Published online Aug 7, 2013. doi: 10.3748/wjg.v19.i29.4732
Revised: April 15, 2013
Accepted: May 16, 2013
Published online: August 7, 2013
Processing time: 157 Days and 17.6 Hours
AIM: To compare the utility of single-balloon colonoscopy (SBC) or double-balloon colonoscopy (DBC) for difficult colonoscopies.
METHODS: Between August 2008 and June 2010, patients in whom total colonoscopy failed within 30 min of insertion were assigned randomly to undergo either SBC or DBC. No sedatives were used. After the endoscopy, all patients were asked to evaluate pain during the procedure on a 10-point analog scale (1 = no pain; 10 = worst imaginable pain) with a questionnaire. The study outcomes were the cecal intubation rate and time, endoscopic findings, complications, and pain score.
RESULTS: The SBC and DBC groups included 11 and 10 patients, respectively. All but one SBC patient achieved total colonoscopy successfully. The cecal intubation times were 18 min (range: 10-85 min) and 12.8 min (range: 9.5-42 min) in the SBC and DBC groups, respectively (P = 0.17). No difference was observed in the prevalence of colon polyps between the SBC and DBC groups (45% vs 30%, P = 0.66). SBC showed advanced colon cancer in the ascending colon, which was inaccessible using conventional colonoscopy. The respective pain scores were 5 (1-10) [median (range)] and 5 (1-6) in the SBC and DBC groups (P = 0.64). No complications were noted in any patient.
CONCLUSION: The utility of single- and double-balloon endoscopy for colonoscopy seems comparable in patients with incomplete colonoscopy using a conventional colonoscope.
Core tip: We compared the utility of single-balloon colonoscopy and double-balloon colonoscopy for difficult colonoscopy. Both single-balloon endoscopy (SBE) and double-balloon endoscopy (DBE) make possible performance of total colonoscopy in patients with incomplete colonoscopy using a conventional colonoscope. The utility of SBE and DBE for colonoscopy seems to be comparable. We recommend that patients with incomplete total colonoscopy undergo SBE or DBE.
- Citation: Yamada A, Watabe H, Takano N, Togo G, Yamaji Y, Yoshida H, Kawabe T, Omata M, Koike K. Utility of single and double balloon endoscopy in patients with difficult colonoscopy: A randomized controlled trial. World J Gastroenterol 2013; 19(29): 4732-4736
- URL: https://www.wjgnet.com/1007-9327/full/v19/i29/4732.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i29.4732
Optical colonoscopy is the gold standard for colorectal examination. Despite advances in colonoscopes and endoscopy techniques, total colonoscopy is still demanding technically. Total colonoscopy is unsuccessful in 5%-10% of patients for a number of reasons[1]. Difficult cecal intubation is associated with female gender, old age, a low body mass index, diverticular disease, and previous abdominal surgery[2-5]. Solutions to this problem are the use of pediatric colonoscopes[6] or a transparent hood[7].
Balloon endoscopy is an effective method for investigating the small intestine[8,9]. Two different types of balloon endoscopy are available: single-balloon endoscopy (SBE) and double-balloon endoscopy (DBE). Both can be performed using either the antegrade or retrograde approach. A retrograde approach might facilitate successful total colonoscopy and allow endoscopic therapy in patients who had incomplete colonoscopy with a conventional colonoscope. Although several studies have assessed the utility of single-balloon colonoscopy (SBC)[10-12] or double-balloon colonoscopy (DBC)[13-15] for colorectal examination, a difference between SBC and DBC has not yet been identified.
Therefore, we compared the utility of SBC and DBC for difficult colonoscopy in an exploratory randomized controlled trial.
