Copyright
©The Author(s) 2020.
World J Gastroenterol. Aug 21, 2020; 26(31): 4703-4717
Published online Aug 21, 2020. doi: 10.3748/wjg.v26.i31.4703
Published online Aug 21, 2020. doi: 10.3748/wjg.v26.i31.4703
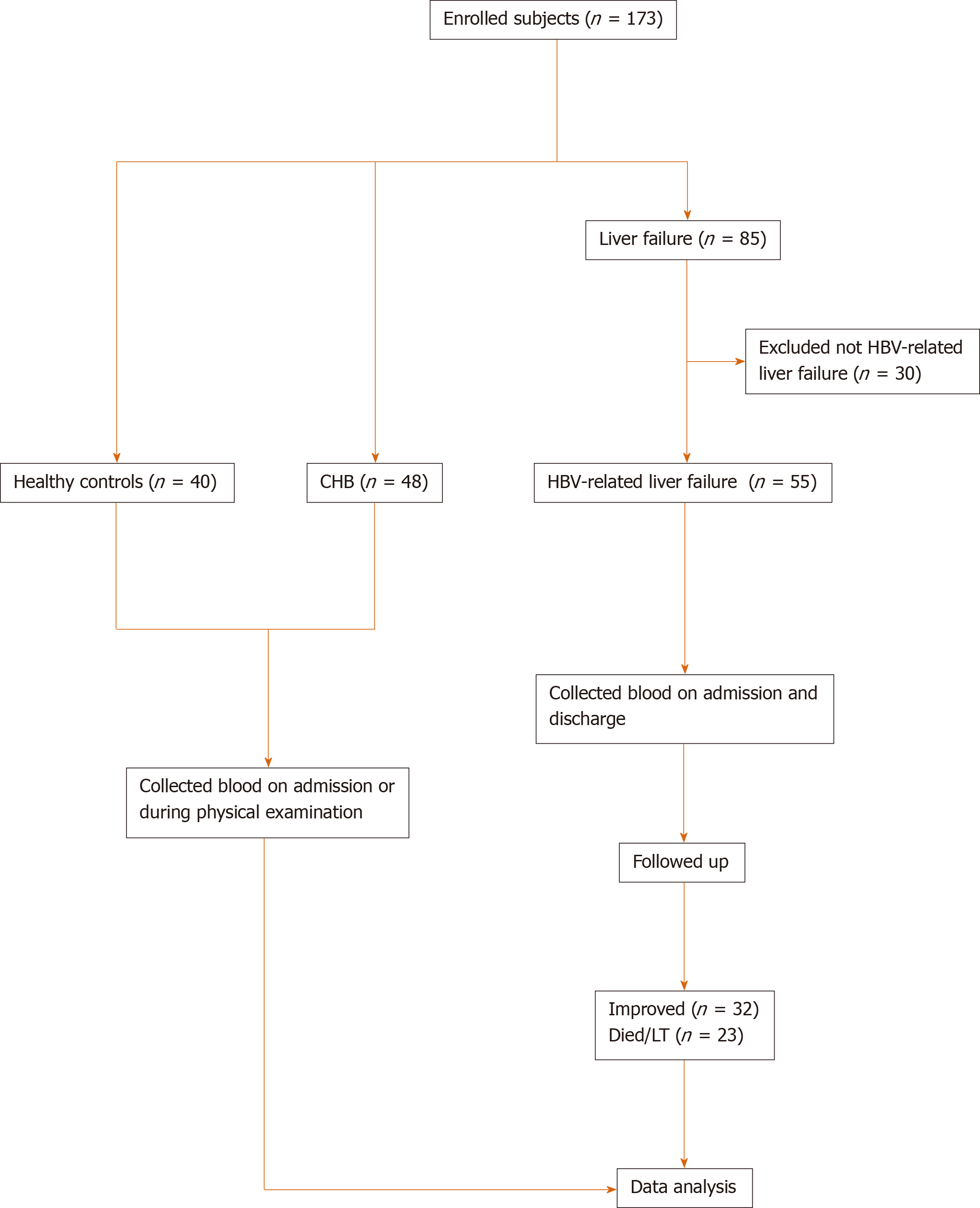
Figure 1 Flow chart for patient enrollment and analysis.
Diagram showing the general process from enrolling patients to the final analysis. CHB: Chronic hepatitis B; HBV: Hepatitis B virus.
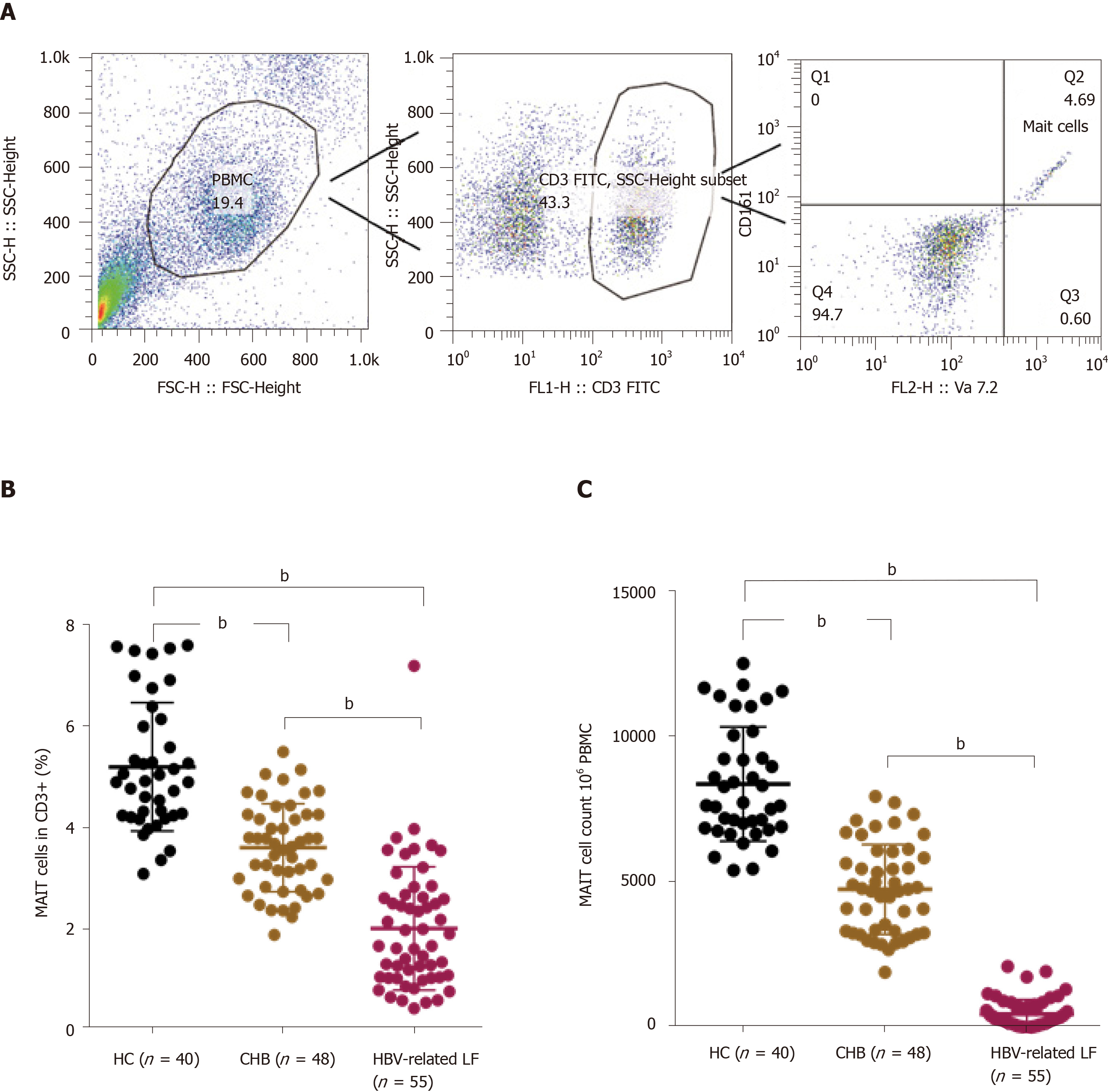
Figure 2 Circulating mucosal-associated invariant T cells were dramatically decreased in hepatitis B virus-related liver failure.
A: The strategy for flow cytometry of mucosal-associated invariant T (MAIT) cells; B: The percentage of circulating MAIT cells in healthy controls (HC, n = 40), chronic hepatitis B (CHB, n = 48) patients and hepatitis B virus (HBV)-related liver failure (LF) patients (n = 55); C: Circulating MAIT cell count in 106 peripheral blood mononuclear cells in HCs and CHB and HBV-related liver failure patients. bP < 0.0001.
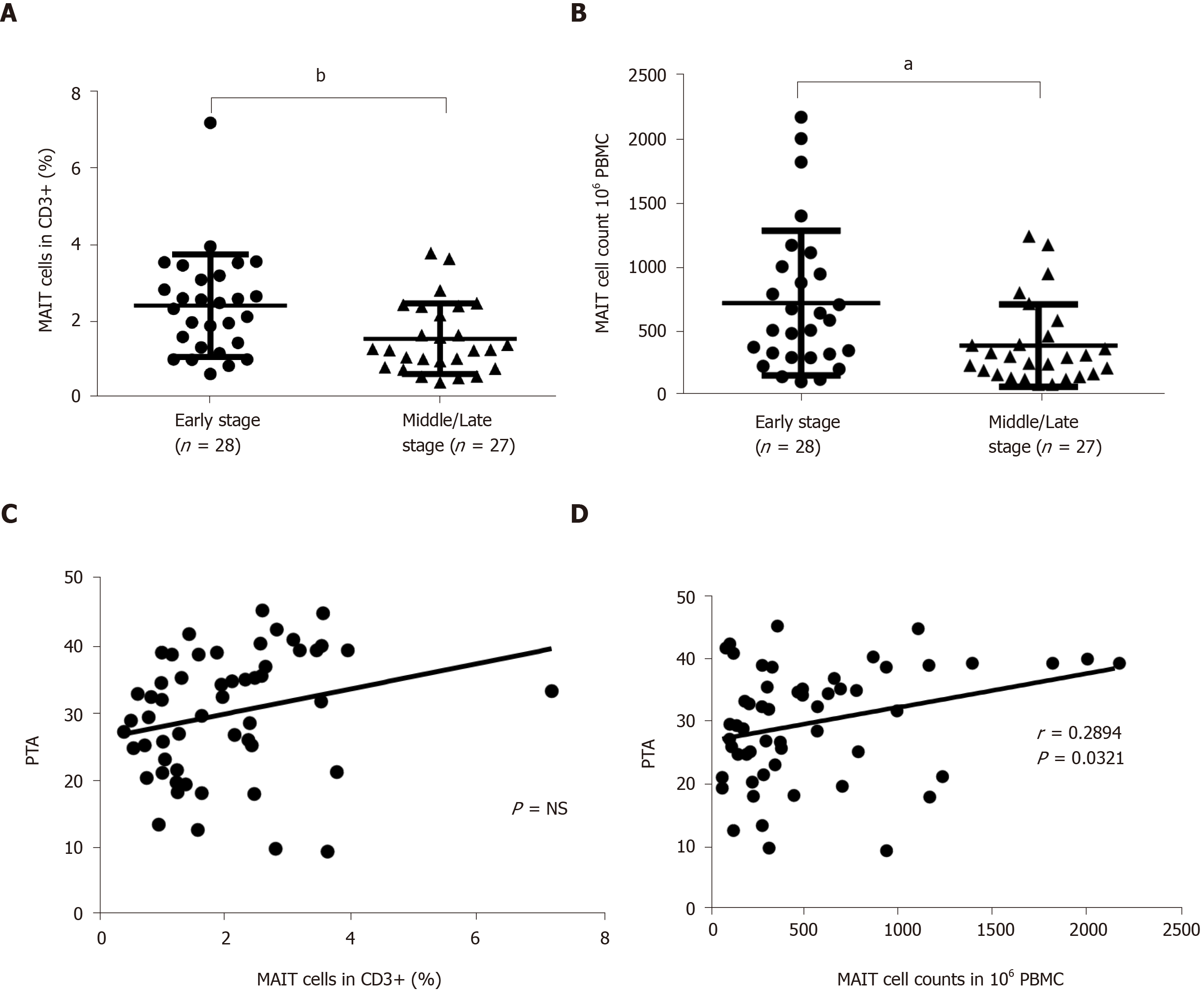
Figure 3 Quantity of circulating mucosal-associated invariant T cells was associated with severity of hepatitis B virus-related liver failure.
A, B: The percentage (A) and number (B) of circulating mucosal-associated invariant T (MAIT) cells in early- (n = 28) and middle/late-stage (n = 27) hepatitis B virus (HBV)-related liver failure; C, D: Correlation between prothrombin activity (PTA) and percentage (C) or number (D) of circulating MAIT cells in patients with HBV-related liver failure. aP < 0.05, bP < 0.01. PBMC: Peripheral blood mononuclear cell. NS: No significance.
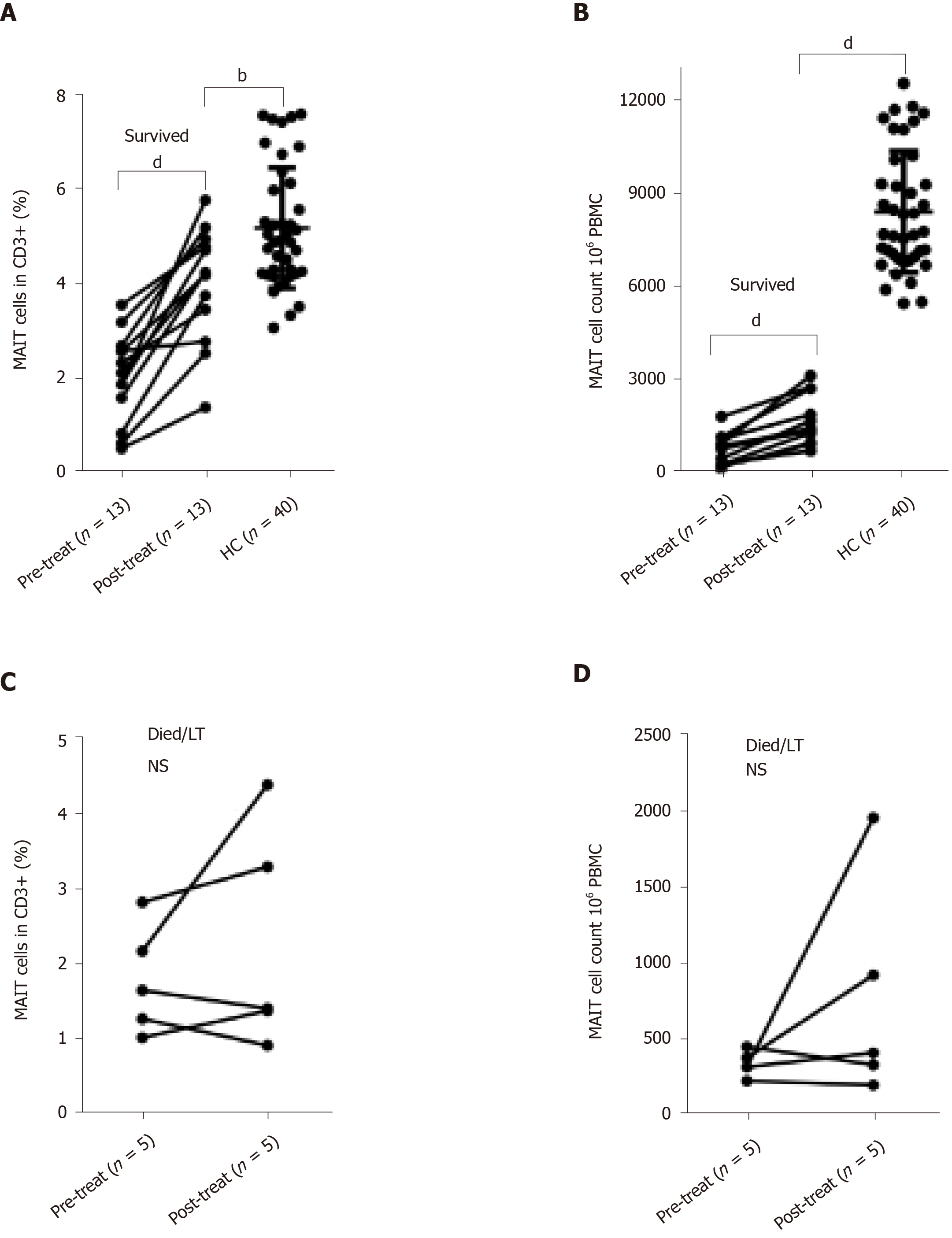
Figure 4 Partial recovery of circulating mucosal-associated invariant T cells in survived hepatitis B virus-related liver failure patients.
A, B: The percentage (A) and count (B) of circulating mucosal-associated invariant T (MAIT) cells before and after treatment of surviving patients (n = 13) with hepatitis B virus (HBV)-related liver failure, and in healthy controls (HC) (n = 40); C, D: The percentage (C) and number (D) of MAIT cells in patients (n = 5) who died or underwent liver transplantation in HBV-related liver failure before and after conservative treatment. bP < 0.01, dP < 0.0001. NS: No significance; PBMC: Peripheral blood mononuclear cell.
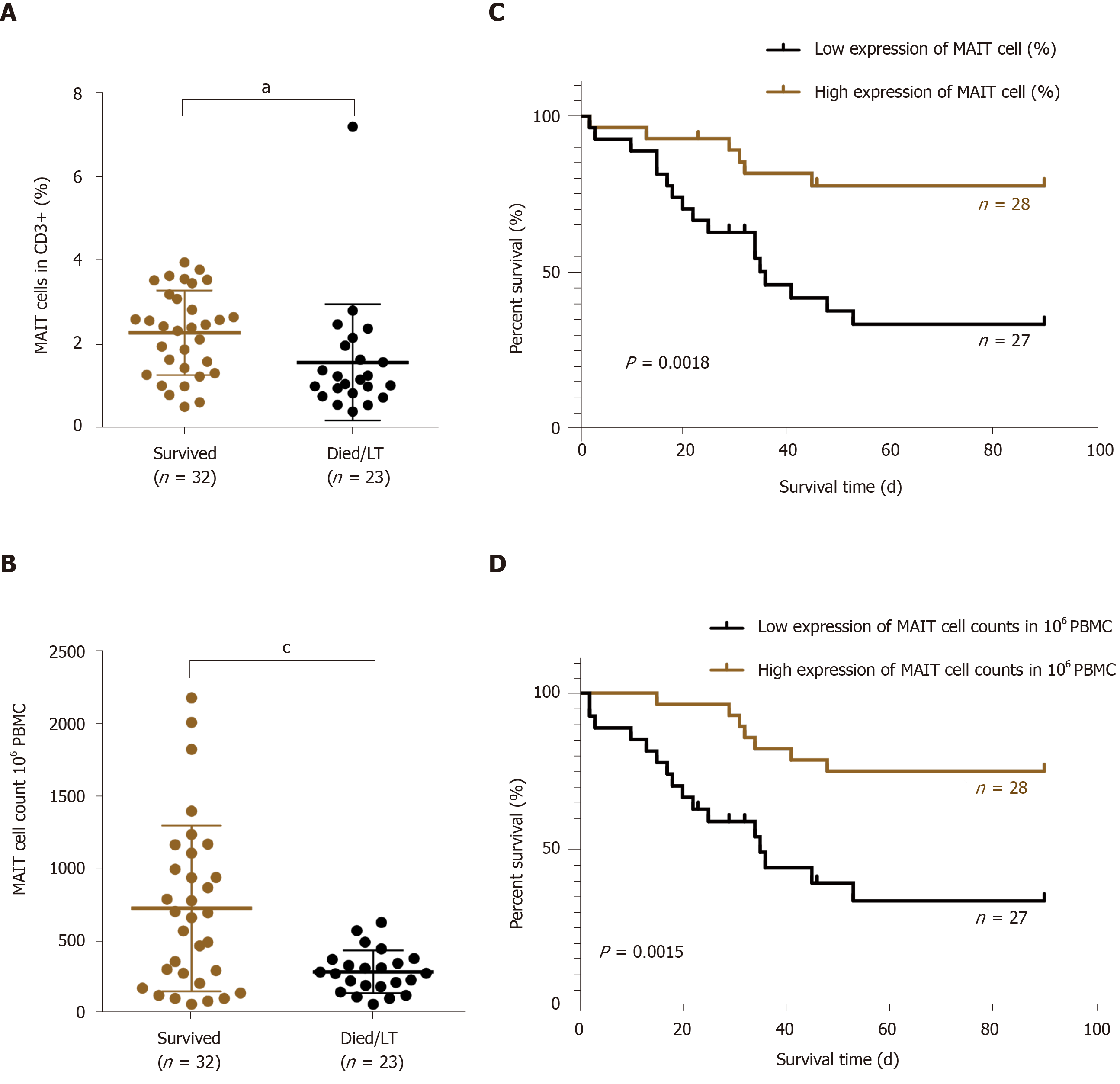
Figure 5 Lower count of circulating mucosal-associated invariant T cells indicated poor prognosis in hepatitis B virus-related liver failure.
A, B: The proportion (A) and number (B) of circulating mucosal-associated invariant T (MAIT) cells in surviving (n = 32) and deceased/liver transplanted (LT) (n = 23) patients with hepatitis B virus (HBV)-related liver failure; C, D: The Kaplan–Meier curve of HBV-related liver failure patients with low (n = 27) and high (n = 28) expression of MAIT cells in percentage (C) and count (D). aP < 0.05, cP < 0.001. PBMC: Peripheral blood mononuclear cell.
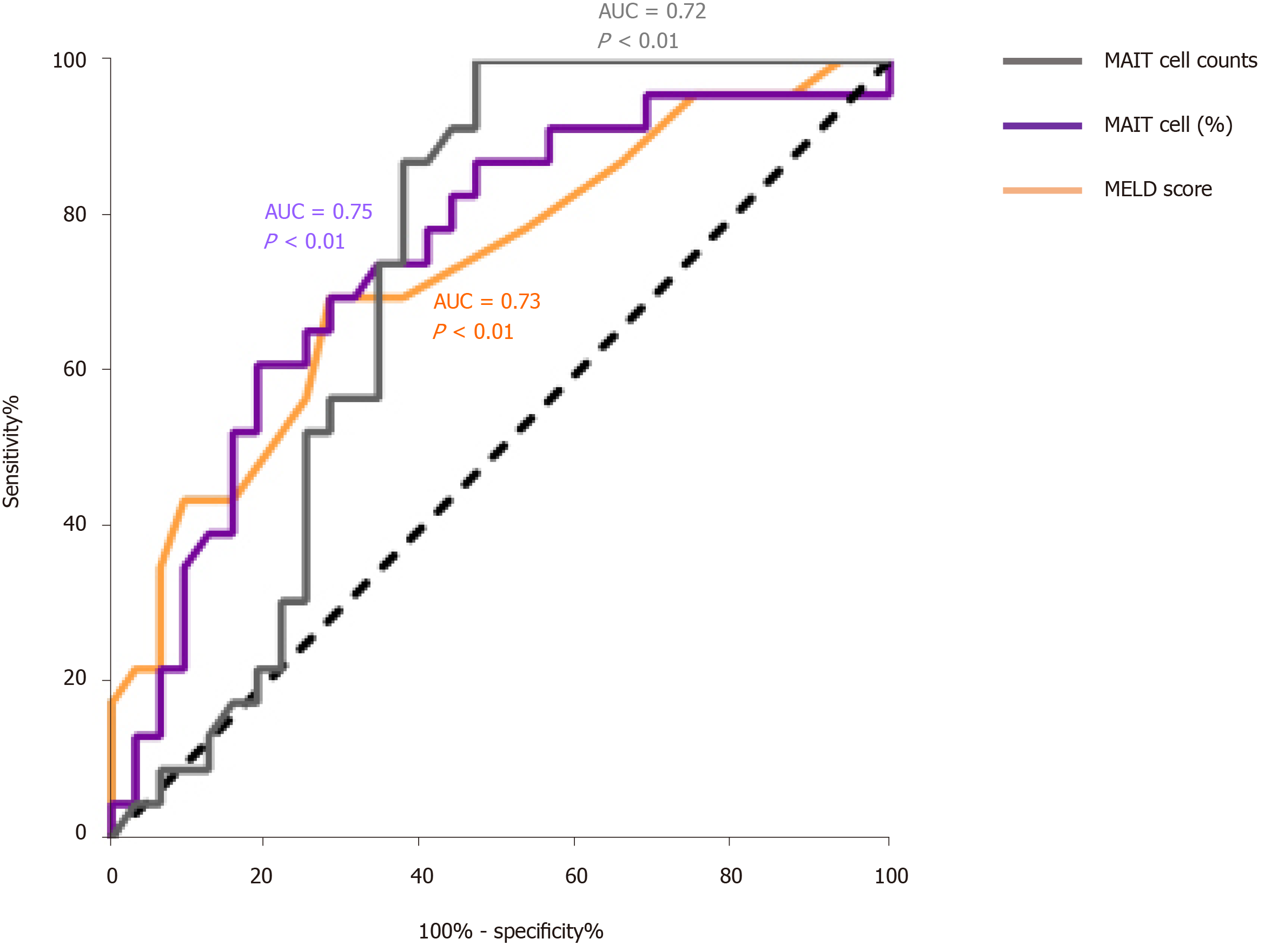
Figure 6 The prognostic value of model for end-stage liver disease score, mucosal-associated invariant T cell counts and percentage of mucosal-associated invariant T cells in patients with hepatitis B virus-related liver failure.
The receiver characteristic operator curve of model for end-stage liver disease (MELD) score and mucosal-associated invariant T (MALT) cells counts and percentage (%). AUC: Area under the curve.
Figure 7 Plasma levels of interleukin-12 and interleukin-18 were increased in patients with hepatitis B virus-related liver failure.
A-D: Plasma level of interleukin (IL)-12p70 (A), IL-18 (B), IL-7 (C) and interferon-α (D) in healthy controls (HC) (n = 40) and patients with hepatitis B virus (HBV)-related liver failure (n = 46). aP < 0.05; dP < 0.0001. NS: No significance.
- Citation: Xue H, Li H, Ju LL, Han XD, Cheng TC, Luo X, Chen L, Shao JG, She YJ, Bian ZL. Mucosal-associated invariant T cells in hepatitis B virus-related liver failure. World J Gastroenterol 2020; 26(31): 4703-4717
- URL: https://www.wjgnet.com/1007-9327/full/v26/i31/4703.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i31.4703