, 导致Hh内吞和降解, 而抑制Hh信号通路[12,16].
胎肝组织中GPC-3高表达, 正常肝组织中无表达, 肝癌组织中GPC-3呈过表达状态; 肝癌动态发生模型显示[17]: 肝细胞恶性转化过程中GPC-3 mRNA呈进行性增高表达, 肝细胞变性组阳性率达83.3%, 癌前病变组和癌变组均为100%. 人肝癌与良性肝组织GPC-3呈极明显的差异表达; HCV感染后肝硬化患者<2 cm小肝癌组织GPC-3表达率100%, 其他良性肝病和正常肝组织均未见表达. 综合文献发现癌组织GPC-3表达率达81.5%, 癌旁及远癌组织无表达; 以组织芯片分析癌组织GPC-3表达, 在伴肝硬化背景癌组织阳性率为90%, 而无肝硬化背景的癌组织阳性率为64%; 肝腺瘤组织阳性率为48%, 良性结节阳性率仅3%, 据此区分良性结节、肝腺瘤和肝癌, 显示GPC-3是肝癌早期诊断标志物, 其敏感性69%, 特异性91%. 癌胚型GPC-3促肝癌形成, 其表达为肝癌早期诊断敏感、特异的分子标志物[18-20], 且高表达患者预后差[21].
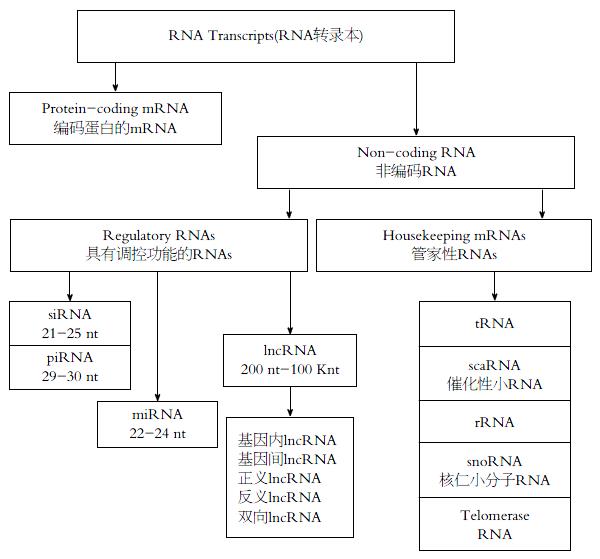
非编码miRNAs由22-24个核苷酸组成(图1), 已报道的超过1000多种, 可分为致癌和抑癌性miRNAs, 他参与胚胎发育, 细胞增殖、分化和凋亡等过程, 转录后可调节相关基因表达, 在干细胞分化、新血管生成、癌细胞浸润与转移过程中发挥作用. 癌组织及循环血miRNAs表达异常, 在肝癌筛查、诊断、监测、治疗和预后评估中具有一定临床价值[22-24]. 致癌miRNAs在肝癌组织及患者循环血中高表达, 其作用类似于癌基因如miR-155、miR-221、miR-222、miR-21和miR-106a过表达, 可促进癌细胞侵袭与转移、加速细胞周期及抗凋亡; 抑癌性miRNAs在正常肝组织中过表达, 其作用类似于抑癌基因如miR-222、miR-126和miR-375等[25,26]. 提示外周血及组织中miRNAs在肝癌致病因素中起关键作用, 如影响多种重要的信号通路如p53、p21、PTEN、PI3K-AKT、c-Myc和STAT3[27,28].
