Copyright
©The Author(s) 2021.
World J Gastroenterol. Jul 21, 2021; 27(27): 4322-4341
Published online Jul 21, 2021. doi: 10.3748/wjg.v27.i27.4322
Published online Jul 21, 2021. doi: 10.3748/wjg.v27.i27.4322
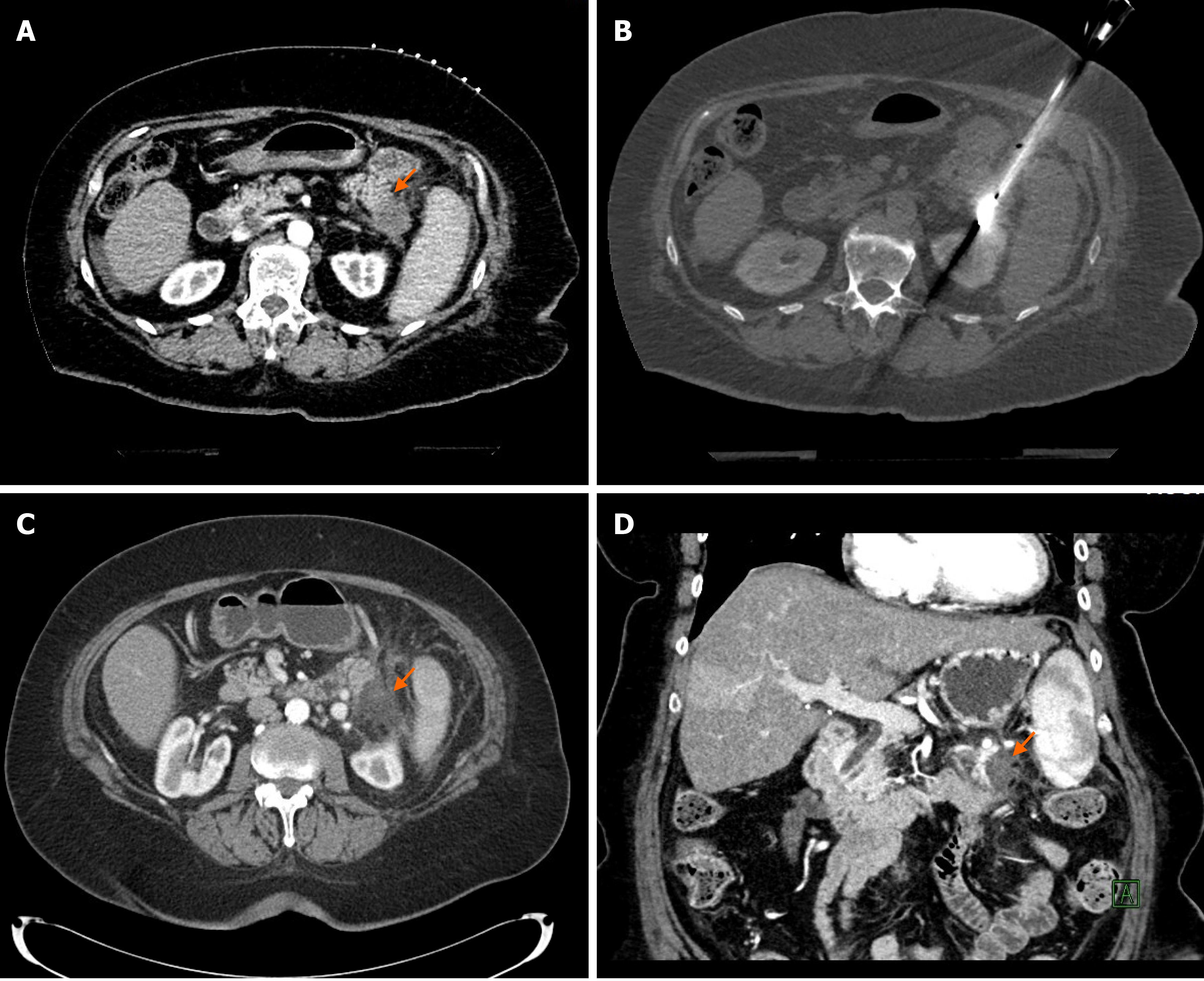
Figure 1 Percutaneous computed tomography-guided microwave ablation of a pancreatic tail adenocarcinoma.
