Published online Feb 28, 2006. doi: 10.3748/wjg.v12.i8.1317
Revised: July 15, 2005
Accepted: July 28, 2005
Published online: February 28, 2006
Small bowel adenocarcinomas are remarkable for their rarity, difficult diagnosis and poor prognosis. Here we report an unusual case of a 33-year-old patient in whom infiltrative adenocarcinoma of the small bowel was diagnosed after a 10-year history of Crohn’s disease. In most previously reported cases, detection of Crohn’s disease was subsequent to that of carcinoma of the small bowel or the patients involved had an even longer history of the disease. Our literature review suggests that the risk of small bowel adenocarcinoma is higher in patients with Crohn’s disease than in the overall population. We present details on epidemiology as well as clinical and diagnostic aspects of this rare disease entity.
- Citation: Kronberger IE, Graziadei IW, Vogel W. Small bowel adenocarcinoma in Crohn’s disease: A case report and review of literature. World J Gastroenterol 2006; 12(8): 1317-1320
- URL: https://www.wjgnet.com/1007-9327/full/v12/i8/1317.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i8.1317
The incidence of inflammatory bowel disease (IBD) is increasing since World War II with levels around 6/100 000 for Crohn’s disease (CD) and 15 to 20/100 000 for ulcerative colitis, a marked rise in the age group between twenty to forty years for both entities[1].
The ulcerations occur primarily in the small and large intestines, but may appear anywhere in the digestive tract from the mouth to the anus. Common symptoms of CD are abdominal pain, often in the lower right area, and diarrhoea, but rectal bleeding, weight loss and fever may also appear. Children with CD may suffer stunted growth and delayed development. The severity of the symptoms fluctuates erratically over time. Patients experience flare-ups between intervals of remission or reduced symptoms. The causes of this disease have not been identified yet; but both genetic factors that induce continued abnormal activation of the immune system[2,3] and environmental triggers, like Mycobacterium avium subspecies paratuberculosis[4], are likely to be involved.
Oral or topical preparations of 5-aminosalicylates represent first line therapy, and steroids and azathioprine are used in severe cases; metronidazole and TNF-alpha antibodies are used in fistulating disease. Fifty to seventy percent of Crohn’s patients undergo surgery for progression of disease indicated by the presence of fistulas, tumor in the abdomen and development of ileus.
IBD is linked to large and small bowel carcinoma, especially to adenocarcinomas[5-7]. In the last twenty years, colorectal cancer has become the fourth most common cancer worldwide, and in Europe colorectal cancer represents the second most frequent cause of death from any cancer in men[8]. Even though only about 1% of all colorectal cancers is associated with ulcerative colitis or Crohn’s colitis, the risk of colorectal cancer for any ulcerative colitis patient is found to be 2% at 10, 8% at 20 and 18% at 30 years, duration of disease, regardless of disease extent[9,10].
Small bowel carcinomas are uncommon representing only 1% to 5% of all gastrointestinal tract malignancies. The first observations suggested that particularly surgically bypassed bowel segments were exposed to high risk of small bowel adenocarcinoma[11,12]. However, the risk of small bowel carcinoma in patients with CD is much higher, being up to 60-fold of that in the general population[13,14].
Neither clear risk factors nor methods for early diagnosis have been established by the few studies on this distinctly uncommon complication within this rare disease. Here we report on a patient in whom infiltrative adenocarcinoma of the ileum was diagnosed after a 10-year history of CD and also discuss possible risk factors, symptoms, feasible diagnostic approaches and treatment options on the basis of published reports.
A 33-year-old man presented in 1992 with recurrent pyrexia and abdominal pain but no diarrhoea. Enteroclysis was performed and a diagnosis of ileal CD was made. His family history was negative for this disease. For persistent abdominal pain under therapy with 5-aminosalicylates, he was put on corticosteroids (prednisone, 12.5 mg daily). In the following four years the patient experienced repeated episodes of abdominal pain without diarrhoea.
Two years later, an abdominal ultrasound performed for reassessment of the disease, showed a thick intestinal loop from the left to the right upper abdomen. Unfortunately no further diagnostic or therapeutic steps were undertaken at that time.
In 2002, the patient, complaining of increasing abdominal pain, underwent ileocolonoscopy, which yielded no suspicious macroscopic or histopathological findings. Blood tests showed mild anaemia, signs of malabsorption (low proteins, phosphorous and iron deficiency) but none for inflammation. The recommended enteroclysis of the small bowel was not performed. In order to reduce corticosteroids, therapy with azathioprine was initiated (2 mg/kg weight/ per day).