积累的报道显示有多种miRNAs用于肝癌诊断, 然而其阳性率差异颇大, 多数为广谱性肿瘤标志, 对肝癌诊断缺乏特异性[29,30]. 如在HBV相关性肝癌, 血液中miR-490-3p、miR-155-5p、miR-210-3、pmiR-24-3p和miR-335-5p表达明显异常, 发现miR-24-3p异常与肝癌发生血管浸润相关, 诊断肝癌的受试者工作ROC曲线下面积为0.63, 与血AFP联检的ROC为0.83; 然而对48份配对的肝癌与癌周组织miRNAs表达的丰度分析, 发现总共有33种miRNAs异常, 其中5种表达上调(miR-182、miR-183、miR-10b、miR-21和miR-452), 28种表达下调, 占84.8%; 依据33种miRNAs的表达谱型, 评价48对配对癌与非癌组织的灵敏度为91.7%, 特异性为100%, 阴性预测值为92.3%, 阳性预测值100%, 判别准确率95.8%和错判率4.1%; 同样以该谱型评价302例非配对癌与非癌组的灵敏度为99.0%, 特异性为97.9%, 阳性预测值为99.7%, 阴性预测值为94.0%, 判别准确率98.5%而错判率仅1.5%[31,32]; 血清microRNA classifier有助于亚临床肝癌的诊断[33], 优于AFP, 具有一定的临床应用前景.
lncRNA是近来肝癌研究的一个全新热点[34,35], 约占80%非编码RNA的lncRNA为200-100k nt的RNA分子位于细胞浆或细胞核内(图1), 可进一步分为: 基因内lncRNA、基因间lncRNA、正义lncRNA、反义lncRNA和双向lncRNA, 由RNA聚合酶Ⅱ转录, 与编码蛋白的mRNA异同, lncRNA不具备典型的启始密码子、启动子保守区、开放阅读框及终止密码子, 不具编码蛋白功能, 或仅能编码100个氨基多肽, 在表观遗传、转录及转录后等方面调控基因表达, 广泛参与肝癌发生、进展, 机制极其复杂[36,37]. 对肝癌发生起促进作用的lncRNAs称为"促癌lncRNA", 呈增加表达对肝癌进展起促进作用, 与内皮细胞间质转化、增殖、转移等密切相关; 对肝癌发生起抑制作用的lncRNA称为"抑癌lncRNA", 表达减少抑癌作用逐步变小, 与患者预后等密切相关. 正常肝脏促癌lncRNA和抑癌lncRNA共同参与细胞增殖和分化调节, 两者处于平衡状态, 然而在促癌因子的作用下这种平衡状态被打破[38,39].
对HBV和HCV相关肝癌lncRNA差异表达分析, 显示101种lncRNA, 鉴定出癌与癌周组明显差异的新lncRNA, 如肝炎病毒感染特异lncRNA: 如与HBV相关HCC的PCAT-29、与HCV相关HCC的aHIF和PAR5, 与HDV相关HCC则为Y3, 而BC017743、BC043430和LINCO1152 3种lncRNA则在不同致病因素的肝癌组织中同时表达[40]. HCC患者肝癌高表达转录本HULC明显高于健康组, 同时在EdmondsonⅢ-Ⅳ级和HBV-HCC患者血表达较高, ROC曲线下面积达0.86. HCC患者血lncRNA-uc003wbd和lncRNA-AF085935明显高于健康组, ROC分别为0.96和0.86[41]. 对lncRNA-TCF7(lncRNA termed TCF7)以健康者为参考, 肝硬化正常, 瘤旁及HCC组分别增高5、100倍[42]. 对81例HCC患者SRHC癌组织明显低于癌旁组, 在AFP≥20 μg/L的HCC患者SRHC高表达组与低表达间差异明显[43], 提示某些特异型lncRNA可作为肝癌诊断的新分子标志物, 但仍有待大样本的临床研究[44,45].
液体活检主要包括循环DNA、肿瘤细胞及外泌体检测, 是MIT Technology Review发布的十大突破技术(2015), 通过分析血、尿或唾液等标本中游离CTC、循环肿瘤DNA(circulating tumor DNA, ctDNA)、小分子RNA及lncRNA等辅助诊断肝癌[46,47]. 与组织活检相比具有创伤小、可重复、均化异质性、实时判断疗效, 动态观察肝癌发展而指导个性化用药等优点[48]. 尽管CTC发现已100多年, 但近期用于HCC诊断的文献较多(表1), CTC诊断阳性率变化范围较大(22%-100%)[49-57]; 从癌细胞遗落信息或死亡残骸中探寻变异密码[58], 正成为肝癌诊断的前沿热点. 所捕获的游离核酸反映患者信息, 蕴藏着广阔的诊断应用前景, 然而该技术尚未发挥实质性作用[59,60].
