Published online Nov 21, 2020. doi: 10.3748/wjg.v26.i43.6880
Peer-review started: October 14, 2020
First decision: November 3, 2020
Revised: November 3, 2020
Accepted: November 9, 2020
Article in press: November 9, 2020
Published online: November 21, 2020
Processing time: 36 Days and 11.1 Hours
The current coronavirus disease 2019 (COVID-19) pandemic has affected routine endoscopy service across the gastroenterology community. This led to the suspension of service provision for elective cases.
To assess the potential barriers for resuming the endoscopy service in Egypt.
A national online survey, four domains, was disseminated over a period of 4 wk in August 2020. The primary outcome of the survey was to determine the impact of the COVID-19 pandemic on the endoscopy service and barriers to the full resumption of a disabled center(s).
A hundred and thirteen Egyptian endoscopy centers participated in the survey. The waiting list was increased by ≥ 50% in 44.9% of areas with clusters of COVID-19 cases (n = 49) and in 35.5% of areas with sporadic cases (n = 62). Thirty nine (34.8%) centers suffered from staff shortage, which was considered a barrier against service resumption by 86.4% of centers in per-protocol analysis. In multivariate analysis, the burden of cases in the unit locality, staff shortage/recovery and the availability of separate designated rooms for COVID-19 cases could markedly affect the resumption of endoscopy practice (P = 0.029, < 0.001 and 0.02, respectively) and Odd’s ratio (0.15, 1.8 and 0.16, respectively).
The COVID-19 pandemic has led to restrictions in endoscopic volumes. The staff shortage/recovery and the availability of COVID-19 designed rooms are the most important barriers against recovery. Increasing working hours and dividing endoscopy staff into teams may help to overcome the current situation.
Core Tip: This survey study included 113 endoscopy centers from all over Egypt. Our findings highlighted the barriers for resuming endoscopy in different types of health care facilities in Egypt as well as reporting the current practice in Egyptian endoscopy units during the pandemic. Our study offers real life based snapshot of the current practice and recommendations for routine endoscopic practice during the second wave.
- Citation: Elshaarawy O, Lashen SA, Makhlouf NA, Abdeltawab D, Zaghloul MS, Ahmed RM, Fathy H, Afifi S, Abdel-Gawad M, Abdelsameea E, Abd-Elsalam S, Mohamed SY, Tag-Adeen M, Tharwat M, Alzamzamy A, Bekhit AN, Eid AM, Awad A, Aamr M, Abd El Dayem WA, Wifi MN, Alboraie M. Barriers for resuming endoscopy service in the context of COVID-19 pandemic: A multicenter survey from Egypt. World J Gastroenterol 2020; 26(43): 6880-6890
- URL: https://www.wjgnet.com/1007-9327/full/v26/i43/6880.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i43.6880
In December 2019, a novel an enveloped Ribonucleic acid (RNA) beta coronavirus caused an outbreak called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) - resulted in coronavirus disease 2019 (COVID-19) began in Wuhan[1,2]. The virus rapidly spread throughout the country, then throughout the whole world, and was declared a global pandemic by the World Health Organization in March 2020[3]. As of September 23, 2020, it has infected over 31 million people worldwide and caused more than 965000 deaths[3,4].
The clinical gastrointestinal manifestations are present and less severe when compared with SARS[1,5,6]. Early reports from Wuhan stated that around 10% of COVID-19 cases had diarrhea and nausea, 1 to 2 d before the beginning of respiratory symptoms[6], and some cases may be missed if screening was applied only to those with respiratory symptoms. It is widely believed that SARS-CoV-2 spreads via droplets and contact (especially if within one meter of distance), but there is evidence that airborne spread is also possible during aerosol-generating procedures (AGPs)[2].
In addition, new emerging evidence that SARS-CoV-2 can be found in the feces of patients, giving the possibility of fecal–oral route transmission[7,8]. This can be explained by the excessive expression of angiotensin-converting enzyme 2 protein, a receptor for SARS-CoV-2 required for cell entry in the epithelial layer of the gastrointestinal tract[9].
Being highly infective, SARS-CoV-2 put the healthcare workers (HCWs) in clinical departments performing endoscopy in great challenges during this pandemic as being highly susceptible to getting the infection[10]. Endoscopy could be considered a high-risk procedure as pulmonary and gastric secretions, as well as fecal material, may contain high viral loads. So, infection to HCWs occurs either due to direct contact with the infected patients or to the lack or improper use of the personal protective equipment (PPE)[11]. In fact, several studies have discussed infection prevention and control measures that must be implemented to increase patient safety, prevent nosocomial outbreaks, protect HCWs, and ensure the rational use of limited PPE[11,12].
