Copyright
©The Author(s) 2003. Published by Baishideng Publishing Group Inc. All rights reserved.
幽门螺杆菌对克拉霉素耐药的分子基础
郝庆, 李岩, 高红, 张显忠
郝庆, 李岩, 中国医科大学附属二院消化科 辽宁省沈阳市 110004
郝庆, 女, 1969-11-20生, 辽宁省沈阳市人, 汉族. 1993年中国医科大学本科毕业, 1998年中国医科大学硕士毕业, 2002年博士毕业, 讲师, 主要从事中药与胃肠动力及幽门螺杆菌耐药机制方面的研究.
高红, 中国医科大学附属二院卫生部先天畸形重点实验室辽宁省沈阳市 110004
张显忠, 沈阳市红十字会医院消化科 辽宁省沈阳市 110013
ORCID number: $[AuthorORCIDs]
电话: 024-83956416
收稿日期: 2002-11-06
修回日期: 2002-11-10
接受日期: 2002-11-18
在线出版日期: 2003-10-15
目的
探讨幽门螺杆菌(Helicobacter pylori, Hp)对克拉霉素耐药的分子基础.
方法
采用E-test方法对35例Hp 的临床分离株进行克拉霉素的MIC (minimal inhibitory concentration)检测, 大于或等于8 mg/L为耐药株. 按酚-氯仿方法提取Hp的DNA, PCR方法扩增23S rRNA基因中2 047-2 347之间的片段, 对PCR产物进行序列分析, 观察耐药株的基因突变情况.
结果
与敏感菌(No33)序列比较, No13存在1个突变位点, 即2 289位点T变成了C (T2289C), No17存在2个突变位点, 即G2224A、T2289C, No22存在3个突变位点, 即G2224A、C2245T及T2289C. 三株耐药Hp菌株的MIC值分别是: No13为8.0 mg/L, No17为64 mg/L, No22为大于256mg/L. 随着耐药性的提高(表现在MIC值的升高), 高耐药性菌株的突变位点多于低耐药性菌株的突变位点.
结论
与耐药有关的3个突变位点, G2224A、C2245T及T2289C, 国内外未见报道, 反映了Hp耐药的地区差异.
关键词: N/A
引文著录: 郝庆, 李岩, 高红, 张显忠. 幽门螺杆菌对克拉霉素耐药的分子基础. 世界华人消化杂志 2003; 11(10): 1485-1487
Molecular mechanism of the resistance of Helicobacter pylori to clarithromycin
Qing Hao, Yan Li, Hong Gao, Xian-Zhong Zhang
Qing Hao, Yan Li, Department of Gastroenterology of the 2nd Affiliated Hospital, China Medical University, Shenyang 110004, Liaoning Province, China
Hong Gao, Key Laboratory for Congenital Malformation of the Ministry of Health, China Medical University, Shenyang 110004, Liaoning Province, China
Xian-Zhong Zhang, Department of Gastroenterology, the Red Cross Hospital of Shenyang, Shenyang 110013, Liaoning Province, China
Corresponding author: Dr. Qing Hao, Gastroenterology Department of the 2nd Affiliated Hospital of China Medical University, 36 Sanhao Jie, Heping District, Shenyang 110004, Liaoning Province, China. haoqing007@sohu.com
Received: November 6, 2002
Revised: November 10, 2002
Accepted: November 18, 2002
Published online: October 15, 2003
AIM
To investigate the resistance mechanism of Hp to clarithromycin.
METHODS
With E-test method, we examined the minimal inhibitory concentration (MIC) to clarithromycin of 35 Hp clinical isolates. Resistance strains were defined when MIC≥8 mg/L. Extract the DNA from the bacteria with the phenol-chloroform extraction method. Then amplify the fragments from 2 047 to 2 347 of 23 S rRNA gene. Gene sequence of the PCR products was analyzed to observe the mutation in the resistant Hp strains.
RESULTS
Compared with susceptible strains, No13 strain contained one point mutation (T2289C), No17 had two point mutations (G2224A, T2289C) and No22 strain had 3 point mutations (G2224A, C2245T, T2289C).The MICs of the 3 resistant Hp isolates were as follows: No13 of 8.0 mg/L, No17 of 64 mg/L, No22 of >256 mg/L. With increase of the resistance of Hp strains, the number of point mutations increased.
CONCLUSION
The point-mutations at 23 S rRNA gene responsible for Hp resistance to clarithromycin have not been reported in literature either at home or abroad, demonstrating that different mechanism of Hp resistance to clarithromycin exists in different regions.