A: 72-year-old patient presented with a 1.9 cm biopsy-proven pancreatic adenocarcinoma in the tail of the pancreas as it shown on this contrast-enhanced computed tomography (CT) image (orange arrow); B: The patient was not surgical candidate due to comorbidities and underwent percutaneous CT-guided microwave ablation (MWA) of the pancreatic tumor. CT image shows the microwave antenna in place in the pancreatic tail tumor; C and D: Axial and coronal contrast-enhanced CT images 6 wk after the MWA show good radiological response with an avascular area in the tail of the pancreas corresponding to the ablation zone (orange arrows). Patient developed peritoneal metastases 4 mo later and died 13 mo after the MWA treatment.
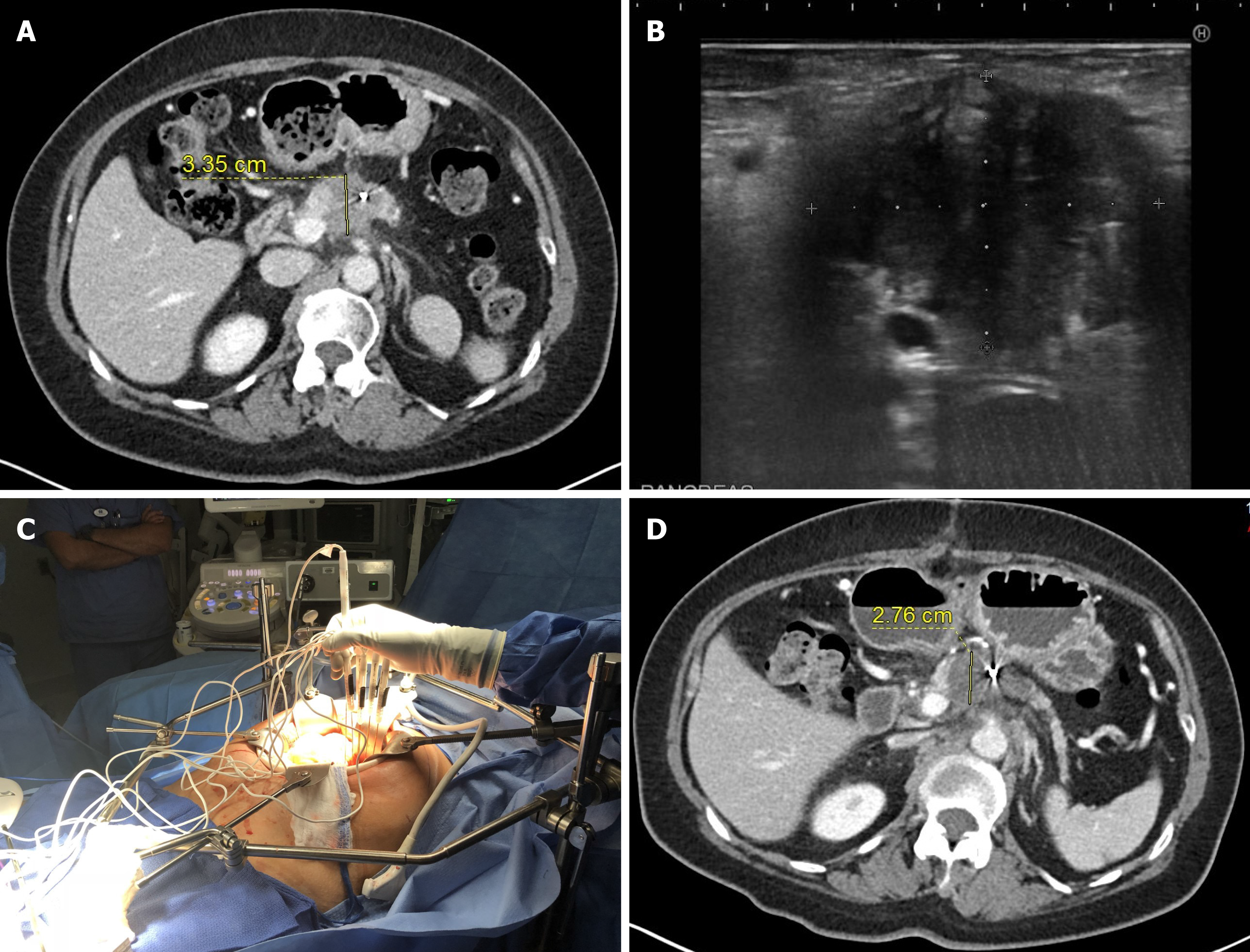
Figure 2 Intraoperative irreversible electroporation of a pancreatic adenocarcinoma.