| 文献 | n | 患者构成 | 患者背景 | 对照组构成 | 检测方法 | 阳性率(%) |
| Choi等[49]2015 | 81 | 80%乙型肝炎; 11%丙型肝炎; 4%酒精性; 59%伴肝硬化 | 手术64, 肝移植17 | 16例肝功能正常志愿者 | RT-PCR(K19, CD44) | 22.2 |
| Fang等[50]2014 | 42 | 55%伴肝硬化 | 术前/术后、TACE | 20例(健康10例, 良性肝病10例) | CellSearchTM | 52.3 |
| Guo等[51]2014 | 299 | 乙型肝炎90%, 90%伴肝硬化 | 手术157, TACE 76, 射频消融术66 | 120例(健康71例, 良性肝病25例, 良性肿瘤24例) | CellSearchTM | 42.6 |
| Li等[52]2014 | 27 | 未显示 | 未显示 | 61例(良性肝病34例, 健康15例, 非肝肿瘤12例) | CellSearchTM | 88.9 |
| Morris等[53]2014 | 52 | 38%酒精性, 乙型肝炎占8%, 糖尿病占12% | 未治疗 | 未显示 | CellSearchTM ISET | 28.0 |
| 100.0 | ||||||
| Mu等[54]2014 | 62 | 乙型肝炎占95.2% | 未显示 | 22例(良性肝病7例, 健康15例) | CellSearchTM | 48.3 |
| Kelley等[55]2015 | 20 | 乙型肝炎25%, 丙型肝炎45%, 乙+丙10%; 酒精性5%; 非酒精性脂肪肝10% | 未显示 | 10例(良性肝病) | CellSearchTM | 40.0 |
| Wang等[56]2016 | 42 | 乙型肝炎: 81%, 丙型肝炎: 2%, 非乙非丙: 17% | 未显示 | 未显示 | CTC-Chip | 59.5 |
| Zhang等[57]2016 | 36 | 未显示 | 未显示 | 未显示 | CTC-Chip | 100.0 |
肝癌发生机制极其复杂, 早期诊断和如何监测肝细胞恶性转化仍是医学难题, 且有效治疗取决于早期准确诊断[61,62]. 晚期肝癌加之MDR形成, 使放化疗、介入与手术等作用有限[63,64]. 综上所述, 尽管肝癌早期准确诊断的相关标志研究已取得显著进步, Wnt信号通路关键分子Wnt3a及上游GPC-3浓度异常, 有助于肝癌诊断和良、恶性肝病的鉴别; 但临床应用亟待解决的问题仍较多, 如miRNA、lncRNA和ctDNA命名混乱, 虽创伤小、可重复, 非人内参兼容/可比性差, 需统一检测样本; ctDNA及GPC-3特异性好, 但敏感性需提高, 仍须大样本、多中心验证. 随着基因沉默、置换、增补、矫正、分子剪接、靶向干预和单抗封闭相关信号分子或作为放射性核素、药物和毒素等载体及免疫治疗等应用[65,66], 特异分子标志物除诊断外, 如以此为靶点与手术、介入、化疗或放疗等结合, 在改善患者疗效, 延长患者存活时间方面具有应用前景[67,68].
肝细胞癌(hepato-cellular carcinoma, HCC)仍是全球常见恶性肿瘤之一, 其发病率及死亡率持续增长. 肝癌发生机制复杂, 早期诊断和如何监测肝细胞恶性转化仍是医学难题, 且有效治疗取决于早期准确诊断. 晚期肝癌加之多药耐药形成, 放化疗、介入与手术等作用有限.
肝癌的早期诊断及有效治疗是医学难题, 其有效治疗取决于肝癌的早期发现. 外周血甲胎蛋白(alpha-fetoprotein, AFP)水平及B超检查, 对小肝癌诊断价值有限, 肝癌防治重点仍是早期特异诊断与有效治疗技术的研发.
Pan等发现肝癌患者Wnt3a表达明显异常, 如以800 ng/L为限诊断肝癌的敏感度、特异度、准确度、阳性预测值和阴性预测值均在90%左右, 与AFP联检达96%; 经受试者工作曲线证实, 明显优于AFP, 为肝癌早期特异诊断最有前景的新标志物.