Several endoscopy societies and expert groups have offered recommendations and position statements for endoscopy during the COVID-19 pandemic[11,13-16]. Several GI society guidelines recommended ceasing elective procedures during the pandemic to decrease the risk of infection[17-19]. Different recommendations/guidelines have been recently released to ensure the smooth reopening of endoscopy units and resuming elective procedures[17]. Whether or not endoscopy units in different parts of the world are ready to resume service based on these recommendations is not fully known.
This study is a multicenter study to discuss the barriers of resuming endoscopic maneuvers in different centers and governorates in Egypt as the coronavirus infection rate has remarkably decreased and there are international calls for resuming all the activities with caution and different precautions, and to assess whether the endoscopic service has returned to its near normal standard level.
We designed an online survey that was based on four domains (Supplementary Figure 1). The first domain included the demographic data as regards the governorate, the type of health care facility, and the type(s) of endoscopy service(s) provided. The second domain was for the status of the COVID-19 pandemic and its impact on the endoscopy service(s). The third domain was directed to the readiness of the health care facility for dealing with COVID-19 cases (infrastructure, working staff, PPEs, case stratification, etc.), and the fourth domain was about the ability of the facility to resume the endoscopy service(s) and the different barriers which preclude service resumption. The whole survey included 20 main questions. All the questions were closed-ended questions that could be answered by selecting the appropriate answer(s).
The questionnaire was set-up by a nationally representative group of endoscopy physicians covering different Egyptian governorates. The survey was designed using the RedCap platform (v9.1.0., United States). The study was approved by the Institutional Review Board of the National Liver Institute, Menoufia University, Egypt (NLI IRB 00003413) in June 2020, protocol number 00203/2020. The questionnaire was distributed online for 4 wk (starting from July 30, 2020 till August 28, 2020). The primary outcome of the survey was to identify the current impact of the COVID-19 pandemic on the endoscopy service and the barriers against the full resumption of the participating centers.