A: Pre-operative contrast-enhanced computed tomography image shows a hypodense mass in the head of the pancreas. A hyperdense fiducial marker, which was placed for prior radiation therapy, is also visible in the mass; B: Intraoperative ultrasound image shows 4 Í 3.2 cm hypoechoic mass in the pancreas; C: Intraoperative photo shows the patient with upper median laparotomy with ablation probes are placed directly into the pancreatic tumor, using ultrasound guidance; D: Follow-up imaging 1 mo after the irreversible electroporation (IRE) showed an avascular ablation zone covering the previously seen pancreatic tumor. The CA19-9 tumor marker decreased from 959 U/mL to 76 U/mL 1 mo after the ablation. The patient is still alive 31 mo after the IRE ablation.
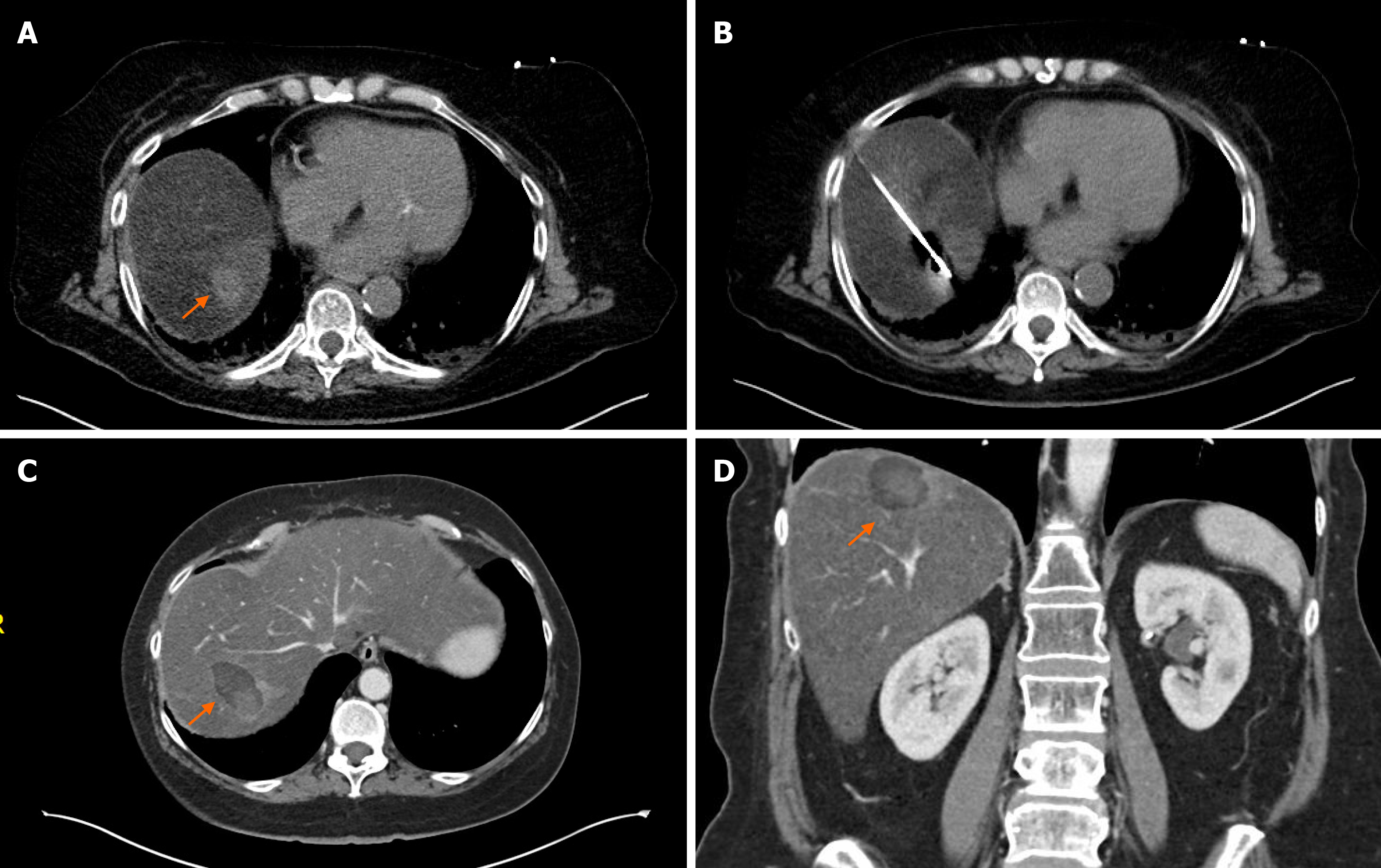
Figure 3 Percutaneous computed tomography-guided microwave ablation of a solitary pancreatic adenocarcinoma liver metastasis.