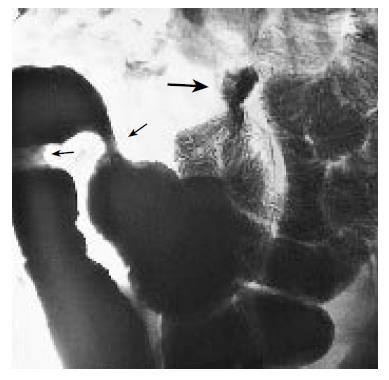
In June 2003 he presented again with abdominal pain, vomiting and distended abdomen. Enteroclysis showed a dilated intestinal loop of the ileum, a pseudotumor in the right abdomen and two stenotic areas, one of which was high-grade and located in the right upper abdomen (Figure 1).
Prednisone was increased to 50 mg/day, in addition to metronidazole and ciprofloxacine. Three weeks later, with a deterioration of obstructive symptoms, the patient underwent surgery.
The surgical specimens consisted of a 45 cm and a 7 cm long resected segments. Macroscopic examination showed high-grade inflammatory alteration of the ileum along a 20 cm segment and two upstream high-grade stenoses. The external surface of the diseased segment appeared brownish discoloured with adhering connective tissue. The internal surface of the ileum showed discontinuous mucous membrane, streaks of ulcers and whitened swelling of the bowel wall. Some foci had a ‘cobblestone’ appearance. The 7 cm long segment had a stenotic ‘sandglass’ formation.
Extensive histopathological examination in the first stricture revealed a poorly differentiated adenocarcinoma infiltrating the serosa, incipient infiltration of the mesenteric fat and lymphangiosis carcinomatosa as well as a metastatic peritoneal range. Tumor had seeded seven out of eleven lymph nodes examined. The resected specimen also showed adenoma’s dysplasia adjacent to the carcinoma. Extended antral metaplastic lesions within agglutinated villi up to one margin were found.
The second specimen revealed proper margins of resection. In the centre of the macroscopic stricture was another focus of the adenocarcinoma. In addition, moderately florid inflammatory infiltrates with acute erosions were detected, compatible with Crohn’s disease.
Immunohistochemistry was negative for NSE and chromogranin, only a few tumor cells were slightly positive for synaptophysin. CEA level determined only after surgery was 54.2 ng/ml (normal <50 ng/ml).
The patient recovered well from surgery and then underwent chemotherapy according to Folfox IV–scheme with oxaliplatin, 5-fluorouracil and leucovorin in six cycles. The patient tolerated the therapy quite well.
The computed tomography (CAT-scan) in October 2004 revealed up to two centimetres enlarged mesenteric and up to one centimetre enlarged retroperitoneal lymph nodes, without any further evidence for metastases. In November 2004 the patient presented with headache, vertigo and ambiopia and was diagnosed with meningeosis carcinomatosa. Intrathecal chemotherapy with methotrexate was started. He is now undergoing intrathecal chemotherapy with sustained-released cytarabine.
According to Parkin et al the age-standardized incidence of small intestine cancer (ICD-10 C17) ranges from 0.2 to 2.4 for males and from 0.2 to 1.8 for females worldwide[15]. The ‘Statistik Austria’ National Registry has 1384 documented cases of small intestine cancer between 1983-2000[16].
The association of CD with small bowel carcinoma is uncommon and to date only about 130 cases of small bowel carcinomas in patients with CD have been reported in the literature since the first description of this disease entity in 1956[17]. Cases and studies published in the last few decades, however, bear out from a 12-fold to an over 60-fold increased risk of small bowel cancer in CD[13,14,18]. This is in contrast to publications that still emphasize the popular position that CD is primarily associated with carcinoma of the colon. Adenocarcinoma is the most common forms of all small bowel malignancy and there appears to be an increased risk for developing ileal carcinoma in CD patients[19-23].
Most of ileal carcinoma in CD are located in strictures[11,24,25] and are often incidentally diagnosed postoperatively as in our case report. The occult carcinomas in strictures pose a challenge to diagnostic investigations using conventional modalities such as small bowel series and upper and lower gastrointestinal endoscopy. CT is now considered the imaging modality of choice[26-28], and a fat density target sign in CT[29] is also getting greater attention as reliable marker for diagnosing CD or even small bowel carcinoma. Abdominal MRI[30], double-contrast enteroclysis[31] and endoscopy[32], especially video wireless capsule endoscopy[33,34], are promising new diagnostic tools.