Data were collected and entered into personal computers and analyzed using Statistical Package for Social Sciences (SPSS version 26.0) software (IBM SPSS Inc. Chicago, United States). The incomplete responses were excluded from the analysis. For simplification, we divided the responding governorates according to the administrative division of the governorates of Egypt (see below in discussion). The data were expressed as numbers (proportions). Comparisons between groups were made by the χ2 or Fisher’s test (FET) for the qualitative variables. A uni- and multivariate regression analysis was done to identify the parameters which determine the decision making as regards the resumption of endoscopy service if not working. Correlation analysis also was done to explore the correlation between the current status of endoscopy service and the different domains.
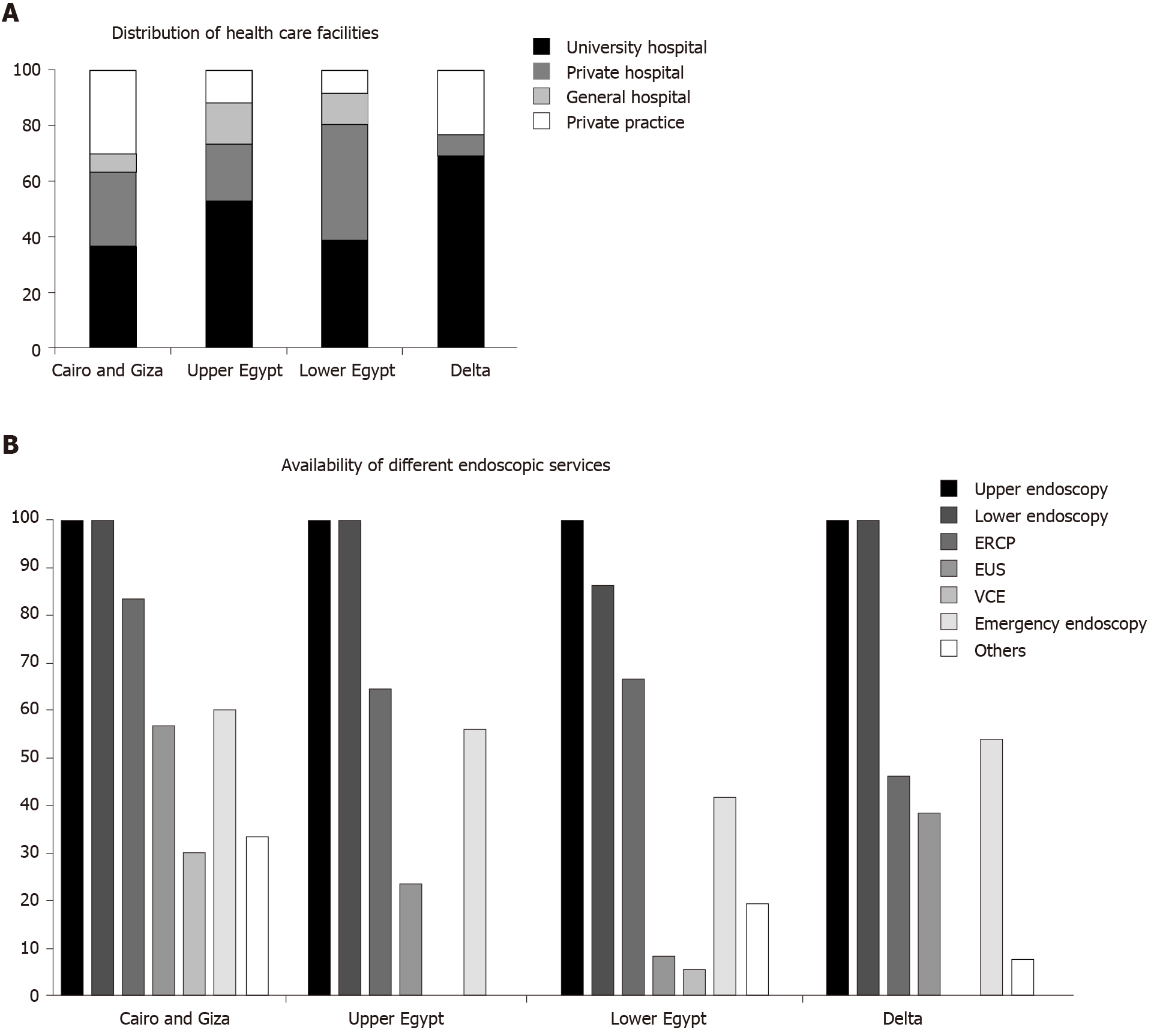
The survey was sent to 115 endoscopy centers all over Egypt, of which 113 (98.3%) responded to the survey in complete response and two centers didn’t give a full response, so they were excluded from the analysis. Most respondents (n = 67, 59.3%) were from high-volume endoscopy units either University or teaching facility general hospitals providing emergency endoscopy. Cairo and Giza regions have participated with 30 (26.5%) centers, Lower Egypt (Alexandria, Beheira, Sharqia, Qalyubia, Damietta, and Ismailia) and Upper Egypt (Assiut, Fayoum, Sohag, Qena, Aswan and Luxor) have participated through 34 (30.1%) centers, and the Delta region (Menoufia, Kafr El-sheik , Gharbia, and Dakahlia) have participated through 13 (11.5%) centers. COVID-19 designated facilities were present among 48 (42.5%) centers (Figure 1).
On the day of the planned endoscopic procedures patients were checked for being suspected cases of COVID-19 in 95 (84.1%) of centers. The process of selection and screening was based on symptoms among 90 centers (79.6%), temperature check among 82 centers (72.6%), non-contrast multi spiral computed tomography (MSCT) chest among 50 centers (44.2%), polymerase chain reaction (PCR) testing among 11 centers (9.7%), and antibody testing among 3 centers (2.7%).