针对AFP水平诊断早期肝癌的限制, 重点评述了近期肝癌相关通路关键信号分子Wnt3a、循环血肿瘤细胞、LncNA、miRNA和循环肿瘤DNA(circulating tumor DNA, ctDNA)等分子标志, 监测肝细胞恶性转化及特异诊断肝癌技术的研发与临床应用前景.
尽管肝癌准确诊断相关标志如Wnt3a及GPC-3异常有助于肝癌诊断和良、恶性肝病鉴别; 但miRNA、lncRNA和ctDNA临床应用亟待解决统一命名, 统一样本, 内参等; ctDNA及GPC-3虽特异但敏感性差, 且须大样本多中心验证.
刘亮, 副主任医师, 复旦大学胰腺癌研究所; 复旦大学附属肿瘤医院胰腺肝胆外科; 王阁, 教授, 中国人民解放军第三军医大学第三附属医院
本文综述了HCC目前新的分子诊断标志物及临床应用, 文献量大, 有一定的可读性.
手稿来源: 邀请约稿
学科分类: 胃肠病学和肝病学
手稿来源地: 江苏省
同行评议报告分类
A级 (优秀): 0
B级 (非常好): B
C级 (良好): C
D级 (一般): 0
E级 (差): 0
编辑: 闫晋利 电编:胡珊
| 1. | Lamontagne RJ, Bagga S, Bouchard MJ. Hepatitis B virus molecular biology and pathogenesis. Hepatoma Res. 2016;2:163-186. [PubMed] [DOI] |
| 2. | Chacko S, Samanta S. "Hepatocellular carcinoma: A life-threatening disease". Biomed Pharmacother. 2016;84:1679-1688. [PubMed] [DOI] |
| 3. | Manthravadi S, Paleti S, Pandya P. Impact of sustained viral response postcurative therapy of hepatitis C-related hepatocellular carcinoma: a systematic review and meta-analysis. Int J Cancer. 2017;140:1042-1049. [PubMed] [DOI] |
| 4. | Bellentani S. The epidemiology of non-alcoholic fatty liver disease. Liver Int. 2017;37 Suppl 1:81-84. [PubMed] [DOI] |
| 5. | Nuño Solinís R, Arratibel Ugarte P, Rojo A, Sanchez Gonzalez Y. Value of Treating All Stages of Chronic Hepatitis C: A Comprehensive Review of Clinical and Economic Evidence. Infect Dis Ther. 2016;5:491-508. [PubMed] [DOI] |
| 6. | Choi SH, Park JY. Regulation of the hypoxic tumor environment in hepatocellular carcinoma using RNA interference. Cancer Cell Int. 2017;17:3. [PubMed] [DOI] |
| 7. | Kirstein MM, Vogel A. The pathogenesis of hepatocellular carcinoma. Dig Dis. 2014;32:545-553. [PubMed] [DOI] |
| 8. | Lee H, Yoon JH, Kim H, Yi NJ, Hong SK, Yoon KC, Kim HS, Ahn SW, Choi JY, Choi Y. False Positive Diagnosis of Hepatocellular Carcinoma in Liver Resection Patients. J Korean Med Sci. 2017;32:315-320. [PubMed] [DOI] |
| 9. | Duchartre Y, Kim YM, Kahn M. The Wnt signaling pathway in cancer. Crit Rev Oncol Hematol. 2016;99:141-149. [PubMed] [DOI] |
| 10. | Gao C, Xiao G, Hu J. Regulation of Wnt/β-catenin signaling by posttranslational modifications. Cell Biosci. 2014;4:13. [PubMed] [DOI] |
| 11. | Huang S, Xie Y, Yang P, Chen P, Zhang L. HCV core protein-induced down-regulation of microRNA-152 promoted aberrant proliferation by regulating Wnt1 in HepG2 cells. PLoS One. 2014;9:e81730. [PubMed] [DOI] |
| 12. | Yao M, Wang L, Fang M, Zheng W, Dong Z, Yao D. Advances in the study of oncofetal antigen glypican-3 expression in HBV-related hepatocellular carcinoma. Biosci Trends. 2016;10:337-343. [PubMed] [DOI] |
| 13. | Pan L, Yao M, Zheng W, Gu J, Yang X, Qiu L, Cai Y, Wu W, Yao D. Abnormality of Wnt3a expression as novel specific biomarker for diagnosis and differentiation of hepatocellular carcinoma. Tumour Biol. 2016;37:5561-5568. [PubMed] [DOI] |
| 14. | Pan LH, Yao M, Cai Y, Gu JJ, Yang XL, Wang L, Yao DF. Oncogenic Wnt3a expression as an estimable prognostic marker for hepatocellular carcinoma. World J Gastroenterol. 2016;22:3829-3836. [PubMed] [DOI] |
