Copyright
©The Author(s) 2021.
World J Gastroenterol. Sep 21, 2021; 27(35): 5803-5821
Published online Sep 21, 2021. doi: 10.3748/wjg.v27.i35.5803
Published online Sep 21, 2021. doi: 10.3748/wjg.v27.i35.5803
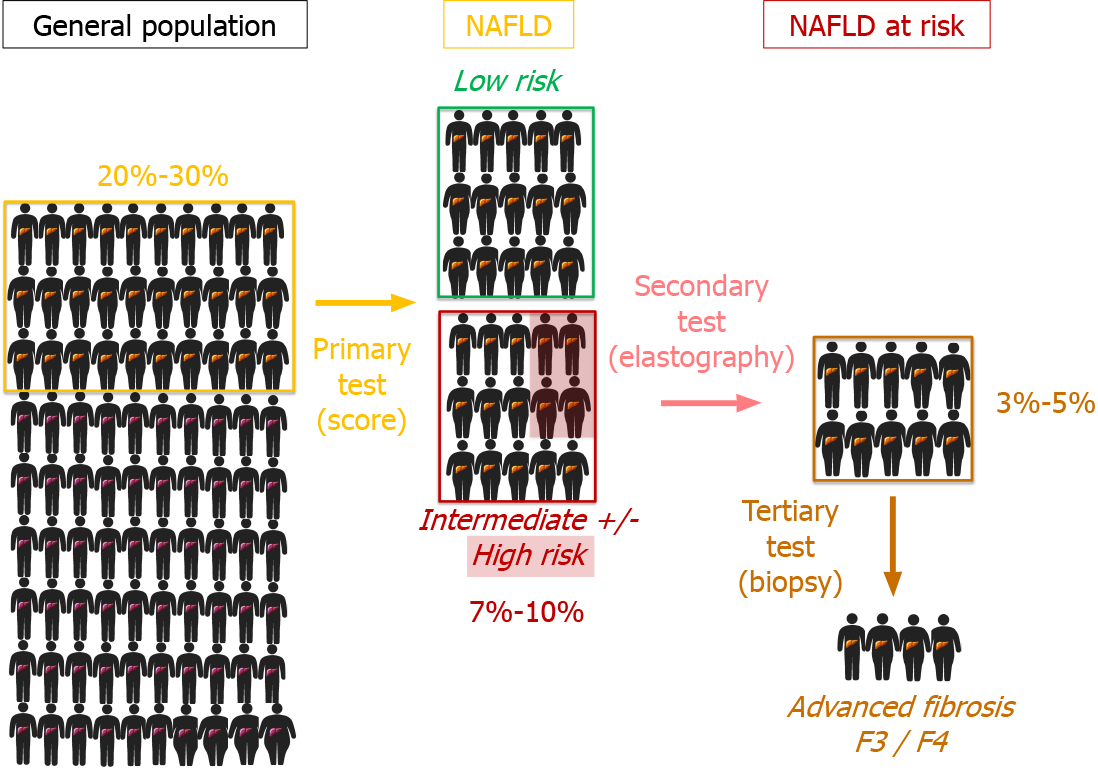
Figure 1 Nonalcoholic fatty liver disease patient proportions according to risk assessment.
Stepwise enrichment of nonalcoholic fatty liver disease (NAFLD) patients at risk for advanced fibrosis using a three-step strategy with score-based primary testing in a subgroup of the general population at risk for NAFLD and elastometric secondary testing to identify candidate patients for liver biopsy represents the third and final step in most algorithms. Patients with a diagnosis of NAFLD by either surrogate scores or ultrasound (20%-30% of the general population) are divided into low-risk vs intermediate-to-high-risk subgroups (the latter 7%-10% of the general population). After elastometry testing, half of these subjects can be assigned to a high likelihood of advanced fibrosis F3/F4 and should be subjected to liver biopsy. NAFLD: Nonalcoholic fatty liver disease.