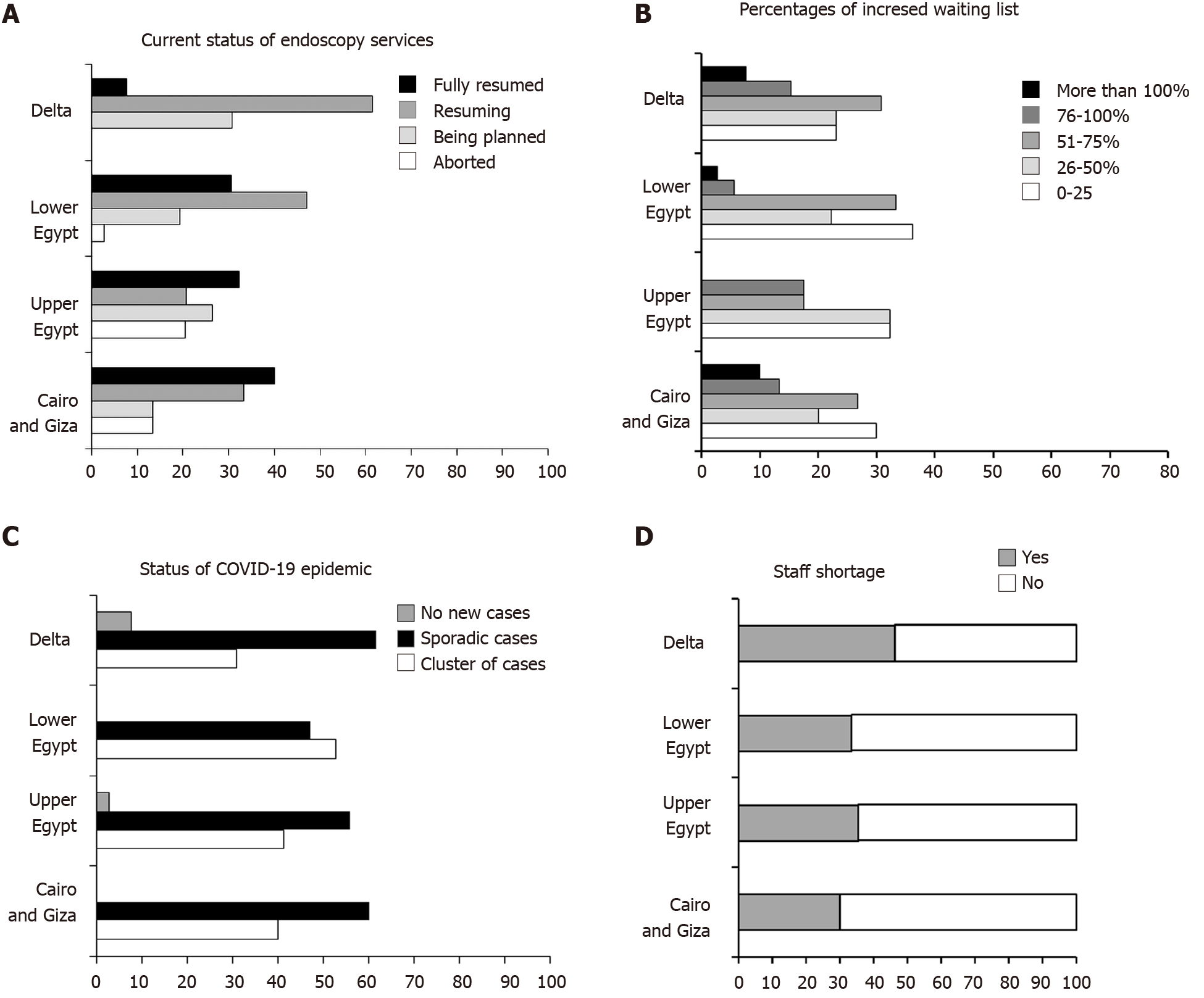
Endoscopy practice was almost resuming or resumed in about 70% of the centers Figure 2A. In general, there was an expansion of the waiting lists all over the country. The Quantification of the expansion is shown in Figure 2B. We found significant variation in the waiting lists according to the distribution of COVID-19 pandemic status among different centers (Figure 2B and C). In areas with clusters of cases (n = 49), the waiting lists increased by 0%-25% in 14.29%, 26%-50% in 32.65%, 51%-75% in 34.69%, 76%-100% in 10.2%, and by more than 100% in 8.17% of these centers. While in areas with sporadic cases (n = 62), 45.16% of the centers had their waiting list increased by 0%-25%, however, in 19.35% and 20.9% of the centers the list increased by 26%-50%, and 51%-75%, respectively. In about 14.59% of the centers, the waiting list increased by more than 75%, meanwhile, areas with no new cases (n = 2), 50% of centers had their list increased by only 0%-25% (FET = 19.1, P = 0.005).
During the COVID-19 outbreak, endoscopy staff has been deployed to COVID-19 designated wards and hospitals. In addition, a significant number of healthcare providers were infected. The shortage of endoscopy staff was present among 39 (34.8%) of centers (Figure 2D). Specialists shortage was present in 88 (77.9%) of centers, nursing staff shortage in 90 (79.6%) of centers, and trainees shortage in 110 (97.3%) of centers. This shortage was considered as a barrier against resuming endoscopy service among 38 (33.6% in intention to treat analysis, 86.4% in per-protocol analysis; 69 centers didn’t answer). The shortage in specialists was more pronounced in Delta and lower Egypt than upper Egypt and Cairo and Giza (61.5% and 91.3% vs. 64.7% and 83.3% respectively, P = 0.019). However, the shortage of nursing staff and trainees were not significantly different among different centers, P = 0.93 and P = 0.24, respectively).
Only 41 units (35%) had to increase the working hours to compensate for this shortage. Seventy-six units (67.3%) recovered their staff either from sick leave or COVID-19 wards.