Other interesting characteristics are adjacent metaplasia, adenoma and epithelial dysplasia[35-38], which underline the importance of further research with respect to sequence-dysplasia in ileal adenocarcinomas in relation to Crohn’s disease.
Risk factors for small intestine carcinoma in CD are chronic active course with stricture, fistulas and onset of disease before the age of 30 years[25,39,40]. Further reported risk factors are: early onset, age between 30 and 50 years, male sex and smoking[13,14,41-45]. Therapy of CD with corticosteroids, azathioprine and TNF-alpha antibodies are also considered as potential risk factors. It has been suggested in previous studies that azathioprine, administered mostly combined with steroids to patients with a long history of Crohn’s disease, frequent recurrence or those allergic to 5-aminosalicylates has a carcinogenic potential[14,46-49]. In the light of these reports, it is interesting to raise the question whether azathioprine therapy initiated in our patient after normal ileocolonoscopy 18 mo before diagnosis of carcinoma might have contributed to the acceleration of the malignant disease. In contrast to azathioprine, 5-aminosalicylates are considered preventive against the development of large and small bowel adenocarcinoma in inflammatory bowel disease[13,23,50-53]. Mesalazine is now used for treating light to moderate Crohn’s colitis and ileitis postoperatively to maintain remissions, but its potential to prevent malignancy needs to be evaluated. TNF-alpha antibodies, also mostly combined with immunosuppression, are used in patients with refractory, steroid-dependent and fistulating CD. There is a theoretical risk of increased rate of malignancies due to antagonism of TNF-alpha, but to date there is no clear proof of such an effect[54-56].
Prognosis of small bowel adenocarcinoma is poor, and the mortality at 1 and 2 years ranges from 30-60% dependent on the stage of the cancer[13,21,57-59].
Further prognostic factors are based on histologic findings such as positive surgical margins, poor differentiation, depth of tumor invasion, positive lymph nodes and extramural venous spread in small bowel adenocarcinoma[60].
Small bowel adenocarcinoma in Crohn’s disease is rare and preoperative diagnosis continues to present challenges. Long-term prognosis is poor - all the more it is important to be vigilant. Patients with increased risk are those with longstanding complicated CD presenting with a ‘de novo’ clinical picture of obstruction. Male patients, in particular smokers, are considered to be at increased risk. Since the diagnosis is difficult to make, attending physicians must exercise a high level of clinical suspicion for operative cure. The preventive potential of 5-ASA in adenocarcinoma of the colon suggests that this drug should be preferred to azathioprine in patients to maintain remission.
S- Editor Guo SY L- Editor Zhang JZ E- Editor Cao L
| 1. | Ekbom A. The epidemiology of IBD: a lot of data but little knowledge. How shall we proceed. Inflamm Bowel Dis. 2004;10 Suppl 1:S32-S34. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 51] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | Oostenbrug LE, van Dullemen HM, te Meerman GJ, Jansen PL. IBD and genetics: new developments. Scand J Gastroenterol Suppl. 2003;63-68. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Esters N, Pierik M, van Steen K, Vermeire S, Claessens G, Joossens S, Vlietinck R, Rutgeerts P. Transmission of CARD15 (NOD2) variants within families of patients with inflammatory bowel disease. Am J Gastroenterol. 2004;99:299-305. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 46] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Greenstein RJ. Is Crohn's disease caused by a mycobacterium Comparisons with leprosy, tuberculosis, and Johne's disease. Lancet Infect Dis. 2003;3:507-514. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 242] [Cited by in F6Publishing: 218] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 5. | Torres C, Antonioli D, Odze RD. Polypoid dysplasia and adenomas in inflammatory bowel disease: a clinical, pathologic, and follow-up study of 89 polyps from 59 patients. Am J Surg Pathol. 1998;22:275-284. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 150] [Cited by in F6Publishing: 143] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 6. | Munkholm P. Review article: the incidence and prevalence of colorectal cancer in inflammatory bowel disease. Aliment Pharmacol Ther. 2003;18 Suppl 2:1-5. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 376] [Cited by in F6Publishing: 381] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 7. | Langholz E, Munkholm P, Davidsen M, Binder V. Colorectal cancer risk and mortality in patients with ulcerative colitis. Gastroenterology. 1992;103:1444-1451. [PubMed] [Cited in This Article: ] |