| 15. | Wu Y, Liu H, Ding H. GPC-3 in hepatocellular carcinoma: current perspectives. J Hepatocell Carcinoma. 2016;3:63-67. [PubMed] [DOI] |
| 16. | Dong Z, Yao M, Wang L, Yang J, Yao D. Down-regulating glypican-3 expression: molecular-targeted therapy for hepatocellular carcinoma. Mini Rev Med Chem. 2014;14:1183-1193. [PubMed] [DOI] |
| 17. | Yao M, Yao DF, Bian YZ, Zhang CG, Qiu LW, Wu W, Sai WL, Yang JL, Zhang HJ. Oncofetal antigen glypican-3 as a promising early diagnostic marker for hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int. 2011;10:289-294. [PubMed] [DOI] |
| 18. | Yao M, Pan LH, Yao DF. Glypican-3 as a specific biomarker for hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int. 2015;14:122-123. [PubMed] [DOI] |
| 19. | Yao M, Wang L, Dong Z, Qian Q, Shi Y, Yu D, Wang S, Zheng W, Yao D. Glypican-3 as an emerging molecular target for hepatocellular carcinoma gene therapy. Tumour Biol. 2014;35:5857-5868. [PubMed] [DOI] |
| 20. | Yao M, Yao DF, Bian YZ, Wu W, Yan XD, Yu DD, Qiu LW, Yang JL, Zhang HJ, Sai WL. Values of circulating GPC-3 mRNA and alpha-fetoprotein in detecting patients with hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int. 2013;12:171-179. [PubMed] [DOI] |
| 21. | Brückner L. Diabetic osteoarthropathy--not a primary indication for amputation. Zentralbl Chir. 1989;114:241-252. [PubMed] [DOI] |
| 22. | Xu J, Li J, Zheng TH, Bai L, Liu ZJ. MicroRNAs in the Occurrence and Development of Primary Hepatocellular Carcinoma. Adv Clin Exp Med. 2016;25:971-975. [PubMed] [DOI] |
| 23. | Shen S, Lin Y, Yuan X, Shen L, Chen J, Chen L, Qin L, Shen B. Biomarker MicroRNAs for Diagnosis, Prognosis and Treatment of Hepatocellular Carcinoma: A Functional Survey and Comparison. Sci Rep. 2016;6:38311. [PubMed] [DOI] |
| 24. | Reichl P, Mikulits W. Accuracy of novel diagnostic biomarkers for hepatocellular carcinoma: An update for clinicians (Review). Oncol Rep. 2016;36:613-625. [PubMed] [DOI] |
| 25. | Fiorino S, Bacchi-Reggiani ML, Visani M, Acquaviva G, Fornelli A, Masetti M, Tura A, Grizzi F, Zanello M, Mastrangelo L. MicroRNAs as possible biomarkers for diagnosis and prognosis of hepatitis B- and C-related-hepatocellular-carcinoma. World J Gastroenterol. 2016;22:3907-3936. [PubMed] [DOI] |
| 26. | Wang L, Yue Y, Wang X, Jin H. Function and clinical potential of microRNAs in hepatocellular carcinoma. Oncol Lett. 2015;10:3345-3353. [PubMed] [DOI] |
| 27. | Mirzaei HR, Sahebkar A, Mohammadi M, Yari R, Salehi H, Jafari MH, Namdar A, Khabazian E, Jaafari MR, Mirzaei H. Circulating microRNAs in Hepatocellular Carcinoma: Potential Diagnostic and Prognostic Biomarkers. Curr Pharm Des. 2016;22:5257-5269. [PubMed] [DOI] |
| 28. | Lee CH, Kim JH, Lee SW. The Role of MicroRNA in Pathogenesis and as Markers of HCV Chronic Infection. Curr Drug Targets. 2016; Apr 1. [Epub ahead of print]. [PubMed] [DOI] |
| 29. | He S, Hu XW, Wang D, Han LF, Zhang DC, Wei C. Accuracy of microRNAs for the diagnosis of hepatocellular carcinoma: A systematic review and meta-analysis. Clin Res Hepatol Gastroenterol. 2016;40:405-417. [PubMed] [DOI] |
