Copyright
©The Author(s) 2021.
World J Gastroenterol. May 7, 2021; 27(17): 1864-1882
Published online May 7, 2021. doi: 10.3748/wjg.v27.i17.1864
Published online May 7, 2021. doi: 10.3748/wjg.v27.i17.1864
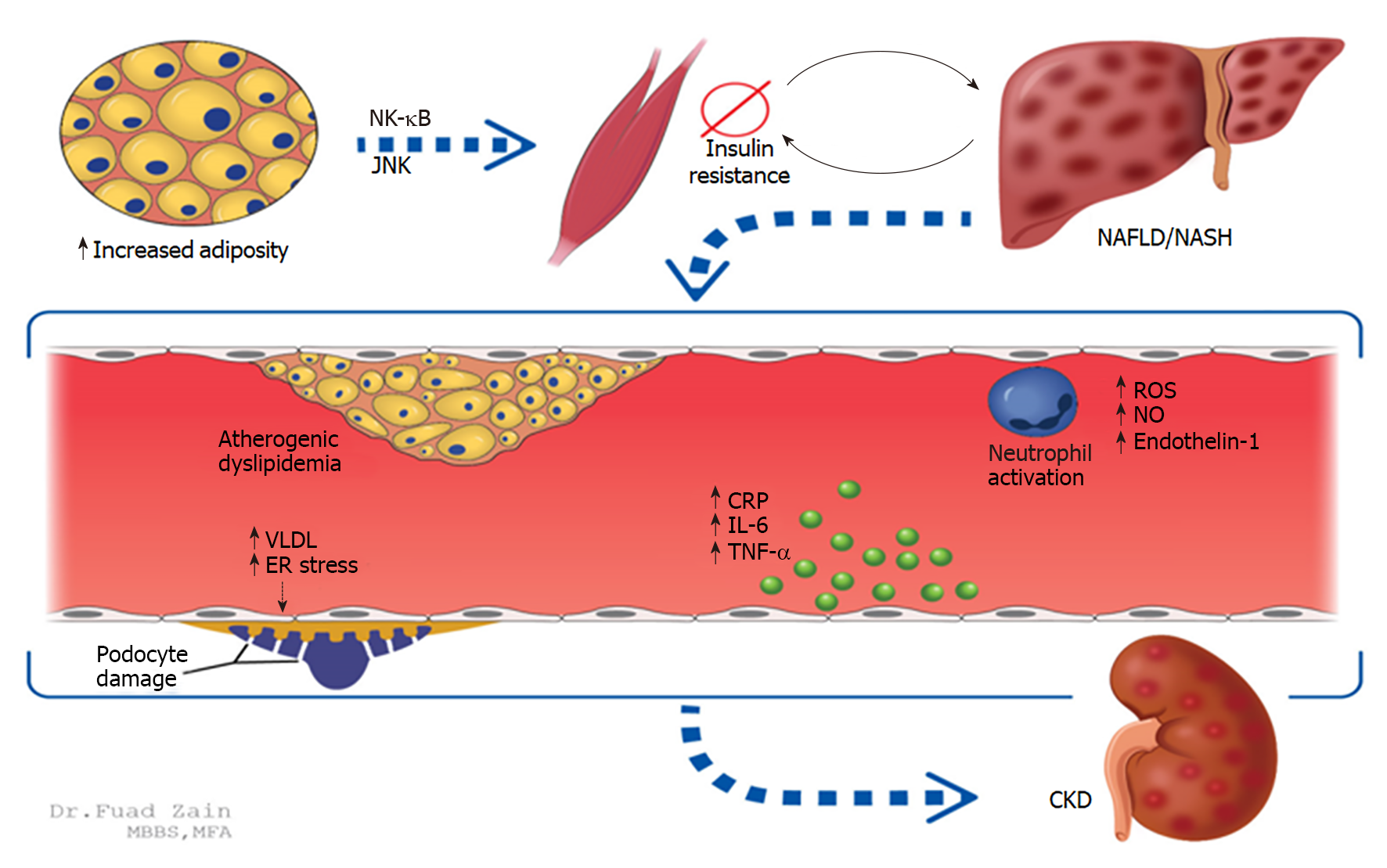
Figure 1 Two established mechanisms between non-alcoholic fatty liver disease and the development of chronic kidney disease are increased adiposity and insulin resistance.