Key Words: N/A
0 引言
幽门螺杆菌(Helicobacter pylori, Hp)是许多消化系疾病包括胃癌的主要致病因子[1-10], 抗Hp的治疗也成为消化性溃疡治疗学方面的一个重要突破. 由于Hp主要定植在胃黏液层下胃小凹表面, 根除治疗相对困难, 克拉霉素被认为是杀Hp效果最好的抗生素[11]. Hp耐药是治疗失败的主要原因[12-14], 国外报道克拉霉素耐药是由于Hp的23S rRNA基因中2143, 2144位点上A到G的突变引起[15-18], 而国内关于该方面的报道极少[19,20]. 我们在前述实验基础上[21], 利用E-test方法筛选出克拉霉素耐药Hp菌株, 探讨了其耐药的分子基础如下.
1 材料和方法
1.1 材料
Hp菌株来源: 利用E-test方法对35例Hp的临床分离株进行克拉霉素的MIC (minimal inhibitory concentration)值测定, 大于或等于8 mg/L为耐药株, 共3株, No13 (MIC为8 mg/L)、No17 (MIC为64 mg/L)及No22(MIC为大于或等于256 mg/L), 1例敏感株, No33(MIC为0.125 mg/L); 引物(23S rRNA基因2 047-2 347之间, 由上海生工生物工程技术服务有限公司); dNTP, 100 bp DNA Ladder Marker (宝生物工程大连有限公司); PCR扩增仪(biometra, germany); 测序仪器为ABI PRISM 377-96; 测序试剂为BigDye terminator v2.0
1.2 方法
按酚-氯仿方法提取Hp DNA. PCR扩增上游引物: 5'-CTGCATGAATGGCGTAACGAG-3'(2 047-2 067); 下游引物: 5'-GAGCGACCGCCCCAGTCAAAC-3'(2 347-2 327); PCR循环体系共20 μL , 其中包括: dd H2O 13.3 μL; 10xPCR buffer 2.5 μL; dNTPs (2.5 mmol/L) 2.0 μL; Taq 酶(5 KU/L) 0.2 μL; 引物(1: 5x)1.5 μL; DNA sample 0.5 μL; 循环条件: 94.0 °C 4 min, 94.0 °C 40 s, 61.5 °C 1 min, 72.0 °C 1 mins, 72.0 °C 7 min, 共32个循环; 聚丙烯酰胺凝胶电泳, 观察PCR产物纯度; 观察扩增产物电泳图, 确定反应体系中PCR产物单一而含量高时, 按上述条件扩增50 μL PCR产物, 由上海生工生物技术有限服务公司, 进行PCR产物序列测定.
2 结果
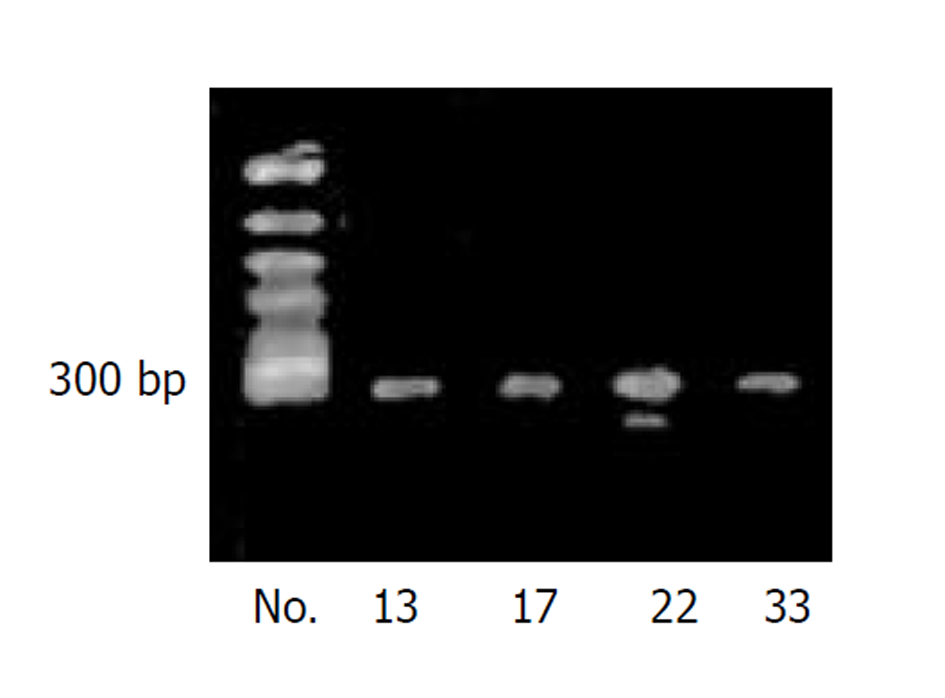
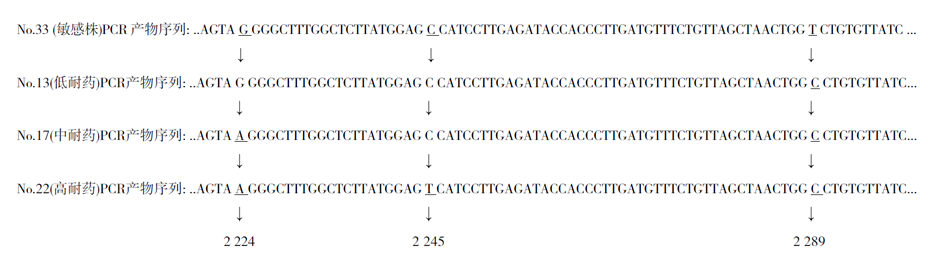
PCR产物为301 bp的DNA片断, 反应体系中只含有单一的目的片断, 无污染, 无杂带(图1). No33为克拉霉素敏感Hp菌株, No.13, 17, 22均为克拉霉素耐药Hp菌株. 从测序图谱中可以发现: 与敏感菌(No.33)序列比较, No.13共测出279个碱基, 其中存在1个突变位点, 即2 289位点T变成了C(T2289C), No.17共测出278个碱基, 其中存在2个突变位点, 即G2224A, T2289C, No.22共测出278个碱基, 其中存在3个突变位点, 即G2224A, C2245T及T2289C. 三株耐药Hp菌株的MIC值分别是: No.13为8.0 mg/L, No.17为64 mg/L, No.22为大于256 mg/L. 随着耐药性的提高(表现在MIC值的升高), 我们发现高耐药性菌株的突变位点多于低耐药性菌株的突变位点(图2).