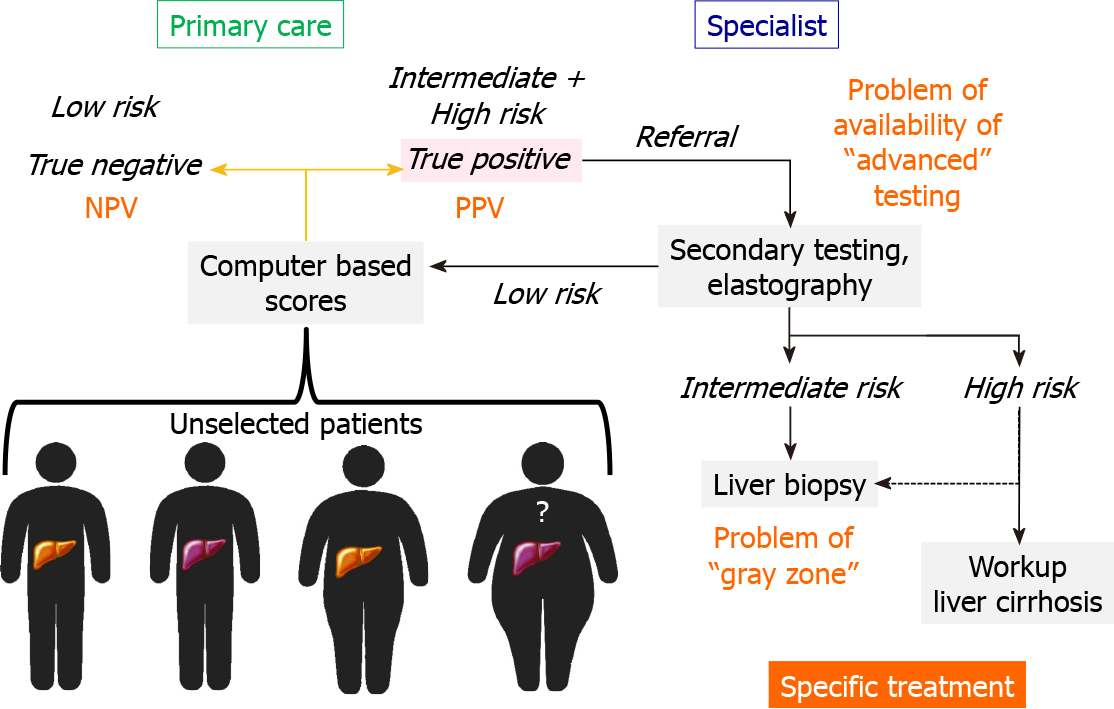
Figure 2 Linking primary care to hepatology.
Unselected patients from the general population are most likely in contact with primary care. In primary care, patients at risk for the presence of nonalcoholic fatty liver disease and according to computer-based scores at risk for advanced fibrosis should be transferred into secondary testing facilities at a specialist setting. Critical for the overall efficacy of a screening algorithm are the likelihood of referral of “intermediate or high risk” individuals to secondary care, the proportion of subjects with “indeterminate” test results (“gray zone” of score-based tests) and the availability of advanced testing platforms for referral. NPV: Negative predictive value; PPV: Positive predictive value.