During the current COVID-19 epidemic in Egypt, 72 (63.7%) of endoscopy centers have provided suitable waiting areas for appropriate social distancing precautions, 65 (57.5%) of centers could provide an adequate number of recovery rooms to keep the social distancing strategy to the optimum, and 40 (35.4%) of centers have increased their working hours to accommodate the extra-burden of increased cases volume; at the same time, 77 (68.1%) of centers have adopted selection strategy to select the endoscopist and the assisting team based on the presence of a suspected/confirmed COVID-19 cases. Sixty-three (55.7%) units were planning to resume the pre-pandemic capacity with a designated track for confirmed COVID-19 cases. However, only 24 (21.2%) of centers could provide special endoscopy rooms for confirmed or suspected COVID-19 cases. Of note, training was already resumed in 16 units (14.2%).
The Intra-procedural precautions applied during the COVID-19 pandemic in Egypt varied according to the availability of PPE in each facility locality as shown in Table 1 (more details in Supplementary Table 1).
| Governorates | Usage of PPE | Action taken by centers | ||||
| For all cases | For suspected cases | For confirmed cases only | Vary accordingly | Delay of turnover for cleaning | Increased time/case | |
| Cairo and Giza | 5 (16.7) | 13 (43.3) | 12 (40) | 8 (26.7) | 27 (90) | 21 (70) |
| Upper Egypt | 10 (29.4) | 7 (20.6) | 13 (38.2) | 7 (20.6) | 32 (94.1) | 27 (79.4) |
| Lower Egypt | 13 (36.1) | 10 (27.8) | 10 (27.8) | 8 (22.2) | 32 (88.9) | 29 (80.6) |
| Delta | 7 (53.8) | 4 (30.8) | 3 (23.1) | 3 (23.1) | 13 (100) | 13 (100) |
Post-procedural patient follow-up for the development of fever or suspected COVID-19 symptoms for 14 d after discharge was a strategy adopted by 18 (15.9%) of centers only. The follow up was performed by either a resident doctors (8%), endoscopy nurses (5.3%), administrative staff (6.2%), and/or specialist physicians (1.8%).
Multivariate regression analysis showed that burden of cases in the unit locality, staff shortage and their recovery and the availability of separate designated rooms for COVID-19 cases could markedly affect the resumption of endoscopy practice (P = 0.029, < 0.001 and 0.02, respectively) and Odd’s ratio (0.15, 1.8 and 0.16, respectively) (Table 2).
| Factor | Univariate | Multivariate | |||
| P value | OR | P value | OR | 95%CI | |
| Status of pandemic | 0.03 | 1.5 | 0.029 | 0.15 | 0.20-0.9 |
| Shortage of PPE | 0.04 | 4.2 | 0.42 | 2.24 | 0.31-16.1 |
| Staff recovery | 0.05 | 1.4 | < 0.001 | 1.8 | 5.1-6.7 |
| Having a COVID designed unit | 0.04 | 4.2 | 0.01 | 0.5 | 0.11-0.82 |
| Having separate endoscopy room | 0.04 | 1.01 | 0.02 | 0.16 | 0.03-0.7 |
| Patient classified before procedure | 0.03 | 1.7 | 0.007 | 0.7 | 1.1-1.18 |
The prolonged suspension of routine endoscopic services during the SARS-CoV-2 pandemic has significant implications on diagnostic endoscopic services such as delay in diagnosis and management of cancer patients as well as the expansion of waiting lists worldwide. Therefore, this encouraged the international gastrointestinal endoscopic societies to release position statements, recommendations, and guidance for the rapid and safe resumption of endoscopic services commensurate with facilities and pandemic situations of each country[14,17-19]. To our knowledge, whether or not endoscopy centers in Egypt are ready to resume elective services has not been studied. Accordingly, the results of the current survey represent the current status of resuming routine endoscopic services in Egypt and determine the barriers of resuming such services.
Our results showed that 70% of different centers all over Egypt have resumed routine endoscopic services as is illustrated in Figure 2A. This is in parallel to the current situation of early recovery phases of the pandemic and the decline in the number of new COVID-19 cases in Egypt and other countries worldwide[3]. Expansion of elective endoscopy waiting lists is one of the challenges to resume the full capacity of endoscopic services. According to the British Society of Gastroenterology guidance in the early recovery stages, triage mechanisms are needed to prioritize patients scheduling according to the indications[20].
The highest percentages of waiting lists expansion are observed in areas with clusters of COVID-19 cases which indicate the awareness of senior decision-makers of endoscopy centers in Egypt with the importance of triaging and prioritization of patients scheduling in the light of clinical need with the available capacity. Also, this reflects their compliance with GI endoscopy societies' guidance. In addition, this observation complies with the current SARS-CoV-2 pandemic situation in Egypt, as there is a decrease in the number of areas with new cases allowing endoscopy centers to restore their full capacity as soon as possible.