| 30. | Afonso MB, Rodrigues PM, Simão AL, Castro RE. Circulating microRNAs as Potential Biomarkers in Non-Alcoholic Fatty Liver Disease and Hepatocellular Carcinoma. J Clin Med. 2016;5:pii E30. [PubMed] [DOI] |
| 31. | Shen J, Siegel AB, Remotti H, Wang Q, Santella RM. Identifying microRNA panels specifically associated with hepatocellular carcinoma and its different etiologies. Hepatoma Res. 2016;2:151-162. [DOI] |
| 32. | Huang JT, Liu SM, Ma H, Yang Y, Zhang X, Sun H, Zhang X, Xu J, Wang J. Systematic Review and Meta-Analysis: Circulating miRNAs for Diagnosis of Hepatocellular Carcinoma. J Cell Physiol. 2016;231:328-335. [PubMed] [DOI] |
| 33. | Lin XJ, Chong Y, Guo ZW, Xie C, Yang XJ, Zhang Q, Li SP, Xiong Y, Yuan Y, Min J. A serum microRNA classifier for early detection of hepatocellular carcinoma: a multicentre, retrospective, longitudinal biomarker identification study with a nested case-control study. Lancet Oncol. 2015;16:804-815. [PubMed] [DOI] |
| 34. | Liu YR, Tang RX, Huang WT, Ren FH, He RQ, Yang LH, Luo DZ, Dang YW, Chen G. Long noncoding RNAs in hepatocellular carcinoma: Novel insights into their mechanism. World J Hepatol. 2015;7:2781-2791. [PubMed] [DOI] |
| 35. | Li C, Chen J, Zhang K, Feng B, Wang R, Chen L. Progress and Prospects of Long Noncoding RNAs (lncRNAs) in Hepatocellular Carcinoma. Cell Physiol Biochem. 2015;36:423-434. [PubMed] [DOI] |
| 36. | Yang X, Xie X, Xiao YF, Xie R, Hu CJ, Tang B, Li BS, Yang SM. The emergence of long non-coding RNAs in the tumorigenesis of hepatocellular carcinoma. Cancer Lett. 2015;360:119-124. [PubMed] [DOI] |
| 37. | Huang JL, Zheng L, Hu YW, Wang Q. Characteristics of long non-coding RNA and its relation to hepatocellular carcinoma. Carcinogenesis. 2014;35:507-514. [PubMed] [DOI] |
| 38. | Zhang Q, Matsuura K, Kleiner DE, Zamboni F, Alter HJ, Farci P. Analysis of long noncoding RNA expression in hepatocellular carcinoma of different viral etiology. J Transl Med. 2016;14:328. [PubMed] [DOI] |
| 39. | Gong X, Wei W, Chen L, Xia Z, Yu C. Comprehensive analysis of long non-coding RNA expression profiles in hepatitis B virus-related hepatocellular carcinoma. Oncotarget. 2016;7:42422-42430. [PubMed] [DOI] |
| 40. | Zhu J, Liu S, Ye F, Shen Y, Tie Y, Zhu J, Jin Y, Zheng X, Wu Y, Fu H. The long noncoding RNA expression profile of hepatocellular carcinoma identified by microarray analysis. PLoS One. 2014;9:e101707. [PubMed] [DOI] |
| 41. | Lu J, Xie F, Geng L, Shen W, Sui C, Yang J. Investigation of serum lncRNA-uc003wbd and lncRNA-AF085935 expression profile in patients with hepatocellular carcinoma and HBV. Tumour Biol. 2015;36:3231-3236. [PubMed] [DOI] |
| 42. | Wang Y, He L, Du Y, Zhu P, Huang G, Luo J, Yan X, Ye B, Li C, Xia P. The long noncoding RNA lncTCF7 promotes self-renewal of human liver cancer stem cells through activation of Wnt signaling. Cell Stem Cell. 2015;16:413-425. [PubMed] [DOI] |