| 8. | Boyle P, Langman JS. ABC of colorectal cancer: Epidemiology. BMJ. 2000;321:805-808. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 309] [Cited by in F6Publishing: 320] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 9. | Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001;48:526-535. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1985] [Cited by in F6Publishing: 1984] [Article Influence: 86.3] [Reference Citation Analysis (0)] |
| 10. | Judge TA, Lewis JD, Lichtenstein GR. Colonic dysplasia and cancer in inflammatory bowel disease. Gastrointest Endosc Clin N Am. 2002;12:495-523. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Barwood N, Platell C. Case report: adenocarcinoma arising in a Crohn's stricture of the jejunum. J Gastroenterol Hepatol. 1999;14:1132-1134. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Mohan IV, Kurian KM, Howd A. Crohn's disease presenting as adenocarcinoma of the small bowel. Eur J Gastroenterol Hepatol. 1998;10:431-432. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Solem CA, Harmsen WS, Zinsmeister AR, Loftus EV Jr. Small intestinal adenocarcinoma in Crohn's disease: a case-control study. Inflamm Bowel Dis. 2004;10:32-35. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 72] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 14. | Jess T, Winther KV, Munkholm P, Langholz E, Binder V. Intestinal and extra-intestinal cancer in Crohn's disease: follow-up of a population-based cohort in Copenhagen County, Denmark. Aliment Pharmacol Ther. 2004;19:287-293. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 169] [Cited by in F6Publishing: 109] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 15. | Parkin DM, Whelan SL, Forlay J, Teppo L, Thomas DB, eds . Age-standardized (world) incidence (per 100,000) and cumulative (0-74) incidence (percent) rates and standard errors. Incidence in Five Continents Vol. VIII, No. 155, Lyon: IARC Scientific Publications 2002; 549-551. [Cited in This Article: ] |
| 16. | Austrian Statistics. Incidence and Mortality of small intestine cancer, Mortality of Crohn's disease 1983-2000. Vienna: Statistik Austria 2004; . [Cited in This Article: ] |
| 17. | Koga H, Aoyagi K, Hizawa K, Iida M, Jo Y, Yao T, Oohata Y, Mibu R, Fujishima M. Rapidly and infiltratively growing Crohn's carcinoma of the small bowel: serial radiologic findings and a review of the literature. Clin Imaging. 1999;23:298-301. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Lewis JD, Deren JJ, Lichtenstein GR. Cancer risk in patients with inflammatory bowel disease. Gastroenterol Clin North Am. 1999;28:459-477, x. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 104] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 19. | Nesbit RR Jr, Elbadawi NA, Morton JH, Cooper RA Jr. Carcinoma of the small bowel. A complication of regional enteritis. Cancer. 1976;37:2948-2959. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 20. | Beachley MC, Lebel A, Lankau CA Jr, Rothman D, Baldi A. Carcinoma of the small intestine in chronic regional enteritis. Am J Dig Dis. 1973;18:1095-1098. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 16] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Michelassi F, Testa G, Pomidor WJ, Lashner BA, Block GE. Adenocarcinoma complicating Crohn's disease. Dis Colon Rectum. 1993;36:654-661. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 70] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Frank JD, Shorey BA. Adenocarcinoma of the small bowel as a complication of Crohn's disease. Gut. 1973;14:120-124. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 45] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | Bernstein CN, Blanchard JF, Kliewer E, Wajda A. Cancer risk in patients with inflammatory bowel disease: a population-based study. Cancer. 2001;91:854-862. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 14] [Reference Citation Analysis (0)] |
| 24. | Marchetti F, Fazio VW, Ozuner G. Adenocarcinoma arising from a strictureplasty site in Crohn's disease. Report of a case. Dis Colon Rectum. 1996;39:1315-1321. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 61] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 25. | Partridge SK, Hodin RA. Small bowel adenocarcinoma at a strictureplasty site in a patient with Crohn's disease: report of a case. Dis Colon Rectum. 2004;47:778-781. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 39] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 26. | Furukawa A, Saotome T, Yamasaki M, Maeda K, Nitta N, Takahashi M, Tsujikawa T, Fujiyama Y, Murata K, Sakamoto T. Cross-sectional imaging in Crohn disease. Radiographics. 2004;24:689-702. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 194] [Cited by in F6Publishing: 135] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 27. | Horton KM, Fishman EK. Multidetector-row computed tomography and 3-dimensional computed tomography imaging of small bowel neoplasms: current concept in diagnosis. J Comput Assist Tomogr. 2004;28:106-116. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 68] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 28. | Buckley JA, Siegelman SS, Jones B, Fishman EK. The accuracy of CT staging of small bowel adenocarcinoma: CT/pathologic correlation. J Comput Assist Tomogr. 1997;21:986-991. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 29. | Chen S, Harisinghani MG, Wittenberg J. Small bowel CT fat density target sign in chronic radiation enteritis. Australas Radiol. 2003;47:450-452. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Schreyer AG, Geissler A, Albrich H, Schölmerich J, Feuerbach S, Rogler G, Völk M, Herfarth H. Abdominal MRI after enteroclysis or with oral contrast in patients with suspected or proven Crohn's disease. Clin Gastroenterol Hepatol. 2004;2:491-497. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 133] [Cited by in F6Publishing: 138] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 31. | Zhan J, Xia ZS, Zhong YQ, Zhang SN, Wang LY, Shu H, Zhu ZH. Clinical analysis of primary small intestinal disease: A report of 309 cases. World J Gastroenterol. 2004;10:2585-2587. [PubMed] [Cited in This Article: ] |
| 32. | Mpofu C, Watson AJ, Rhodes JM. Strategies for detecting colon cancer and/or dysplasia in patients with inflammatory bowel disease. Cochrane Database Syst Rev. 2004;CD000279. [PubMed] [Cited in This Article: ] |
| 33. | Voderholzer WA, Ortner M, Rogalla P, Beinhölzl J, Lochs H. Diagnostic yield of wireless capsule enteroscopy in comparison with computed tomography enteroclysis. Endoscopy. 2003;35:1009-1014. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 144] [Cited by in F6Publishing: 152] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 34. | Jungles SL. Video wireless capsule endoscopy: a diagnostic tool for early Crohn's disease. Gastroenterol Nurs. 2004;27:170-175. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 35. | Sigel JE, Petras RE, Lashner BA, Fazio VW, Goldblum JR. Intestinal adenocarcinoma in Crohn's disease: a report of 30 cases with a focus on coexisting dysplasia. Am J Surg Pathol. 1999;23:651-655. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 99] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 36. | Rashid A, Hamilton SR. Genetic alterations in sporadic and Crohn's-associated adenocarcinomas of the small intestine. Gastroenterology. 1997;113:127-135. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 81] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 37. | Petras RE, Mir-Madjlessi SH, Farmer RG. Crohn's disease and intestinal carcinoma. A report of 11 cases with emphasis on associated epithelial dysplasia. Gastroenterology. 1987;93:1307-1314. [PubMed] [Cited in This Article: ] |
| 38. | Jankowski JA, Bedford FK, Boulton RA, Cruickshank N, Hall C, Elder J, Allan R, Forbes A, Kim YS, Wright NA. Alterations in classical cadherins associated with progression in ulcerative and Crohn's colitis. Lab Invest. 1998;78:1155-1167. [PubMed] [Cited in This Article: ] |
| 39. | Lashner BA. Risk factors for small bowel cancer in Crohn's disease. Dig Dis Sci. 1992;37:1179-1184. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 64] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 40. | Christodoulou D, Skopelitou AS, Katsanos KH, Katsios C, Agnantis N, Price A, Kappas A, Tsianos EV. Small bowel adenocarcinoma presenting as a first manifestation of Crohn's disease: report of a case, and a literature review. Eur J Gastroenterol Hepatol. 2002;14:805-810. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 41. | Kaerlev L, Teglbjaerg PS, Sabroe S, Kolstad HA, Ahrens W, Eriksson M, Guénel P, Hardell L, Launoy G, Merler E. Medical risk factors for small-bowel adenocarcinoma with focus on Crohn disease: a European population-based case-control study. Scand J Gastroenterol. 2001;36:641-646. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 42. | Lightdale CJ, Sternberg SS, Posner G, Sherlock P. Carcinoma complicating Crohn's disease. Report of seven cases and review of the literature. Am J Med. 1975;59:262-268. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 87] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 43. | Church JM, Weakley FL, Fazio VW, Sebek BA, Achkar E, Carwell M. The relationship between fistulas in Crohn's disease and associated carcinoma. Report of four cases and review of the literature. Dis Colon Rectum. 1985;28:361-366. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 47] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 44. | Munkholm P, Langholz E, Davidsen M, Binder V. Intestinal cancer risk and mortality in patients with Crohn's disease. Gastroenterology. 1993;105:1716-1723. [PubMed] [Cited in This Article: ] |