Regarding the shortage in endoscopy staff, 34.5% of the centers reported a significant shortage of staff during the SARS-CoV-2 pandemic in nursing staff (79.6%) and specialists (77.9%). This is related to two factors; one was the reallocation of staff and medical equipment to the surge in demand to manage suspected and confirmed COVID-19 cases and the other was some of them get infected caused by frequent exposure to infected patients. The shortage in specialists was more pronounced in Delta and Lower Egypt geographically which may be related to the geographic distribution of a large number of confirmed COVID-19 cases and isolation hospitals that need more medical staff.
This shortage in endoscopy staff is considered as a barrier against resuming endoscopy service among 38 centers in the current study (33.6% in intention to treat analysis where n = 113, 86.4% in the per-protocol analysis where n = 44). Regarding patient selection before endoscopy, a large number of participating centers (84.1%) screened their patients. The most common method used was symptoms-based screening for COVID-19 risk stratification (79.6%) of the centers and fewer centers used PCR testing (9.7%).
Similarly, Alboraie et al[21] reported that most worldwide centers (93.9%) screened patients for possible COVID-19 disease prior to the procedure and 54 centers (33.13%) used PCR testing. However, asymptomatic infected patients are a known source for transmission[2,22], accordingly, this type of screening is not sufficient to guide for COVID-19 risk stratification. A recent study from China, employed both symptoms-based screening and PCR in patient’s screening, reported no cases of endoscopy-related nosocomial COVID-19 disease transmission in 1361 cases[23].
Regarding pre-procedural precautions and endoscopy centers designation, our results show that most participating centers so far follow the different international GI endoscopy societies guidelines[14,17-19] including appropriate social distancing precautions or increase working hours to accommodate the extra-burden of increased cases volume. More than two-thirds of our centers have adopted a selection strategy to select the endoscopist and the assisting team based on the presence of a suspected/confirmed COVID-19 case. Also, Alboraie et al[21] stated that the majority (78.5%) of the centers considered dedicated teams for the delivery of endoscopic services after the onset of the pandemic.
To reduce the risk of infection spread most of the international society's recommendations are in agreement with the existence of a restricted protocol for infection control and the awareness of medical staff for the donning and doffing of PPE. According to the results of our study, there is wide variability between different centers regarding intra-procedural precautions depending upon the availability of PPE and type of procedures. We can overcome those types of barriers by reuse some of PPE components such as respirator masks in case of shortage as it was reported by many studies as the methods of decontamination were explained[23-25].
Most of the international recommendations on endoscopy encourage follow-up of patients after endoscopic procedures[11]. Unfortunately, in our study few participating centers (15.9%) are practicing the strategy of following their patients for the development of any suspected symptoms post-procedure. A similar study showed that 18.4% of centers only called patients back two weeks after procedures[21]. According to multivariate regression analysis that was done in our study, we found that endoscopy staff shortage, availability of separate designated rooms for COVID-19 cases, and the burden of cases in each locality are the most obvious barriers for the resumption of routine endoscopy practice in Egypt.
Although there are many barriers that may interfere with the complete restoration of endoscopy services in Egypt, according to the results of our study, most participating centers are preparing their facilities for the resumption of full endoscopy services.
We recommend increasing working hours and dividing endoscopy staff into teams to overcome the shortage of endoscopy staff. Also, follow up of patients for two weeks after endoscopic procedures to detect any possible transmission of SARS-CoV-2 infection in endoscopy centers as this strategy may help in tracing the source of nosocomial transmission.
In conclusion, the current study represents an important national multicenter survey addressing crucial information about resuming regular gastrointestinal endoscopy services and its barriers in Egypt.
An outbreak of coronavirus disease 2019 (COVID-19) has hit the world and disturbed the whole healthcare system, including endoscopic practices which are a very risky procedures in terms of exposure to infection.
Smooth resumption of routine endoscopic service has to be guaranteed as well as decreasing the burden of exposing patients and endoscopy staff to infection during endoscopic procedures. Many strategies have to be implemented in endoscopy units, however, these strategies face many barriers as shortage of personal protective equipment, working staff and post procedure tracing of infection and follow-up of patients.
This survey study was designed to evaluate the feasibility and the difficulty of resumption of routine endoscopic service in the context of COVID-19 pandemic.
We conducted a survey study that included 20 questions to be answered by the head of endoscopy units in 113 units from all over Egypt.