| 43. | Zheng H, Yang S, Yang Y, Yuan SX, Wu FQ, Wang LL, Yan HL, Sun SH, Zhou WP. Epigenetically silenced long noncoding-SRHC promotes proliferation of hepatocellular carcinoma. J Cancer Res Clin Oncol. 2015;141:1195-1203. [PubMed] [DOI] |
| 44. | He Y, Meng XM, Huang C, Wu BM, Zhang L, Lv XW, Li J. Long noncoding RNAs: Novel insights into hepatocelluar carcinoma. Cancer Lett. 2014;344:20-27. [PubMed] [DOI] |
| 45. | Qu Z, Yuan CH, Yin CQ, Guan Q, Chen H, Wang FB. Meta-analysis of the prognostic value of abnormally expressed lncRNAs in hepatocellular carcinoma. Onco Targets Ther. 2016;9:5143-5152. [PubMed] [DOI] |
| 46. | Zhou J, Huang A, Yang XR. Liquid Biopsy and its Potential for Management of Hepatocellular Carcinoma. J Gastrointest Cancer. 2016;47:157-167. [PubMed] [DOI] |
| 47. | Tang JC, Feng YL, Guo T, Xie AY, Cai XJ. Circulating tumor DNA in hepatocellular carcinoma: trends and challenges. Cell Biosci. 2016;6:32. [PubMed] [DOI] |
| 48. | Su YH, Lin SY, Song W, Jain S. DNA markers in molecular diagnostics for hepatocellular carcinoma. Expert Rev Mol Diagn. 2014;14:803-817. [PubMed] [DOI] |
| 49. | Choi GH, Kim GI, Yoo JE, Na DC, Han DH, Roh YH, Park YN, Choi JS. Increased Expression of Circulating Cancer Stem Cell Markers During the Perioperative Period Predicts Early Recurrence After Curative Resection of Hepatocellular Carcinoma. Ann Surg Oncol. 2015;22 Suppl 3:S1444-S1452. [PubMed] [DOI] |
| 50. | Fang ZT, Zhang W, Wang GZ, Zhou B, Yang GW, Qu XD, Liu R, Qian S, Zhu L, Liu LX. Circulating tumor cells in the central and peripheral venous compartment - assessing hematogenous dissemination after transarterial chemoembolization of hepatocellular carcinoma. Onco Targets Ther. 2014;7:1311-1318. [PubMed] [DOI] |
| 51. | Guo W, Yang XR, Sun YF, Shen MN, Ma XL, Wu J, Zhang CY, Zhou Y, Xu Y, Hu B. Clinical significance of EpCAM mRNA-positive circulating tumor cells in hepatocellular carcinoma by an optimized negative enrichment and qRT-PCR-based platform. Clin Cancer Res. 2014;20:4794-4805. [PubMed] [DOI] |
| 52. | Li J, Chen L, Zhang X, Zhang Y, Liu H, Sun B, Zhao L, Ge N, Qian H, Yang Y. Detection of circulating tumor cells in hepatocellular carcinoma using antibodies against asialoglycoprotein receptor, carbamoyl phosphate synthetase 1 and pan-cytokeratin. PLoS One. 2014;9:e96185. [PubMed] [DOI] |
| 53. | Morris KL, Tugwood JD, Khoja L, Lancashire M, Sloane R, Burt D, Shenjere P, Zhou C, Hodgson C, Ohtomo T. Circulating biomarkers in hepatocellular carcinoma. Cancer Chemother Pharmacol. 2014;74:323-332. [PubMed] [DOI] |
| 54. | Mu H, Lin KX, Zhao H, Xing S, Li C, Liu F, Lu HZ, Zhang Z, Sun YL, Yan XY. Identification of biomarkers for hepatocellular carcinoma by semiquantitative immunocytochemistry. World J Gastroenterol. 2014;20:5826-5838. [PubMed] [DOI] |
| 55. | Kelley RK, Magbanua MJ, Butler TM, Collisson EA, Hwang J, Sidiropoulos N, Evason K, McWhirter RM, Hameed B, Wayne EM. Circulating tumor cells in hepatocellular carcinoma: a pilot study of detection, enumeration, and next-generation sequencing in cases and controls. BMC Cancer. 2015;15:206. [PubMed] [DOI] |