| 45. | Sandmeier D, Bouzourene H. Adenocarcinoma in Crohn's disease. Histopathology. 2003;42:404-405. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 46. | Westaby S, Everett WG, Dick AP. Adenocarcinoma of the small bowel complicating Crohn's disease in a patient treated with azathioprine. Clin Oncol. 1977;3:377-381. [PubMed] [Cited in This Article: ] |
| 47. | Fraser AG, Orchard TR, Robinson EM, Jewell DP. Long-term risk of malignancy after treatment of inflammatory bowel disease with azathioprine. Aliment Pharmacol Ther. 2002;16:1225-1232. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 148] [Cited by in F6Publishing: 153] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 48. | Connell WR, Kamm MA, Dickson M, Balkwill AM, Ritchie JK, Lennard-Jones JE. Long-term neoplasia risk after azathioprine treatment in inflammatory bowel disease. Lancet. 1994;343:1249-1252. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 364] [Cited by in F6Publishing: 317] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 49. | van Hogezand RA, Eichhorn RF, Choudry A, Veenendaal RA, Lamers CB. Malignancies in inflammatory bowel disease: fact or fiction. Scand J Gastroenterol Suppl. 2002;48-53. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 44] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 50. | Lim WC, Hanauer SB. Controversies with aminosalicylates in inflammatory bowel disease. Rev Gastroenterol Disord. 2004;4:104-117. [PubMed] [Cited in This Article: ] |
| 51. | Allgayer H. Review article: mechanisms of action of mesalazine in preventing colorectal carcinoma in inflammatory bowel disease. Aliment Pharmacol Ther. 2003;18 Suppl 2:10-14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 72] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 52. | Moody GA, Jayanthi V, Probert CS, Mac Kay H, Mayberry JF. Long-term therapy with sulphasalazine protects against colorectal cancer in ulcerative colitis: a retrospective study of colorectal cancer risk and compliance with treatment in Leicestershire. Eur J Gastroenterol Hepatol. 1996;8:1179-1183. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 170] [Cited by in F6Publishing: 172] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 53. | Ryan BM, Russel MG, Langholz E, Stockbrugger RW. Aminosalicylates and colorectal cancer in IBD: a not-so bitter pill to swallow. Am J Gastroenterol. 2003;98:1682-1687. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 54. | Tilg H, Knoflach P, Petritsch W, Vogelsang H, Reinisch W. [Infliximab in the treatment of Crohn's disease -- a practical approach. Infliximab and chronic Crohn's disease--Consensus statement of the Working Group on Chronic Inflammatory Crohn's Diseases of the OGGH]. Z Gastroenterol. 2004;42:1256-1263. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 55. | Wenzl HH, Reinisch W, Jahnel J, Stockenhuber F, Tilg H, Kirchgatterer A, Petritsch W. Austrian infliximab experience in Crohn's disease: a nationwide cooperative study with long-term follow-up. Eur J Gastroenterol Hepatol. 2004;16:767-773. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 56. | Dotan I, Yeshurun D, Hallak A, Horowitz N, Tiomny E, Reif S, Halpern Z, Rachmilewitz D. [Treatment of Crohn's disease with anti TNF alpha antibodies--the experience in the Tel Aviv Medical Center]. Harefuah. 2001;140:289-93, 368. [PubMed] [Cited in This Article: ] |
| 57. | Dabaja BS, Suki D, Pro B, Bonnen M, Ajani J. Adenocarcinoma of the small bowel: presentation, prognostic factors, and outcome of 217 patients. Cancer. 2004;101:518-526. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 357] [Cited by in F6Publishing: 327] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 58. | Ribeiro MB, Greenstein AJ, Heimann TM, Yamazaki Y, Aufses AH Jr. Adenocarcinoma of the small intestine in Crohn's disease. Surg Gynecol Obstet. 1991;173:343-349. [PubMed] [Cited in This Article: ] |
| 59. | Hawker PC, Gyde SN, Thompson H, Allan RN. Adenocarcinoma of the small intestine complicating Crohn's disease. Gut. 1982;23:188-193. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 61] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 60. | Abrahams NA, Halverson A, Fazio VW, Rybicki LA, Goldblum JR. Adenocarcinoma of the small bowel: a study of 37 cases with emphasis on histologic prognostic factors. Dis Colon Rectum. 2002;45:1496-1502. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 80] [Article Influence: 3.6] [Reference Citation Analysis (0)] |