NF-κB: Nuclear factor-κB; JNK: Jun N-terminal kinases; NAFLD/NASH: Non-alcoholic fatty liver disease/Non-alcoholic steatohepatitis; ROS: Reactive oxygen species; NO: Nitric oxide; CRP: C-reactive protein; IL-6: Interleukin-6; VLDL: Very low-density lipoprotein; TNF-α: Tumor necrosis factor alpha; CKD: Chronic kidney disease
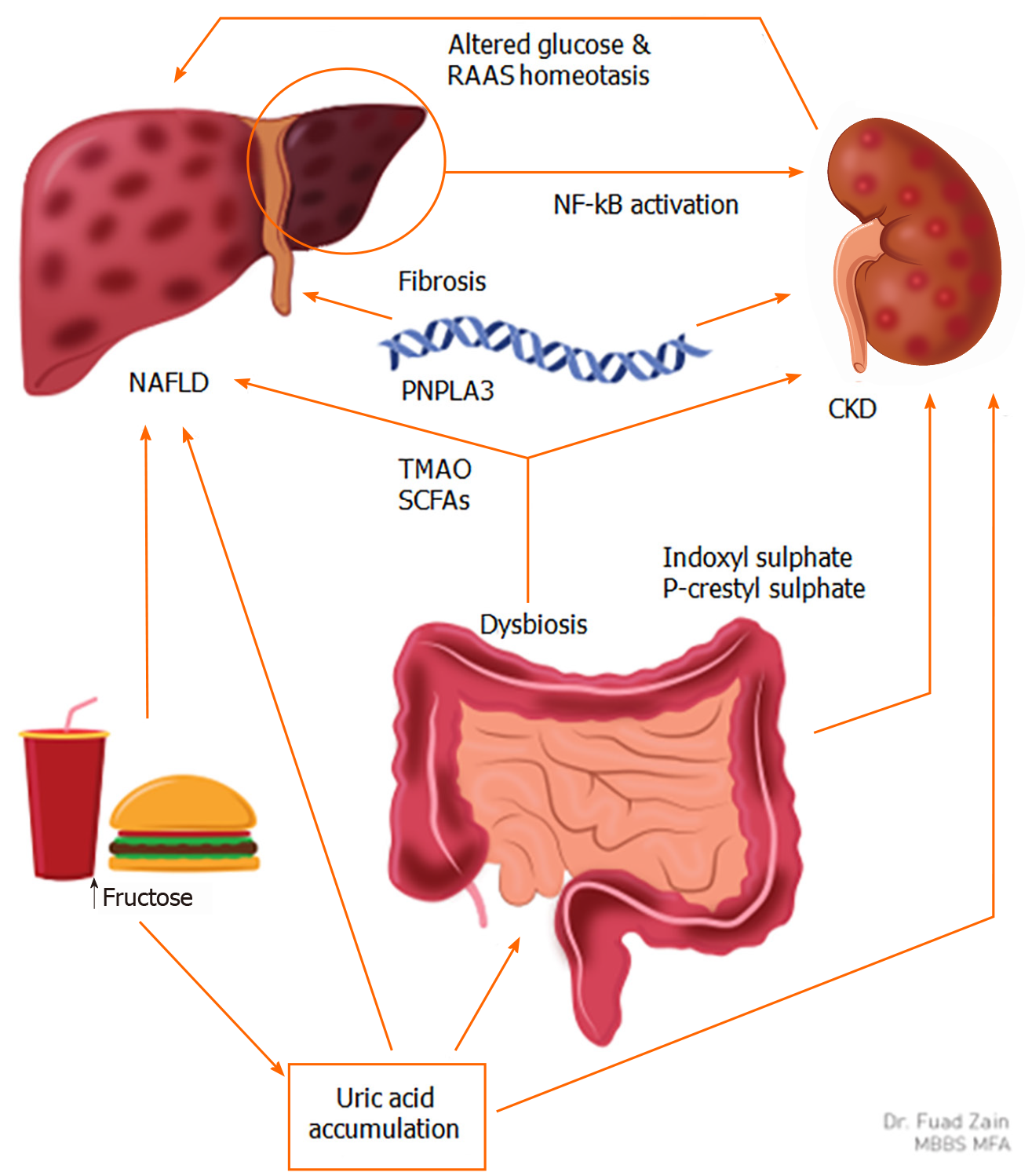
Figure 2 Fructose consumption and uric acid accumulation play a key role in patients with non-alcoholic fatty liver disease who develop chronic kidney disease.
TMAO: Trimethylamine N-oxide; SCFAs: Short-chain fatty acids; RAAS: Renin-angiotensin-aldosterone system; PNPLA3: Patatin-like phospholipase domain-containing protein 3; NAFLD: Non-alcoholic fatty liver disease; CKD: Chronic kidney disease; NF-κB: Nuclear factor-κB.