Consecutive patients after a prior incomplete colonoscopy with a conventional colonoscope were candidates for this study. Incomplete colonoscopy was defined as failure to identify two landmarks, the ileocecal valve and appendiceal orifice, within 30 min or cancellation of colonoscopy due to intolerable pain during the procedure. The exclusion criteria were the following: incomplete colonoscopy due to poor bowel preparation or colonic stenosis, prior colectomy, inflammatory bowel disease, malignant tumor, poor general condition, pregnancy, having undergone successful total colonoscopy within 1 year, age younger than 20 years, and refusal to provide written informed consent.
To eliminate patient selection bias, the enrolled patients were assigned randomly to either the SBC or DBC group in a 1:1 ratio. Randomization was performed using a computer-generated list of random numbers. The endoscopists and patients were not blinded to the group assignment.
The study was conducted according to the Declaration of Helsinki and approved by the ethics committee of our institution. The Japanese clinical trial registration scheme (UMIN-CTR) registration number for the study was UMIN000001684. Written informed consent was obtained from each study participant.
Each balloon endoscopic examination was conducted by an endoscopist who had performed at least 30 balloon endoscopies. SBC was performed using an SIF-Q260 (Olympus Medical Systems, Tokyo, Japan), and DBC was performed using an EN-450T5 (FUJIFILM Medical, Tokyo, Japan). The study patients were administered 2 L of polyethylene glycol (PEG) solution before the procedure. Scopolamine butylbromide (20 mg) or glucagon (1 IU) was administered. No sedatives were used. Air insufflation was used during the both procedures. Fluoroscopy was used when stretching the scope or when the scope was stacked. We withdrew the endoscope when either the insertion time exceeded 90 min or the patient requested that the procedure be stopped. Cecal intubation was defined as successful when the ileocecal valve and appendiceal orifice were identified. Ancillary procedures such as polypectomy and biopsy were performed while withdrawing the scope after cecal intubation. While the patients were in the recovery room after the examination, they were asked to evaluate the pain during the examination on a 10-point analog scale (1 = no pain, 10 = worst imaginable pain) in a questionnaire.
The primary outcome was the successful cecal intubation rate. Secondary outcome measures were the cecal intubation time, endoscopic findings, complications, and pain score during the examination.
Categorical data including the total enteroscopy rate and diagnosis rate were compared using Fisher’s exact test. Continuous variables were compared using Student’s t-test. The cecal insertion time and X-ray fluoroscopy time were compared with the Mann-Whitney U-test. Differences with P < 0.05 were considered to indicate statistical significance. All statistical analyses were performed using JMP, ver. 9.0 (SAS Institute, Cary, NC, United States).
During the study period from August 2008 to June 2010, 21 patients were enrolled and assigned randomly to undergo either SBC (n = 11) or DBC (n = 10). Table 1 shows the baseline characteristics of the study patients. There was no significant difference between the SBC and DBC groups.
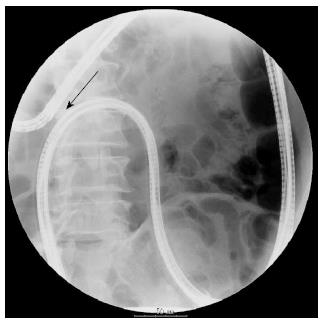
Table 2 shows the cecal intubation rate and endoscopy results. Using balloon endoscopy, cecal intubation was achieved in all cases but one patient who previously had abdominal surgery for cholecystitis and fluoroscopy showed adhesion between the sigmoid and transverse colons (Figure 1). The cecal intubation rate was 91% in the SBC group and 100% in the DBC group (P = 0.99). The median cecal intubation time of the successful cases did not differ between the SBC and DBC groups [18.0 min (range: 10-85 min) vs 12.8 min (range: 9.5-42 min), respectively, P = 0.17], neither did the X-ray fluoroscopy time [3 min (range: 1-7 min) vs 1 min (range: 1-5 min), P = 0.12). There was no difference in the pain score during the endoscopic procedure between the SBC and DBC groups [median (range), 5 (range: 1-10) vs 5 (range: 1-6), P = 0.64].