One hundred and thirteen centers participated in the study from all over Egypt. Due to halting the routine endoscopic services during the pandemic, the waiting lists were doubled in most of the centers. Third of the centers experienced significant shortage of endoscopy staff. The lack of dedicated endoscopy rooms for infected patients and the staff shortage were the main barriers to resume routine services smoothly.
We recommend increasing working hours and dividing endoscopy staff into teams to overcome the shortage of endoscopy staff. Also, follow up of patients for two weeks after endoscopic procedures to detect any possible transmission of infection in endoscopy centers as this strategy may help in tracing the source of nosocomial transmission.
For smooth resumption of endoscopic service between two waves of the current pandemic, several strategies have to be applied in a uniform manner in all endoscopy units. Our study showed how different centers acted differently during this pandemic in terms of their plan to safely getting routine endoscopy service on track. Future studies should propose modalities to guarantee uniform application of determined strategies that overcome the current barriers.
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: United European Gastroenterology; Egyptian Association for Research and Training in Hepatogastroenterology.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Galloro G, Liu YC S-Editor: Gao CC L-Editor: A P-Editor: Ma YJ
| 1. | Xie J, Tong Z, Guan X, Du B, Qiu H. Clinical Characteristics of Patients Who Died of Coronavirus Disease 2019 in China. JAMA Netw Open. 2020;3:e205619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 228] [Article Influence: 45.6] [Reference Citation Analysis (0)] |
| 2. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35178] [Cited by in RCA: 30014] [Article Influence: 6002.8] [Reference Citation Analysis (3)] |
| 3. | World Health Organization. Coronavirus Disease (COVID-19) Situation Reports. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. |
| 4. | Joao BN. Geographic Information Systems and COVID-19: The Johns Hopkins University Dashboard. 2020 Preprint. Available from: ResearchSquare: rs-15447. [DOI] [Full Text] |
| 5. | Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14869] [Cited by in RCA: 12940] [Article Influence: 2588.0] [Reference Citation Analysis (1)] |
| 6. | Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14113] [Cited by in RCA: 14738] [Article Influence: 2947.6] [Reference Citation Analysis (0)] |
| 7. | Gu J, Han B, Wang J. COVID-19: Gastrointestinal Manifestations and Potential Fecal-Oral Transmission. Gastroenterology. 2020;158:1518-1519. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 954] [Cited by in RCA: 949] [Article Influence: 189.8] [Reference Citation Analysis (1)] |
| 8. | Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for Gastrointestinal Infection of SARS-CoV-2. Gastroenterology 2020; 158: 1831-1833. e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1985] [Cited by in RCA: 1991] [Article Influence: 398.2] [Reference Citation Analysis (1)] |
| 9. | Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, Tan W. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA. 2020;323:1843-1844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1894] [Cited by in RCA: 2656] [Article Influence: 531.2] [Reference Citation Analysis (0)] |
| 10. | Ni W, Yang X, Yang D, Bao J, Li R, Xiao Y, Hou C, Wang H, Liu J, Yang D, Xu Y, Cao Z, Gao Z. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit Care. 2020;24:422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 843] [Cited by in RCA: 695] [Article Influence: 139.0] [Reference Citation Analysis (1)] |
| 11. | Soetikno R, Teoh AYB, Kaltenbach T, Lau JYW, Asokkumar R, Cabral-Prodigalidad P, Shergill A. Considerations in performing endoscopy during the COVID-19 pandemic. Gastrointest Endosc. 2020;92:176-183. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 154] [Cited by in RCA: 158] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 12. | Mayol J, Fernández Pérez C. Elective surgery after the pandemic: waves beyond the horizon. Br J Surg. 2020;107:1091-1093. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 61] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 13. | Zhang Y, Zhang X, Liu L, Wang H, Zhao Q. Suggestions for infection prevention and control in digestive endoscopy during current 2019-nCoV pneumonia outbreak in Wuhan, Hubei province, China. Endoscopy. 2020;52:312-314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 14. | Catlow J, Beaton D, Beintaris I, Shaw T, Broughton R, Healey C, Penman I, Coleman M, Rutter M. JAG/BSG national survey of UK endoscopy services: impact of the COVID-19 pandemic and early restoration of endoscopy services. Frontline Gastroenterol. 2020;0:1-7. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Repici A, Maselli R, Colombo M, Gabbiadini R, Spadaccini M, Anderloni A, Carrara S, Fugazza A, Di Leo M, Galtieri PA, Pellegatta G, Ferrara EC, Azzolini E, Lagioia M. Coronavirus (COVID-19) outbreak: what the department of endoscopy should know. Gastrointest Endosc. 2020;92:192-197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 373] [Cited by in RCA: 379] [Article Influence: 75.8] [Reference Citation Analysis (0)] |