| 56. | Wang S, Zhang C, Wang G, Cheng B, Wang Y, Chen F, Chen Y, Feng M, Xiong B. Aptamer-Mediated Transparent-Biocompatible Nanostructured Surfaces for Hepotocellular Circulating Tumor Cells Enrichment. Theranostics. 2016;6:1877-1886. [PubMed] [DOI] |
| 57. | Zhang Y, Zhang X, Zhang J, Sun B, Zheng L, Li J, Liu S, Sui G, Yin Z. Microfluidic chip for isolation of viable circulating tumor cells of hepatocellular carcinoma for their culture and drug sensitivity assay. Cancer Biol Ther. 2016;17:1177-1187. [PubMed] [DOI] |
| 58. | Zhang Y, Li J, Cao L, Xu W, Yin Z. Circulating tumor cells in hepatocellular carcinoma: detection techniques, clinical implications, and future perspectives. Semin Oncol. 2012;39:449-460. [PubMed] [DOI] |
| 59. | Zhou J, Shi YH, Fan J. Circulating cell-free nucleic acids: promising biomarkers of hepatocellular carcinoma. Semin Oncol. 2012;39:440-448. [PubMed] [DOI] |
| 60. | Wu LJ, Pan YD, Pei XY, Chen H, Nguyen S, Kashyap A, Liu J, Wu J. Capturing circulating tumor cells of hepatocellular carcinoma. Cancer Lett. 2012;326:17-22. [PubMed] [DOI] |
| 61. | Kamimura K, Kobayashi Y, Takahashi Y, Abe H, Kumaki D, Yokoo T, Kamimura H, Sakai N, Sakamaki A, Abe S. Tumor markers for early diagnosis for brain metastasis of hepatocellular carcinoma: A case series and literature review for effective loco-regional treatment. Cancer Biol Ther. 2017;18:79-84. [PubMed] [DOI] |
| 62. | Sia D, Villanueva A, Friedman SL, Llovet JM. Liver Cancer Cell of Origin, Molecular Class, and Effects on Patient Prognosis. Gastroenterology. 2017;152:745-761. [PubMed] [DOI] |
| 63. | Yuan BH, Li RH, Yuan WP, Yang T, Tong TJ, Peng NF, Li LQ, Zhong JH. Harms and benefits of adoptive immunotherapy for postoperative hepatocellular carcinoma: an updated review. Oncotarget. 2017; Jan 4. [Epub ahead of print]. [PubMed] [DOI] |
| 64. | Raoul JL, Adhoute X, Gilabert M, Edeline J. How to assess the efficacy or failure of targeted therapy: Deciding when to stop sorafenib in hepatocellular carcinoma. World J Hepatol. 2016;8:1541-1546. [PubMed] [DOI] |
| 65. | Sapisochin G, Bruix J. Liver transplantation for hepatocellular carcinoma: outcomes and novel surgical approaches. Nat Rev Gastroenterol Hepatol. 2017; Jan 5. [Epub ahead of print]. [PubMed] [DOI] |
| 66. | Li G, Staveley-O'Carroll KF, Kimchi ET. Potential of Radiofrequency Ablation in Combination with Immunotherapy in the Treatment of Hepatocellular Carcinoma. J Clin Trials. 2016;6:pii257. [PubMed] [DOI] |
| 67. | Farrell C, Halpen A, Cross TJ, Richardson PD, Johnson P, Joekes EC. Ultrasound surveillance for hepatocellular carcinoma: service evaluation of a radiology-led recall system in a tertiary-referral centre for liver diseases in the UK. Clin Radiol. 2017;72:338.e11-338.e17. [PubMed] [DOI] |
| 68. | Giovannini C, Bolondi L, Gramantieri L. Targeting Notch3 in Hepatocellular Carcinoma: Molecular Mechanisms and Therapeutic Perspectives. Int J Mol Sci. 2016;18:pii E56. [PubMed] [DOI] |