A: 62-year-old female presented with a 2 cm solitary liver metastasis (orange arrow), 9 mo after the surgical resection of the primary tumor from the pancreatic head; B: Intraprocedural image shows the microwave antenna in the liver metastasis; C and D: Axial and coronal contrast-enhanced computed tomography images 1 mo after the ablation demonstrates a 4.3 Í 2.7 cm hypodense ablation zone (orange arrows). There was no evidence of residual or new metastases in the liver. Patient is currently on systemic therapy 2 mo after the ablation without evidence of disease.
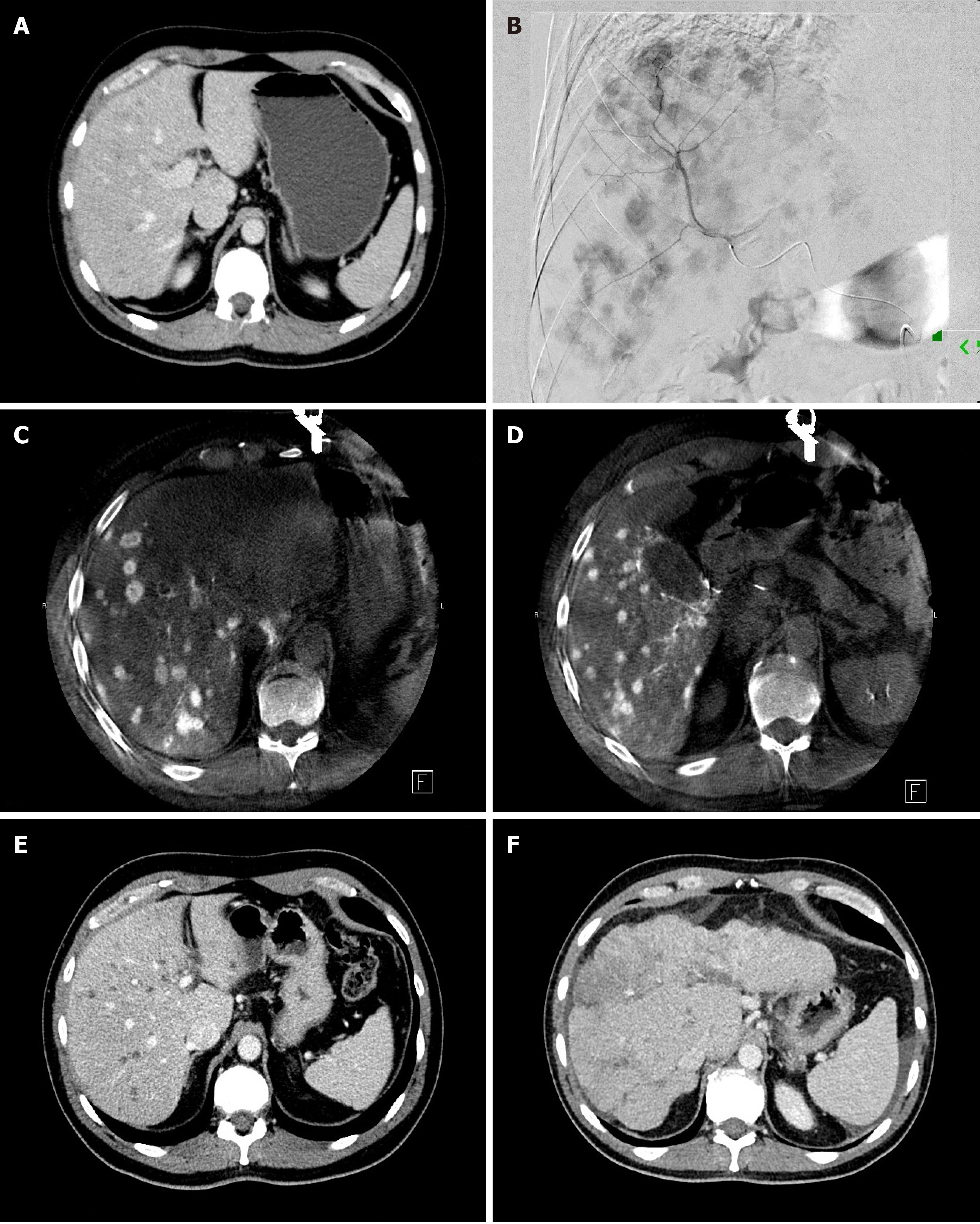
Figure 4 Transarterial radioembolization of pancreatic adenocarcinoma liver metastases.
A: Pre-treatment contrast-enhanced computed tomography (CT) image of a 45-year-old man with pancreatic cancer demonstrates bilobar multifocal mildly hypodense liver metastases; B: Hepatic angiogram with contrast injection into the anterior division of the right hepatic artery shows multifocal arterially enhancing liver metastases; C and D: Intra-procedural cone-beam CT images of the liver during selective contrast injection into right hepatic artery shows multifocal arterially enhancing liver metastases; E: Contrast-enhanced CT image 1 mo after bilobar transarterial radioembolization (TARE) shows hypodense, “burnt out” liver metastases. The patient CA19-9 Level decreased from 882 U/mL pre-procedure to 56 U/mL. One year after the initial TARE new liver lesions appeared and his CA19-9 increased to 530 U/mL. He underwent a second round of bilobar TARE, and his CA19-9 Level decreased to 233 U/mL; F: Contrast-enhanced CT image 18 mo after the initial TARE shows shrunken liver with lobulated, nodular borders consistent with TARE-induced pseudocirrhosis. The patient died 22 mo after the initial TARE due to extrahepatic and hepatic progression of his disease.
- Citation: Bibok A, Kim DW, Malafa M, Kis B. Minimally invasive image-guided therapy of primary and metastatic pancreatic cancer. World J Gastroenterol 2021; 27(27): 4322-4341
- URL: https://www.wjgnet.com/1007-9327/full/v27/i27/4322.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i27.4322