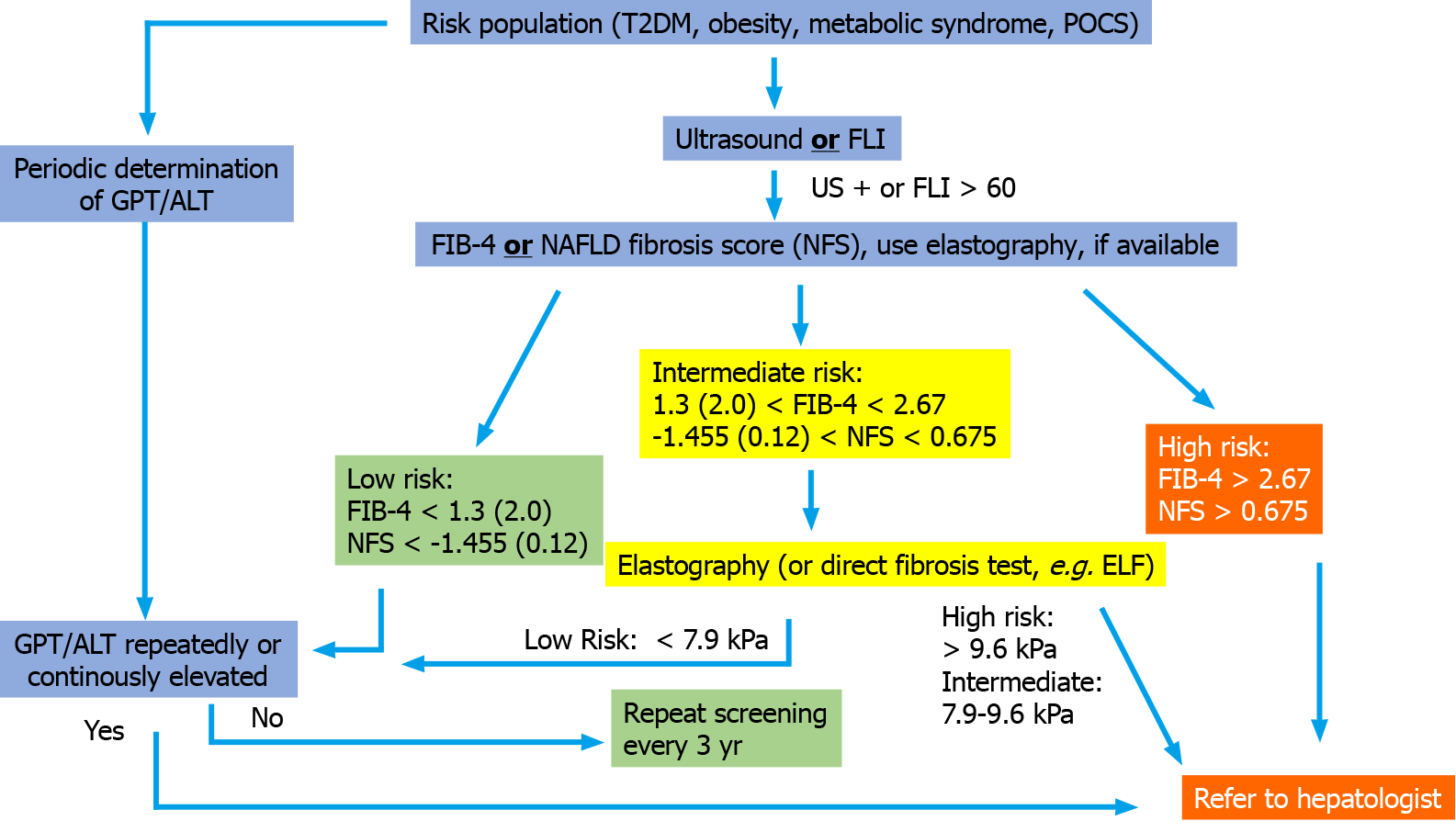
Figure 3 Possible screening algorithm that can be modified according to availability but contains the two main elements (detection of steatosis and fibrosis risk) and can be performed in the primary care physician’s office.
The algorithm corresponds well to the so-called European algorithm of the EASL-EASD-EASO Clinical Practice Guidelines[6] and to a recently proposed approach for family physicians and diabetologists[68] but is simpler to use. The sequences of fatty liver index and Fibrosis-4 (FIB-4) have been decisively studied for screening in a high-risk population of type 2 diabetes patients[65]. The use of age-adjusted cutoff values (in parentheses) is reasonable to reduce the high proportion of intermediate tested individuals. The sequential use of FIB-4, nonalcoholic fatty liver disease fibrosis score or enhanced liver fibrosis in the intermediate group has not been investigated in studies so far, but there are first studies on the basic sequential use of noninvasive fibrosis scores[123]. FLI: Fatty liver index; FIB-4: Fibrosis-4; T2DM: Type 2 diabetes mellitu; NFS: Nonalcoholic fatty liver disease fibrosis score; GPT: Glutamate pyruvate transaminase; ALT: Alanine aminotransferase.
- Citation: Dietrich CG, Rau M, Geier A. Screening for nonalcoholic fatty liver disease-when, who and how? World J Gastroenterol 2021; 27(35): 5803-5821
- URL: https://www.wjgnet.com/1007-9327/full/v27/i35/5803.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i35.5803