Copyright
©The Author(s) 2019.
World J Gastroenterol. Aug 21, 2019; 25(31): 4343-4359
Published online Aug 21, 2019. doi: 10.3748/wjg.v25.i31.4343
Published online Aug 21, 2019. doi: 10.3748/wjg.v25.i31.4343
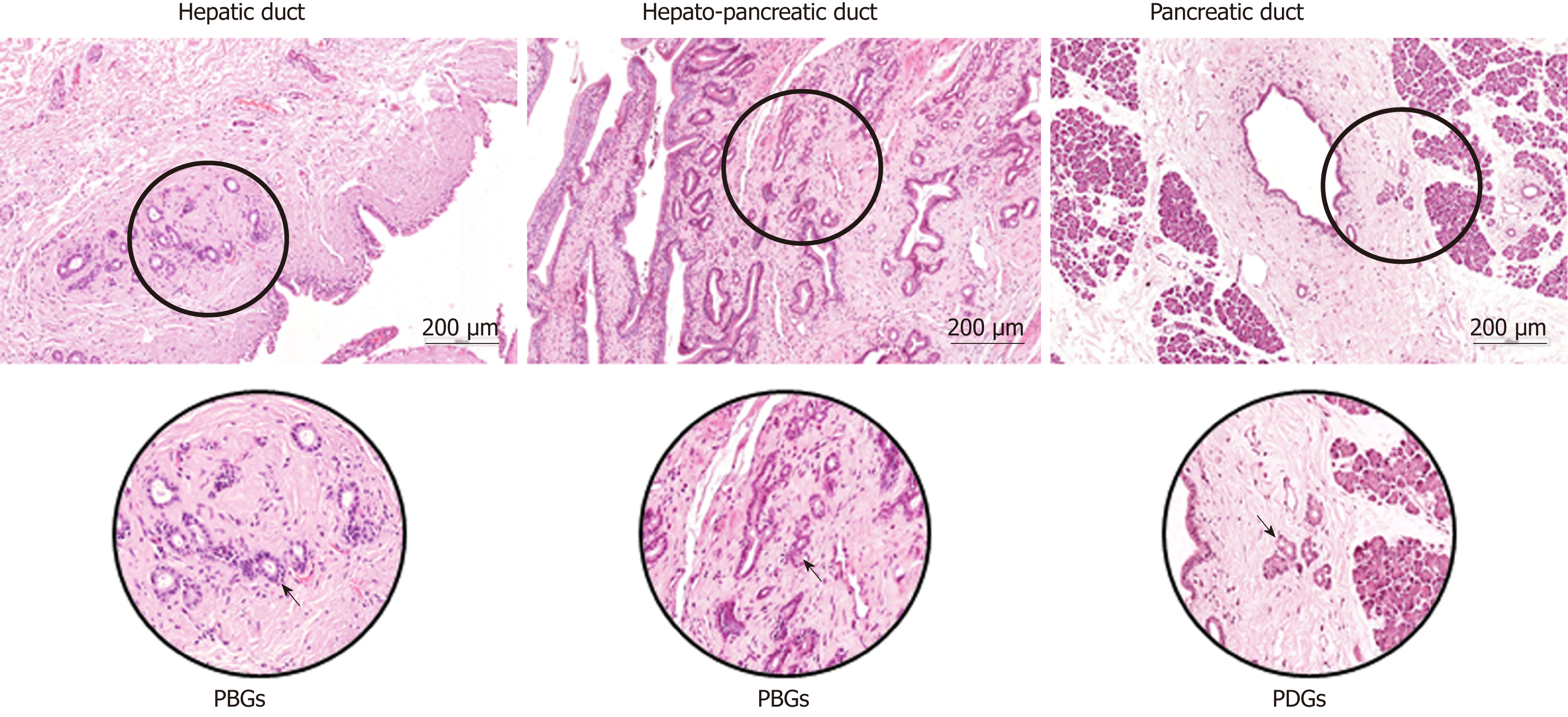
Figure 1 Common and Distinctive Features of peribiliary and pancreatic ductal glands.
The peribiliary glands are tubule-alveolar glands present within the walls of larger biliary ducts, more commonly located at branching points of the biliary tree, in particular at the hepatopancreatic region. The pancreatic ductal glands containing pancreatic committed progenitors are observed within the walls of larger pancreatic ducts. PBGs: Peribiliary glands; PDGs: Pancreatic ductal glands.
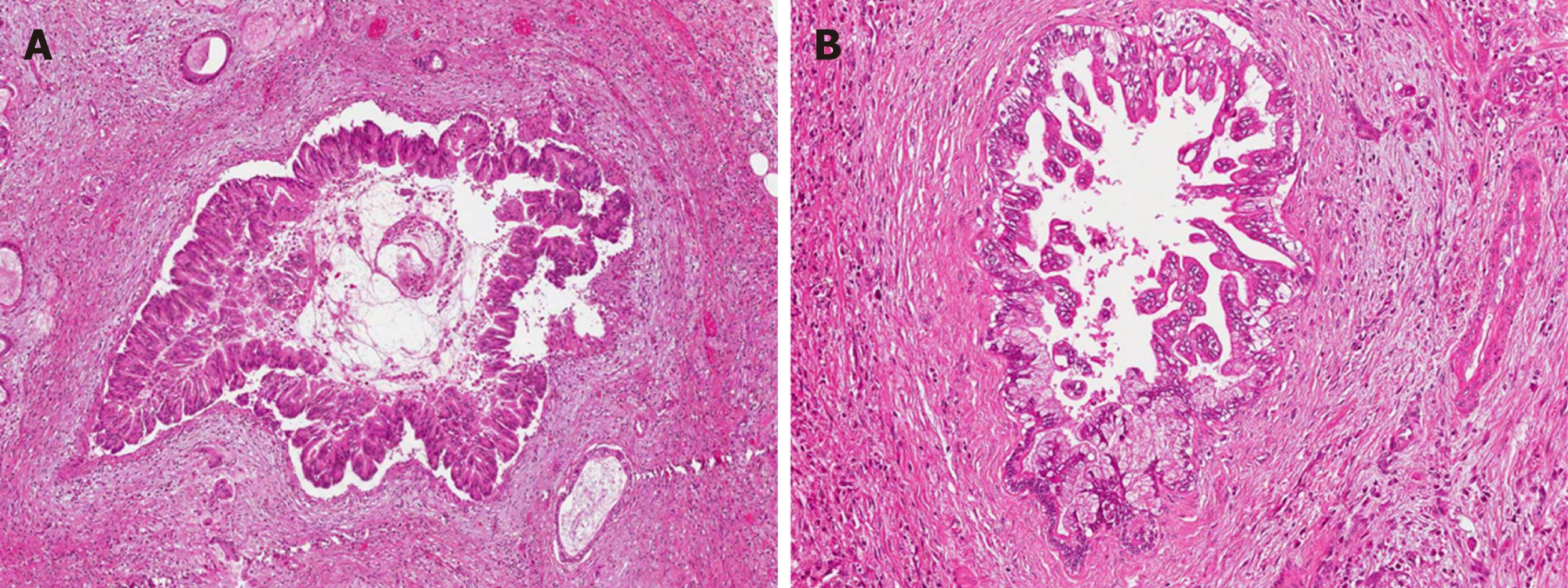
Figure 2 Common and distinctive features of pancreatic intraepithelial neoplasias and biliary intraepithelial neoplasms.
A: Pancreatic intraepithelial neoplasia, high grade (PanIN-3, 10 ×) sorrounded by infiltrating adenocarcinoma. B: Biliary intraepithelial neoplasia, high grade (BilIN-3, 10 ×) with nearby infiltrating adenocarcinoma Both lesions are microscopic precancerous lesions of pancreas (A) and biliary tree (B), not identifiable by radiological imaging.
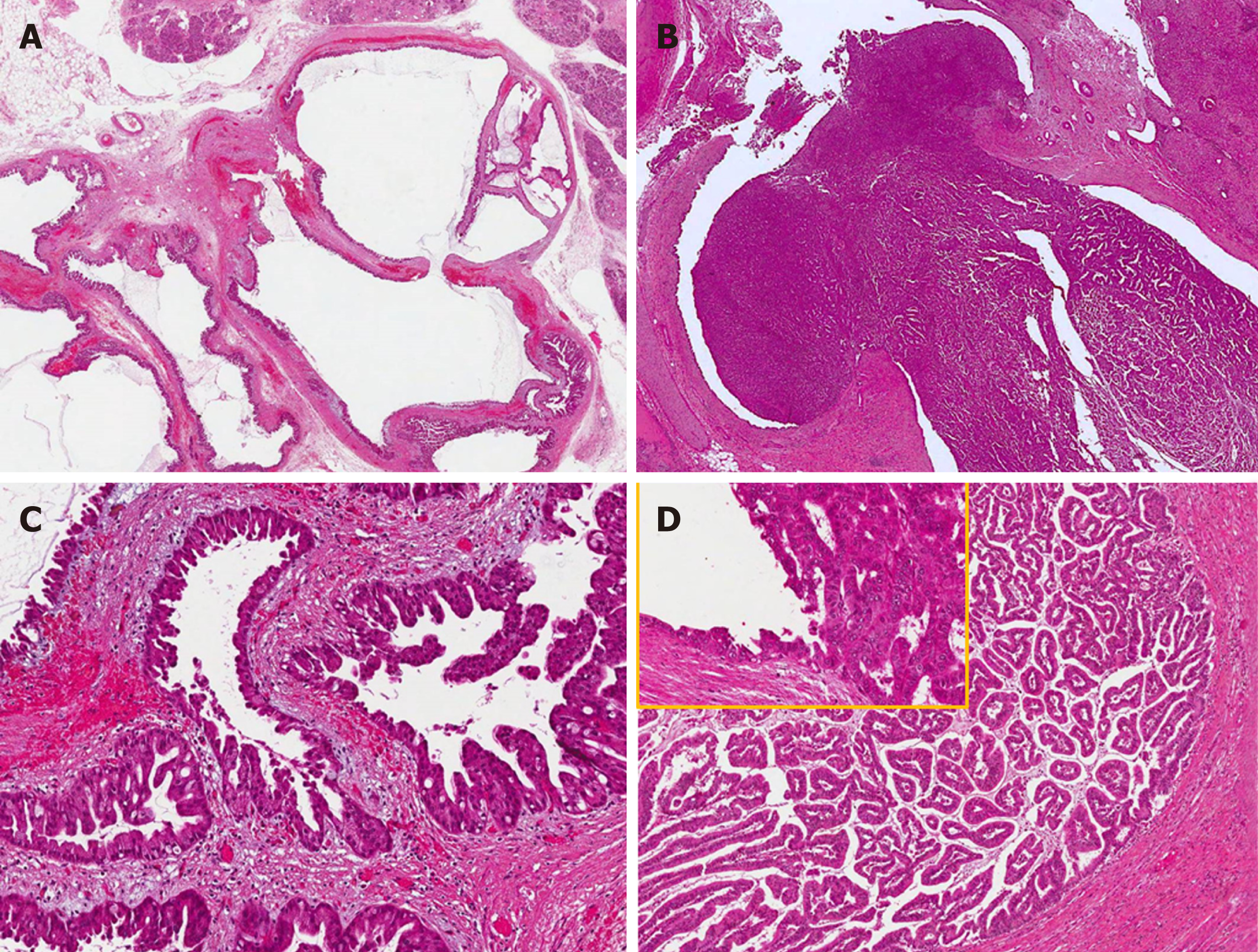
Figure 3 Common and distinctive features of pancreatic and biliary intraductal papillary mucinous neoplasms.
Low power view of intraductal papillary mucinous neoplasm of the pancreas (A) with oncocytic aspects (B), causing evident dilatation of the Wirsung duct which was detected radiologically as a macroscopic lesion. Low power view of intraductal papillary neoplasm of the bile duct (C) characterized by a polypoid growth inside the common hepatic duct, composed of multiple papillary projections with a fibrovascular stroma and covered by oncocytic cells (D). In the upper left part of panel D at higher magnification, the transition between the normal bile duct epithelium and the papillary neoplastic proliferation is evident.
- Citation: Zaccari P, Cardinale V, Severi C, Pedica F, Carpino G, Gaudio E, Doglioni C, Petrone MC, Alvaro D, Arcidiacono PG, Capurso G. Common features between neoplastic and preneoplastic lesions of the biliary tract and the pancreas. World J Gastroenterol 2019; 25(31): 4343-4359
- URL: https://www.wjgnet.com/1007-9327/full/v25/i31/4343.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i31.4343