| 16. | Francis N, Dort J, Cho E, Feldman L, Keller D, Lim R, Mikami D, Phillips E, Spaniolas K, Tsuda S, Wasco K, Arulampalam T, Sheraz M, Morales S, Pietrabissa A, Asbun H, Pryor A. SAGES and EAES recommendations for minimally invasive surgery during COVID-19 pandemic. Surg Endosc. 2020;34:2327-2331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 125] [Cited by in RCA: 163] [Article Influence: 32.6] [Reference Citation Analysis (0)] |
| 17. | . American Society for Gastrointestinal Endoscopy: guidance for trainees during the COVID-19 pandemic. Gastrointest Endosc. 2020;92:748-753. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Chiu PWY, Ng SC, Inoue H, Reddy DN, Ling Hu E, Cho JY, Ho LK, Hewett DG, Chiu HM, Rerknimitr R, Wang HP, Ho SH, Seo DW, Goh KL, Tajiri H, Kitano S, Chan FKL. Practice of endoscopy during COVID-19 pandemic: position statements of the Asian Pacific Society for Digestive Endoscopy (APSDE-COVID statements). Gut. 2020;69:991-996. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 256] [Cited by in RCA: 249] [Article Influence: 49.8] [Reference Citation Analysis (0)] |
| 19. | Gralnek IM, Hassan C, Beilenhoff U, Antonelli G, Ebigbo A, Pellisè M, Arvanitakis M, Bhandari P, Bisschops R, Van Hooft JE, Kaminski MF, Triantafyllou K, Webster G, Pohl H, Dunkley I, Fehrke B, Gazic M, Gjergek T, Maasen S, Waagenes W, de Pater M, Ponchon T, Siersema PD, Messmann H, Dinis-Ribeiro M. ESGE and ESGENA Position Statement on gastrointestinal endoscopy and the COVID-19 pandemic. Endoscopy. 2020;52:483-490. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 259] [Cited by in RCA: 295] [Article Influence: 59.0] [Reference Citation Analysis (0)] |
| 20. | The British Society of Gastroenterology. BSG Guidance on recommencing GI Endoscopy in the deceleration & early recovery phases of the COVID-19 pandemic. Available from: https://www.bsg.org.uk/covid-19-advice/bsg-guidance-on-recommencing-gi-endoscopy-in-the-deceleration-early-recovery-phases-of-the-covid-19-pandemic/. |
| 21. | Alboraie M, Piscoya A, Tran QT, Mendelsohn RB, Butt AS, Lenz L, Alavinejad P, Emara MH, Samlani Z, Altonbary A, Monged A, Lemmers A, Sudovykh I, Ho DQD, Ghazanfar S, Kamau E, Iqbal S, Tan DMY, Liao WC, Vignesh S; “The Global Endo-COVID working group”. The global impact of COVID-19 on gastrointestinal endoscopy units: An international survey of endoscopists. Arab J Gastroenterol. 2020;21:156-161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (1)] |
| 22. | Hoehl S, Rabenau H, Berger A, Kortenbusch M, Cinatl J, Bojkova D, Behrens P, Böddinghaus B, Götsch U, Naujoks F, Neumann P, Schork J, Tiarks-Jungk P, Walczok A, Eickmann M, Vehreschild MJGT, Kann G, Wolf T, Gottschalk R, Ciesek S. Evidence of SARS-CoV-2 Infection in Returning Travelers from Wuhan, China. N Engl J Med. 2020;382:1278-1280. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 433] [Cited by in RCA: 406] [Article Influence: 81.2] [Reference Citation Analysis (0)] |
| 23. | Lindsley WG, Martin SB Jr, Thewlis RE, Sarkisian K, Nwoko JO, Mead KR, Noti JD. Effects of Ultraviolet Germicidal Irradiation (UVGI) on N95 Respirator Filtration Performance and Structural Integrity. J Occup Environ Hyg. 2015;12:509-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 179] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 24. | Mills D, Harnish DA, Lawrence C, Sandoval-Powers M, Heimbuch BK. Ultraviolet germicidal irradiation of influenza-contaminated N95 filtering facepiece respirators. Am J Infect Control. 2018;46:e49-e55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 176] [Cited by in RCA: 185] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 25. | Holmdahl T, Walder M, Uzcátegui N, Odenholt I, Lanbeck P, Medstrand P, Widell A. Hydrogen Peroxide Vapor Decontamination in a Patient Room Using Feline Calicivirus and Murine Norovirus as Surrogate Markers for Human Norovirus. Infect Control Hosp Epidemiol. 2016;37:561-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |