Copyright
©The Author(s) 2020.
World J Gastroenterol. Nov 7, 2020; 26(41): 6391-6401
Published online Nov 7, 2020. doi: 10.3748/wjg.v26.i41.6391
Published online Nov 7, 2020. doi: 10.3748/wjg.v26.i41.6391
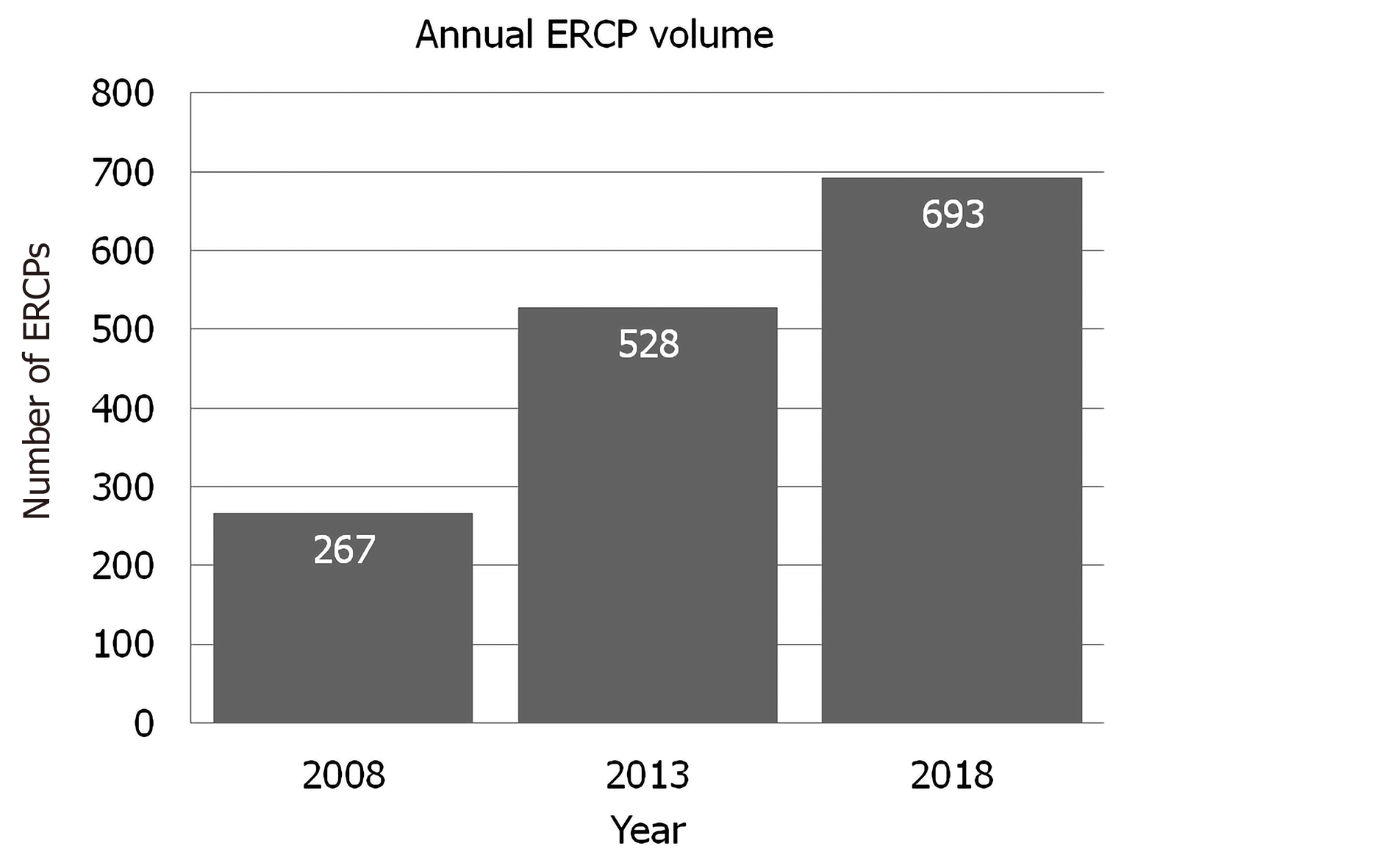
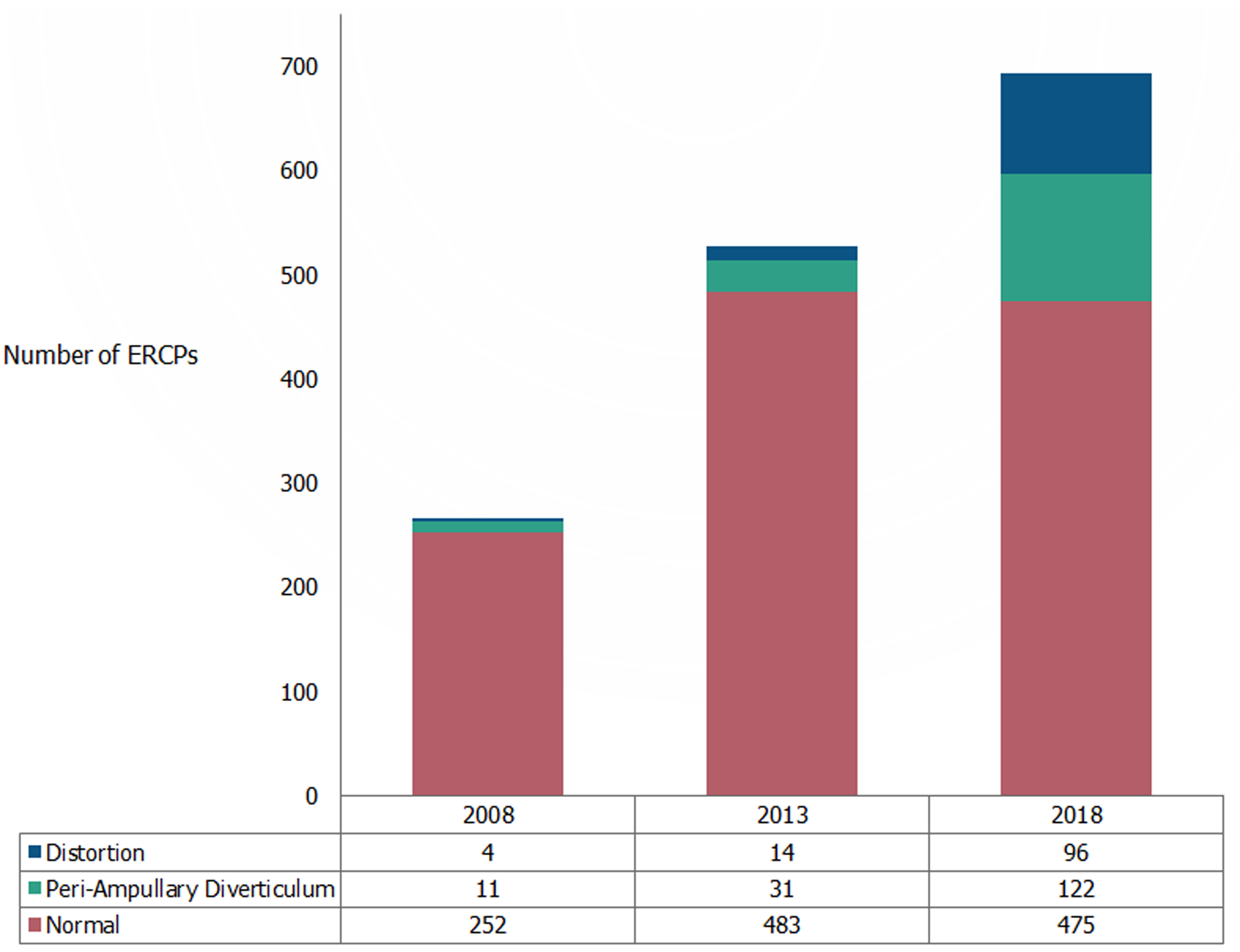
Figure 1 Annual endoscopic retrograde cholangiopancreatography volume progressively increased from 2008 to 2018.
ERCP: Endoscopic retrograde cholangiopancreatography.
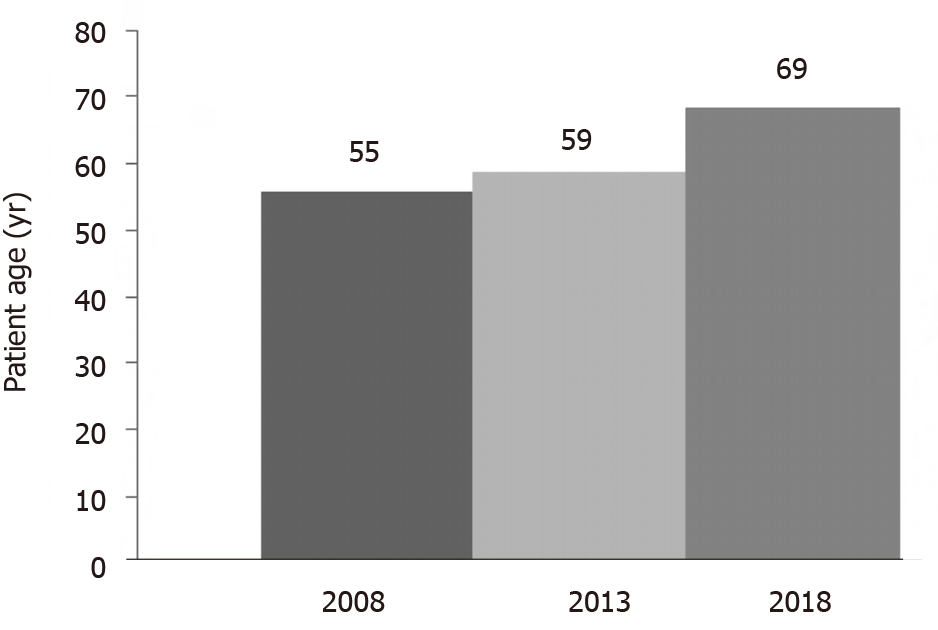
Figure 2 Mean age of patients progressively increased significantly from 2008 to 2018.
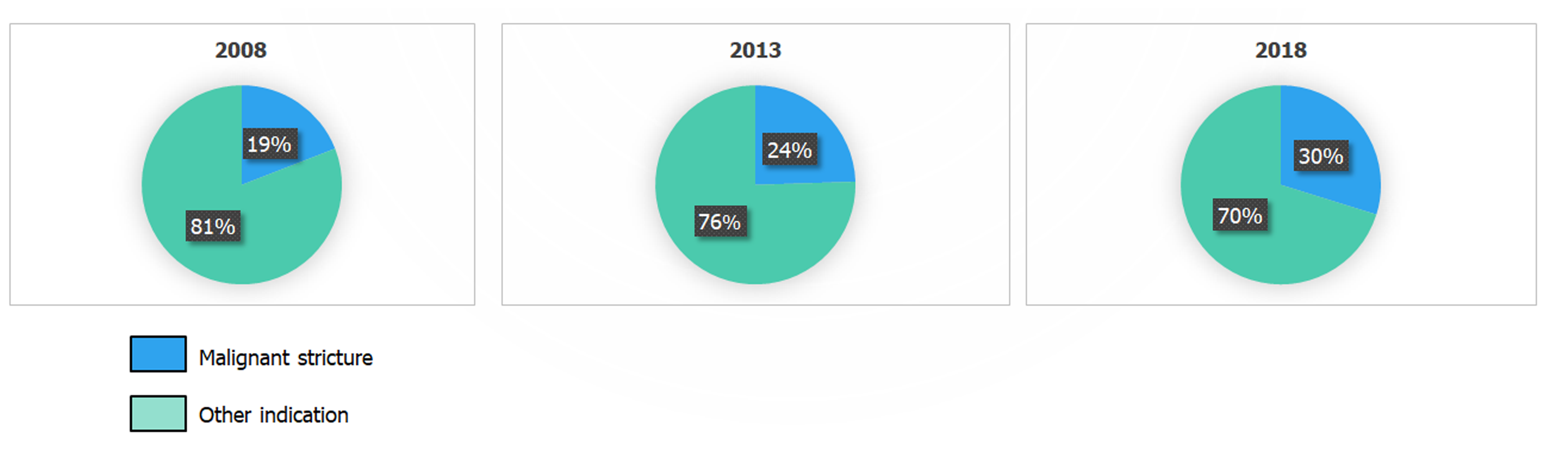
Figure 3 Proportion of endoscopic retrograde cholangiopancreatography performed for management of malignant biliary strictures increased from 2008 to 2018, but this did not reach statistical significance.
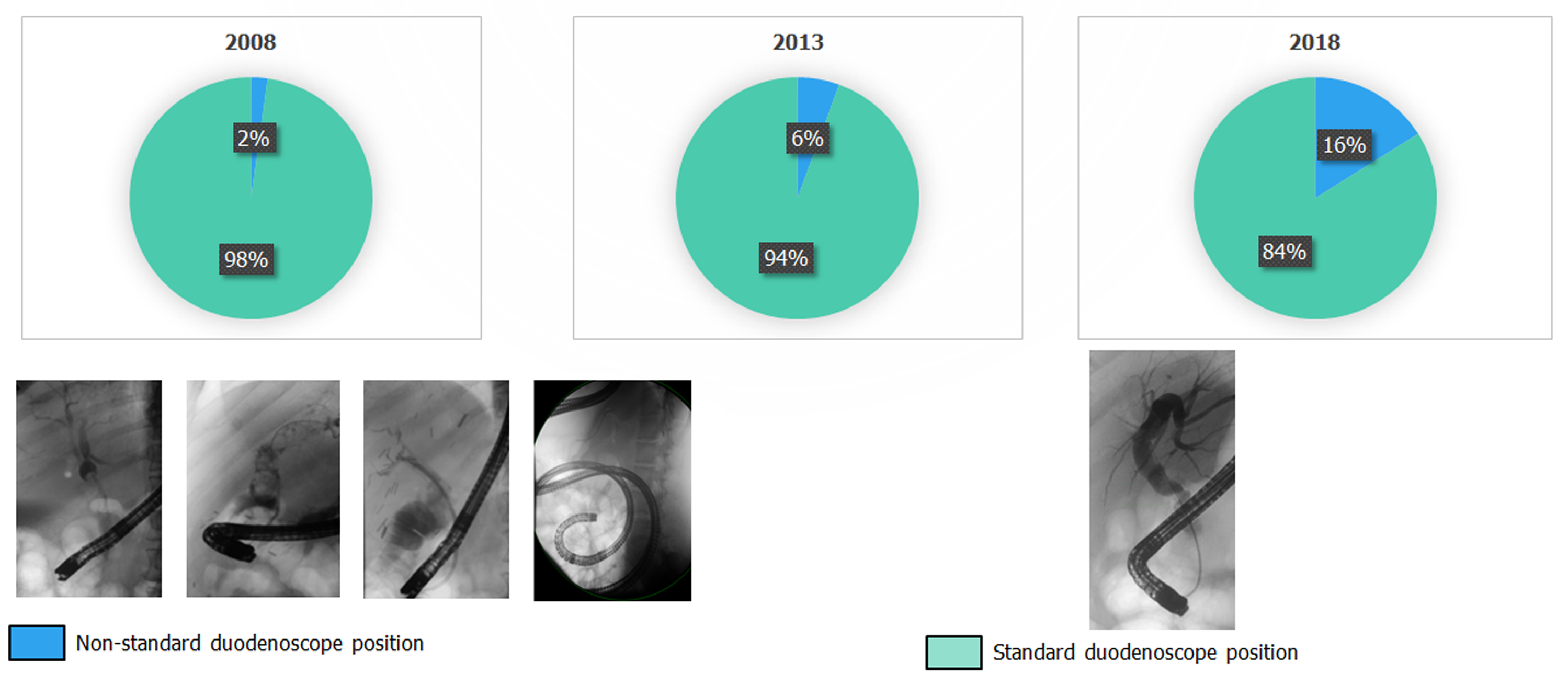
Figure 4 Proportion of endoscopic retrograde cholangiopancreatography performed with the duodenoscope in a non-standard position increased significantly from 2008 to 2018.
Figure 5 Progressive increase in the frequency of ampullary distortion/tumor infiltration, duodenal distortion/stenosis and peri-ampullary diverticula was noted in over the study period.
ERCP: Endoscopic retrograde cholangiopancreatography.
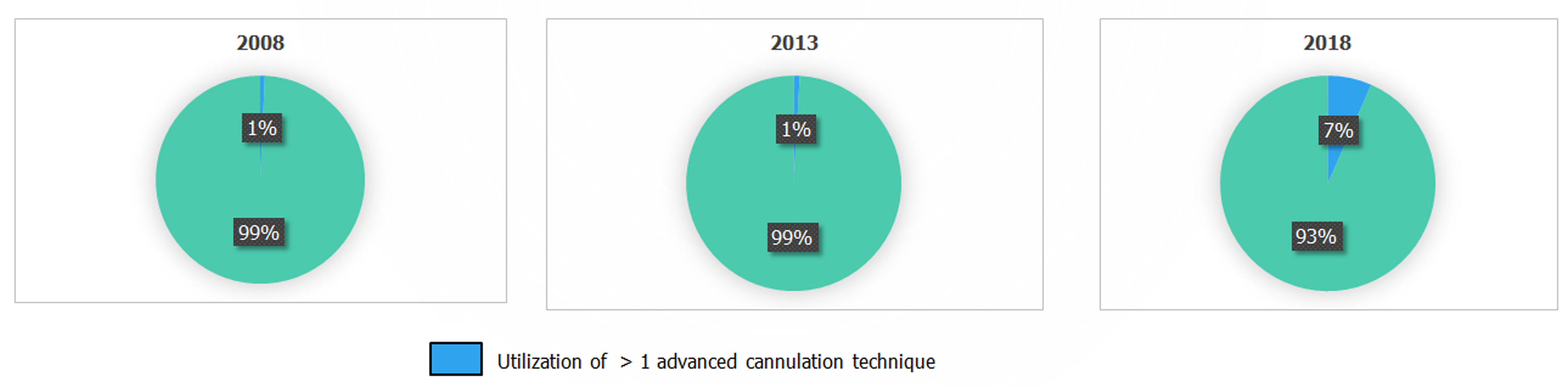
Figure 6 Utilization of more than one advanced cannulation technique for a given endoscopic retrograde cholangiopancreatography increased significantly over the study period.
Figure 7 Over the study period, there was an increasing proportion of procedures with oropharyngeal, esophageal, gastric and duodenal barriers to duodenoscope advancement and cannulation.
A: Qropharyngeal barriers to duodenoscope advancement and cannulation; B: Esophageal barriers to duodenoscope advancement and cannulation; C: Gastric barriers to duodenoscope advancement and cannulation; D: Duodenal barriers to duodenoscope advancement and cannulation.
- Citation: Barakat MT, Girotra M, Thosani N, Kothari S, Banerjee S. Escalating complexity of endoscopic retrograde cholangiopancreatography over the last decade with increasing reliance on advanced cannulation techniques. World J Gastroenterol 2020; 26(41): 6391-6401
- URL: https://www.wjgnet.com/1007-9327/full/v26/i41/6391.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i41.6391