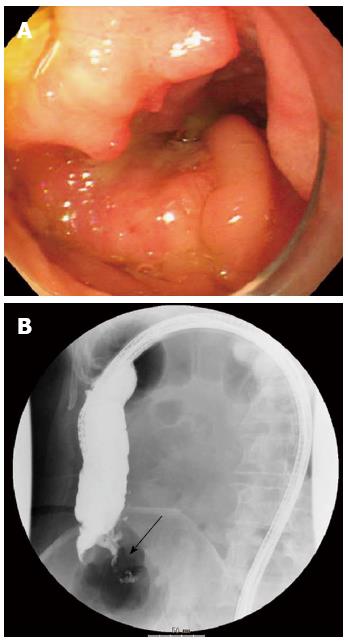
The diagnostic yield in each group is shown in Table 3. Colorectal polyps were detected in 8 of the 21 (38%) patients. All polyps were histologically confirmed as adenoma. The detection rate was 45% and 30% with SBC and DBC, respectively; the difference was not significant (P = 0.66). Moreover, SBC showed advanced colon cancer in the ascending colon, which was inaccessible by conventional colonoscopy (Figure 2).
No complications were noted in this study.
In our series, both SBE and DBE had high total colonoscopy rates in patients with incomplete colonoscopy using a conventional colonoscope. The utility of SBE and DBE for colonoscopy seems comparable.
Both SBE and DBE were initially designed for small bowel endoscopy and have proved their value for small bowel examination[9]. The endoscope and overtube are advanced sequentially with serial fixing and shortening of the small intestine using the balloons, in order to minimize looping and advance the scope. This balloon technique has already been used successfully for patients in whom colonoscopy is difficult. The reported total colonoscopy rate is 95%-100% for SBE[10-12], and 88%-100% for DBE[13-16]. Our total colonoscopy rates were comparable for SBE and DBE (91% vs 100%, P = 0.99). Previously, we reported that the total enteroscopy rate for the small intestine was higher with DBE than with SBE (57% vs 0%, P = 0.002)[17]. DBE grips the small intestine at the tip of the endoscope more easily than SBE, which makes possible deep insertion of the endoscope without redundant loops. When used for colonoscopy, the potential disadvantage of SBE seen in small intestinal endoscopy is negligible.
In our series, the cecal intubation time was comparable between SBC and DBC. Teshima et al[12] reported that SBE was faster than DBE because only one balloon cycle is used, as opposed to two. Compared with small intestinal endoscopy, colonoscopy is faster and requires fewer balloon cycles. Consequently, the simpler manipulation with SBE does not shorten the cecal intubation time.
The importance of total colonoscopy is well recognized, especially for older patients because of the increase in right-sided colon cancer with age[18,19]. Indeed, SBE detected advanced colon cancer in the ascending colon, which was inaccessible to conventional colonoscopy. In addition, we performed all procedures without any sedatives or complications. The study indicated that SBE and DBE can be performed safely in patients with incomplete total colonoscopy using a conventional colonoscope. Therefore, we recommend that patients with incomplete total colonoscopy undergo SBE or DBE.
The present study showed that SBC and DBC can be performed safely without sedation even in patients with incomplete total colonoscopy using a conventional colonoscope. In terms of colonoscopy, several papers reported that conventional colonoscopy without sedation is feasible, effective and well tolerated[20,21]. On the other side, most of previous papers regarding SBC and DBC used sedative drugs[11,12,14-16]. Although the pain score during for procedure was slightly high, all of the present study patients did not request to stop the procedure.
There were some limitations to this study. The number of participants was relatively small and a larger prospective non-inferiority trial is needed to elucidate any difference in the utility of SBE and DBE. However, the procedures had very high diagnostic yields in both groups, suggesting that both SBC and DBC are effective modalities for colonic examination.
In conclusion, both single- and double-balloon endoscopy make possible performance of total colonoscopy in patients with incomplete colonoscopy using a conventional colonoscope. The utility of SBE and DBE for colonoscopy seems to be comparable.
Despite advances in colonoscopes and endoscopy techniques, total colonoscopy still fails in some patients. Balloon endoscopy is an effective tool for investigating the small intestine. Two different types of balloon endoscopy are available commercially: single-balloon endoscopy (SBE) and double-balloon endoscopy (DBE). A retrograde approach might facilitate successful total colonoscopy and allow endoscopic therapy in patients who had incomplete colonoscopy with a conventional colonoscope. A difference between single-balloon colonoscopy (SBC) and double-balloon colonoscopy (DBC) has not yet been identified.
SBE and DBE can be used to complete examination of the colon in patients with incomplete colonoscopy using a conventional colonoscope. It also allows therapeutic interventions.
SBE and DBE have been an important endoscopic breakthrough for successful total colonoscopy and endoscopic therapy in patients who had incomplete colonoscopy with a conventional colonoscope. In this study, the authors compared the utility of SBC and DBC for difficult colonoscopy in an exploratory randomized controlled trial. The study indicated that both SBE and DBE make possible performance of total colonoscopy in patients with incomplete colonoscopy using a conventional colonoscope without any sedation. The utility of SBE and DBE for colonoscopy seems to be comparable.
This study suggests that patients with incomplete total colonoscopy undergo SBE or DBE.
DBE consists of an endoscope and a soft overtube. A latex balloon is attached to the tip of the endoscope and another to the tip of the overtube. Each balloon can be inflated and deflated by a pressure controlled air pump system. SBE is simpler to perform than DBE because it has only 1 balloon at the tip of the overtube. The equipment and techniques are different between DBE and SBE. However, the principle of insertion is the same; gripping the intestine by using balloon inflation prevents redundant loop formation and thus facilitates deep insertion of the endoscope.
The authors compared SBE with DBE in patients with previous incomplete colonoscopy because of several reasons. They achieved excellent total colonoscopy rates (91% vs 100%) even in these difficult cases. These results indicate the utility of SBE and DBE in patients with incomplete conventional colonoscopy.
P- Reviewers Racz I, Redondo-Cerezo E S- Editor Gou SX L- Editor A E- Editor Zhang DN
| 1. | Marshall JB, Barthel JS. The frequency of total colonoscopy and terminal ileal intubation in the 1990s. Gastrointest Endosc. 1993;39:518-520. [PubMed] [Cited in This Article: ] |
| 2. | Anderson JC, Gonzalez JD, Messina CR, Pollack BJ. Factors that predict incomplete colonoscopy: thinner is not always better. Am J Gastroenterol. 2000;95:2784-2787. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 148] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 3. | Anderson JC, Messina CR, Cohn W, Gottfried E, Ingber S, Bernstein G, Coman E, Polito J. Factors predictive of difficult colonoscopy. Gastrointest Endosc. 2001;54:558-562. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 165] [Cited by in F6Publishing: 181] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 4. | Takahashi Y, Tanaka H, Kinjo M, Sakumoto K. Prospective evaluation of factors predicting difficulty and pain during sedation-free colonoscopy. Dis Colon Rectum. 2005;48:1295-1300. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 83] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Cirocco WC, Rusin LC. Factors that predict incomplete colonoscopy. Dis Colon Rectum. 1995;38:964-968. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 132] [Cited by in F6Publishing: 140] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 6. | Kaffes AJ, Mishra A, Ding SL, Hope R, Williams SJ, Gillespie PE, Bourke MJ. A prospective trial of variable stiffness pediatric vs. standard instrument colonoscopy. Gastrointest Endosc. 2003;58:685-689. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Kondo S, Yamaji Y, Watabe H, Yamada A, Sugimoto T, Ohta M, Ogura K, Okamoto M, Yoshida H, Kawabe T. A randomized controlled trial evaluating the usefulness of a transparent hood attached to the tip of the colonoscope. Am J Gastroenterol. 2007;102:75-81. [PubMed] [Cited in This Article: ] |