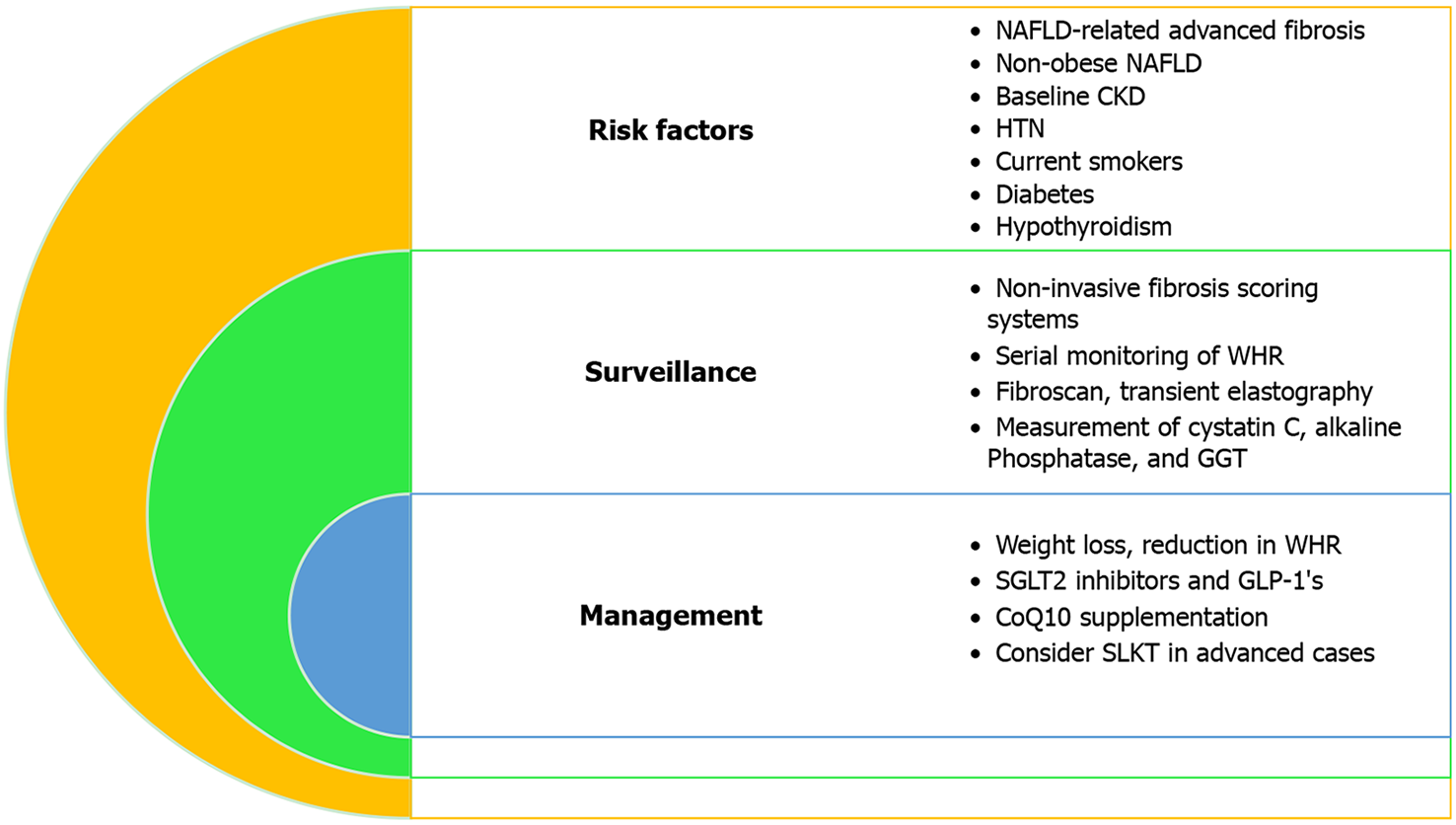
Figure 3 Identifying and managing non-alcoholic fatty liver disease patients who are at risk for developing chronic kidney disease.
NAFLD: Non-alcoholic fatty liver disease; CKD: Chronic kidney disease; HTN: Hypertension; WHR: Waist-to-Hip ratio; GGT: Gamma-glutamyl transferase; T2DM: Type 2 diabetes mellitus; SLKT: Simultaneous liver-kidney transplantation; SGLT2: Sodium-glucose cotransporter type-2; GLP-1: Glucagon-like peptide 1.
- Citation: Heda R, Yazawa M, Shi M, Bhaskaran M, Aloor FZ, Thuluvath PJ, Satapathy SK. Non-alcoholic fatty liver and chronic kidney disease: Retrospect, introspect, and prospect. World J Gastroenterol 2021; 27(17): 1864-1882
- URL: https://www.wjgnet.com/1007-9327/full/v27/i17/1864.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i17.1864