图2 克拉霉素耐药Hp菌株23S rRNA基因突变情况.
3 讨论
Hp对克拉霉素耐药的现象不断出现, 从而导致了三联根治方案的失败. 根据大肠杆菌对克拉霉素的耐药机制, Stone et al [15]首先发现并报告了Hp对克拉霉素耐药的分子基础是23S rRNA基因中2 143, 2 144位点上A到G的突变, 在随后的研究[22-25]中也发现了其他位点上的一些突变导致耐药, 比如: A2142C, A2143C, A2143T, A2115G, G2141A. Hp的遗传学特征存在明显的地域差别[26,27], Hp耐药株的遗传学特征也存在着明显的地域差别[28]. 关于中国人感染的克拉霉素耐药Hp菌株的分子基础, 研究报道的极少, 史彤et al [19]曾利用PCR-RFLP方法分析了上海地区克拉霉素耐药Hp菌株的遗传特征, 该研究只是根据23S rRNA基因中2 143, 2 144位点上A到G突变后, 可以产生新的酶切位点, 而推断耐药株可能存在该位点的突变, 而未进行直接的目的基因的序列分析, 故也不能发现除上述2个位点之外的突变, 因而该研究具有一定的局限性. 我们通过E-test方法筛选出3株不同程度的Hp耐药株, 其MIC值分别为: No.13 8 mg/L, No.17 64 mg/L, No.22>256 mg/L, 和1例敏感株, No.33, 其MIC值为0.125 mg/L. 我们发现, 与敏感株相比, 3株耐药株均存在点突变, 且不同耐药程度的Hp菌株, 突变位点的数目也不相同, 低度耐药的13号Hp菌株只存在T2289C的突变, 中度耐药的17号Hp菌株存在2处突变, 即G2224A 和T2289C, 而高度耐药的22号Hp菌株发生了3处突变: 即G2224A, C2245T和T2289C, 随耐药性的增加, 突变的位点数目也增加. 由上述结果还可以看出, 耐药突变局限于2 219-2 289之间, 共70个碱基对之中, 其中T2289C的突变存在于3例Hp耐药株中, 而C2245T只存在于高耐药的No.22号Hp菌株中, G2224A存在于中、高度耐药株中. 这个现象在国内外的研究中均未见报道, 而国外常报道的A2143G和A2144G的突变也未能在本研究中出现, 这一点也证实了Hp耐药机制的地域差异. 国内关于这方面的研究还需进一步深入进行, 以期建立中国人感染的克拉霉素耐药Hp菌株的遗传学资料.
克拉霉素杀菌机制[29]在于, 他可以与23S rRNA肽链转移酶结合, 从而抑制菌体蛋白质的合成, 起到杀菌作用, 当该基因发生突变时, 其编码的氨基酸发生改变, 肽链转移酶环状结构的局部发生破坏, 克拉霉素与核糖体的结合即减弱, 失去了作用位点, 不能发挥抗菌作用, 临床上即出现了克拉霉素耐药现象. 自然界中, 生物的遗传物质存在着自然突变率, 但是非常低, 大约在10-6-10-8, Hp耐药突变的产生目前倾向于认为是抗生素选择性压力的结果[30], 即由于克拉霉素的大量广泛应用, 杀死了敏感菌, 而留下了自然突变产生的耐药株进一步繁殖, 形成主要致病菌, 但大环内酯类药物能否诱发这种耐药突变, 目前还未见有关报道.