| 8. | Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216-220. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 896] [Cited by in F6Publishing: 828] [Article Influence: 36.0] [Reference Citation Analysis (0)] |
| 9. | Yamamoto H, Kita H, Sunada K, Hayashi Y, Sato H, Yano T, Iwamoto M, Sekine Y, Miyata T, Kuno A. Clinical outcomes of double-balloon endoscopy for the diagnosis and treatment of small-intestinal diseases. Clin Gastroenterol Hepatol. 2004;2:1010-1016. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 10. | May A, Nachbar L, Ell C. Push-and-pull enteroscopy using a single-balloon technique for difficult colonoscopy. Endoscopy. 2006;38:395-398. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Keswani RN. Single-balloon colonoscopy versus repeat standard colonoscopy for previous incomplete colonoscopy: a randomized, controlled trial. Gastrointest Endosc. 2011;73:507-512. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Teshima CW, Aktas H, Haringsma J, Kuipers EJ, Mensink PB. Single-balloon-assisted colonoscopy in patients with previously failed colonoscopy. Gastrointest Endosc. 2010;71:1319-1323. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 13. | Kaltenbach T, Soetikno R, Friedland S. Use of a double balloon enteroscope facilitates caecal intubation after incomplete colonoscopy with a standard colonoscope. Dig Liver Dis. 2006;38:921-925. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 45] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Pasha SF, Harrison ME, Das A, Corrado CM, Arnell KN, Leighton JA. Utility of double-balloon colonoscopy for completion of colon examination after incomplete colonoscopy with conventional colonoscope. Gastrointest Endosc. 2007;65:848-853. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 77] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 15. | Hotta K, Katsuki S, Ohata K, Abe T, Endo M, Shimatani M, Nagaya T, Kusaka T, Matsuda T, Uraoka T. A multicenter, prospective trial of total colonoscopy using a short double-balloon endoscope in patients with previous incomplete colonoscopy. Gastrointest Endosc. 2012;75:813-818. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Suzuki T, Matsushima M, Tsukune Y, Fujisawa M, Yazaki T, Uchida T, Gocyo S, Okita I, Shirakura K, Sasao K. Double-balloon endoscopy versus magnet-imaging enhanced colonoscopy for difficult colonoscopies, a randomized study. Endoscopy. 2012;44:38-42. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Takano N, Yamada A, Watabe H, Togo G, Yamaji Y, Yoshida H, Kawabe T, Omata M, Koike K. Single-balloon versus double-balloon endoscopy for achieving total enteroscopy: a randomized, controlled trial. Gastrointest Endosc. 2011;73:734-739. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 137] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 18. | Okamoto M, Yamaji Y, Watabe H, Ikenoue T, Togo G, Kondo S, Ota M, Yoshida H, Kawabe T, Omata M. Older age and proximal location are the risk factors for metachronous advanced neoplasms after colorectal polypectomy: Analysis of cases with long-term colonoscopic surveillance. Gastrointest Endosc. 2004;59:AB279-AB279. [Cited in This Article: ] |
| 19. | Okamoto M, Kawabe T, Yamaji Y, Kato J, Ikenoue T, Togo G, Yoshida H, Shiratori Y, Omata M. Rectosigmoid findings are not associated with proximal colon cancer: analysis of 6 196 consecutive cases undergoing total colonoscopy. World J Gastroenterol. 2005;11:2249-2254. [PubMed] [Cited in This Article: ] |
| 20. | Petrini JL, Egan JV, Hahn WV. Unsedated colonoscopy: patient characteristics and satisfaction in a community-based endoscopy unit. Gastrointest Endosc. 2009;69:567-572. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 21. | Liao WC, Chiu HM, Chen CC, Lee YC, Wu MS, Lin JT, Wu AS, Wang HP. A prospective evaluation of the feasibility of primary screening with unsedated colonoscopy. Gastrointest Endosc. 2009;70:724-731. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |