Copyright
©The Author(s) 2019.
World J Gastroenterol. Jun 7, 2019; 25(21): 2636-2649
Published online Jun 7, 2019. doi: 10.3748/wjg.v25.i21.2636
Published online Jun 7, 2019. doi: 10.3748/wjg.v25.i21.2636
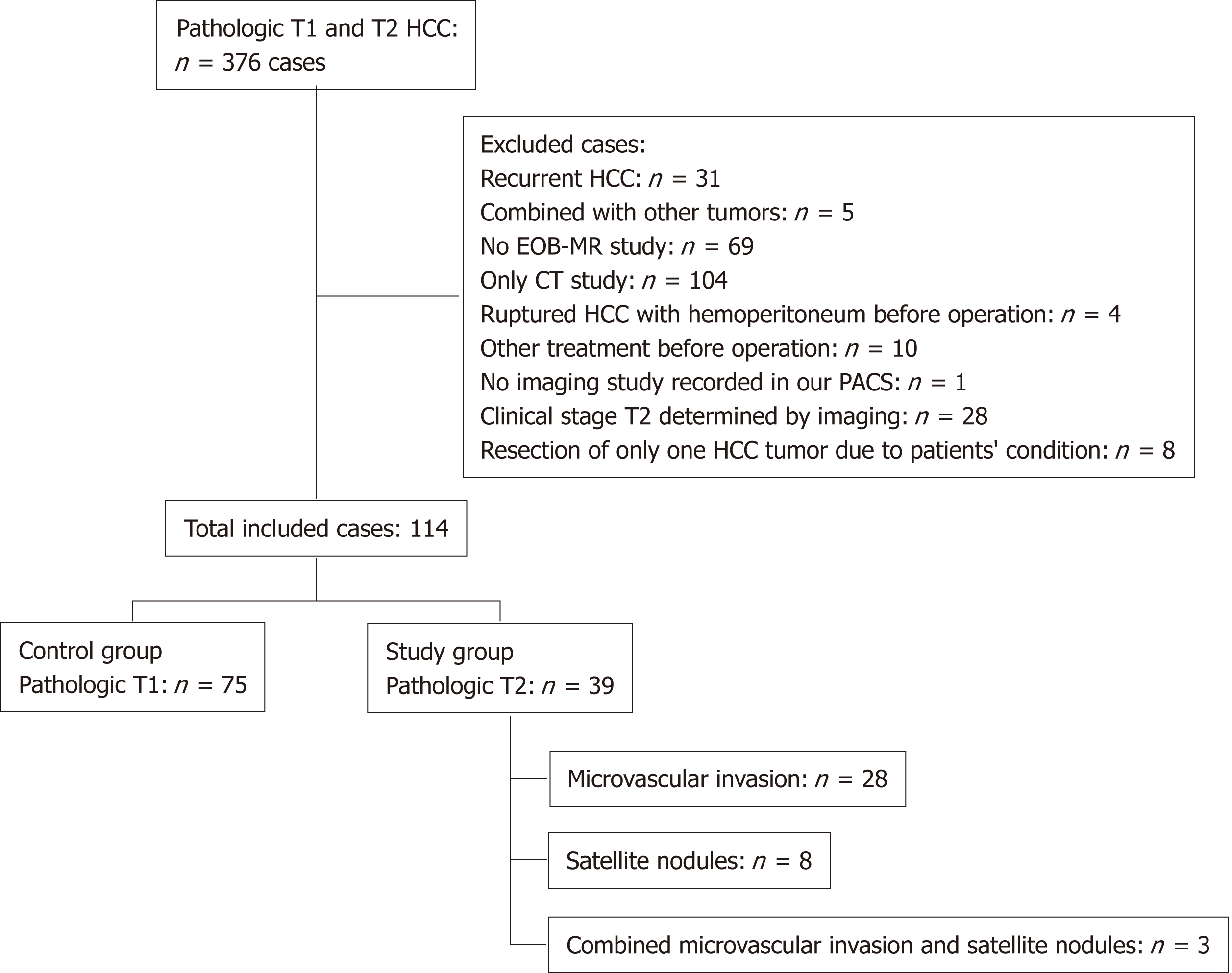
Figure 1 Flow chart of the study population selection process and the inclusion and exclusion criteria.
HCC: Hepatocellular carcinoma; EOB-MRI: ethoxybenzyl magnetic resonance imaging; CT: Computed tomography.
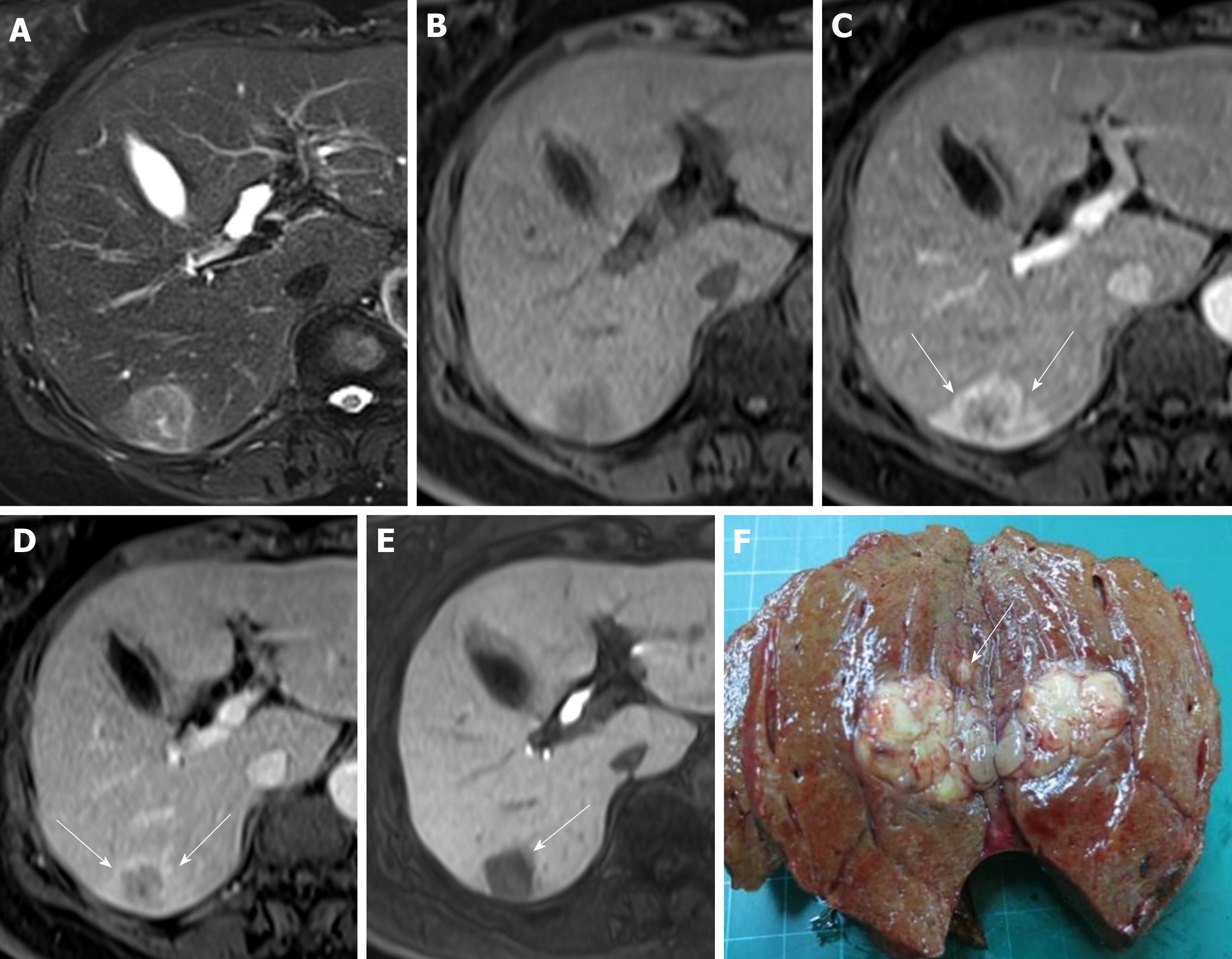
Figure 2 Images in a 73-year-old woman with a solitary hepatocellular carcinoma (tumor size 2.
6 cm) in segment VI. A and B: Axial view of T2- and T1-weighted magnetic resonance images with fat suppression before administration of gadolinium ethoxybenzyl diethylene-triaminepentaacetic acid; C: Arterial phase and D: Portal venous phase showing hyperenhancing mass in segment VI with washout appearance, which is the typical appearance of hepatocellular carcinoma, as well as corona enhancement (arrow); E: Hepatobiliary phase, axial view of T1-weighted three-dimensional gradient-echo magnetic resonance image with fat suppression. The faint low signal intensity around the tumor is the peritumoral hypointensity (arrow); F: The tumor is identifiable postoperatively as a pT2 hepatocellular carcinoma because a satellite nodule surrounds the main tumor.
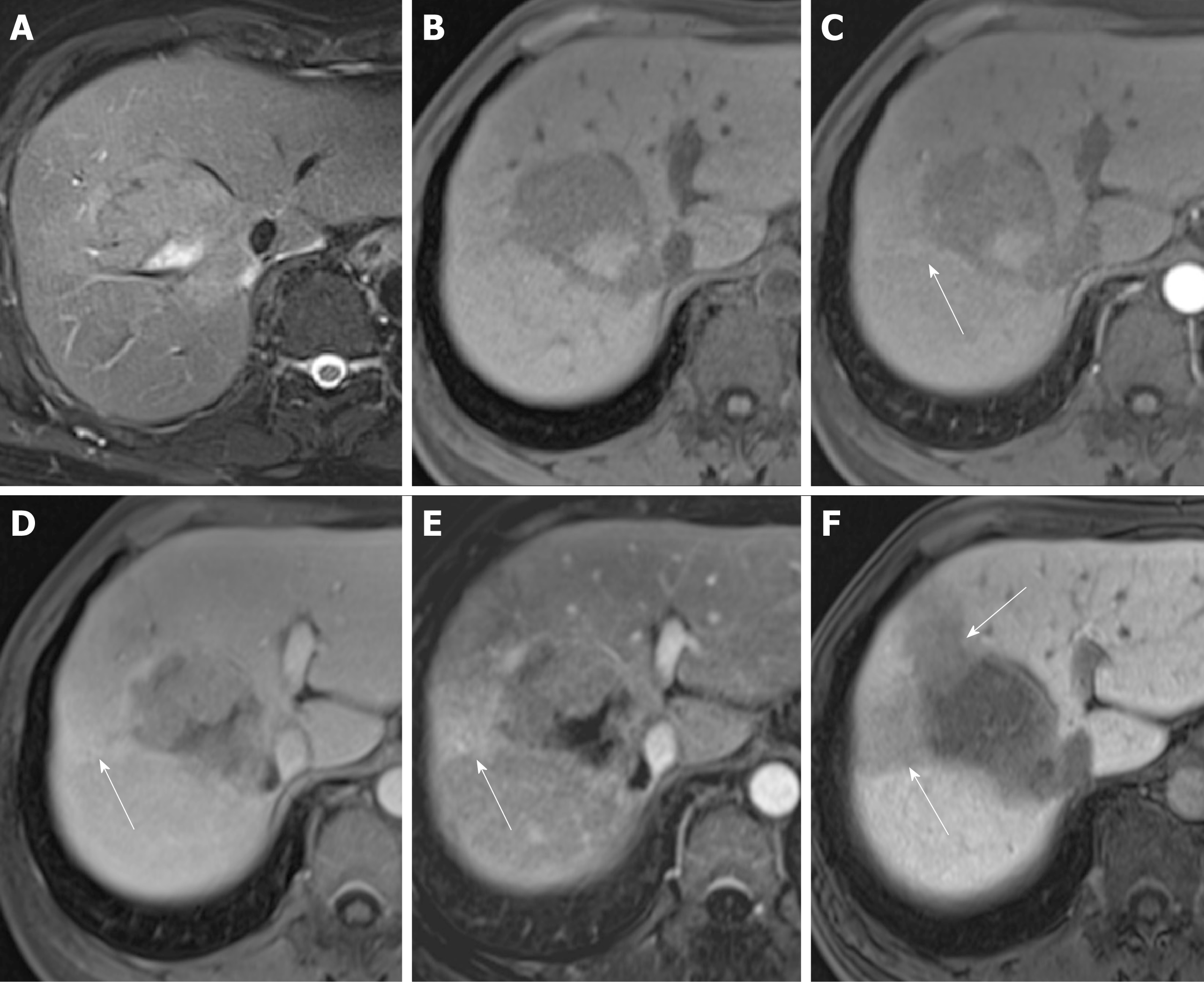
Figure 3 Images in a 64-year-old man with a solitary hepatocellular carcinoma (tumor size 5.
5 cm) in segment VIII. A and B: Axial view of T2- and T1-weighted magnetic resonance images with fat suppression before administration of gadolinium ethoxybenzyl diethylene-triaminepentaacetic acid; C: Arterial phase and D: Portal venous phase showing hyperenhancing mass in segment VIII with partial washout appearance and corona enhancement (arrow); E: Subtracted images of the portal venous phase with more obvious corona enhancement; F: Hepatobiliary phase, T1-weighted three-dimensional gradient-echo magnetic resonance image (axial view) with fat suppression. The obvious flame-like peritumoral hypointensity (arrow) is noted. This tumor was identified postoperatively as a pT2 hepatocellular carcinoma owing to its microvascular invasion.
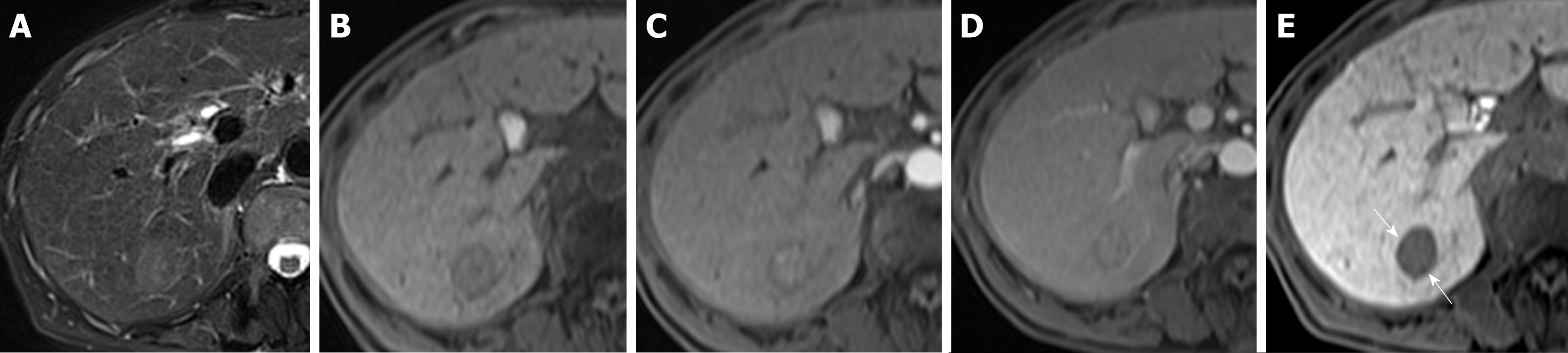
Figure 4 Images in a 65-year-old woman with a solitary hepatocellular carcinoma (tumor size 2.
1 cm) in segment VII. A and B: Axial view of T2- and T1-weighted magnetic resonance images with fat suppression before administration of gadolinium ethoxybenzyl diethylene-triaminepentaacetic acid; C: Arterial phase showing hyperenhancing mass in segment VII; D: Portal venous phase with notable washout appearance of the hepatocellular carcinoma; E: Hepatobiliary phase, axial view of T1-weighted three-dimensional gradient-echo magnetic resonance image with fat suppression. The hypointense rim (arrow) is noted. Postoperatively, pT1 hepatocellular carcinoma was diagnosed.
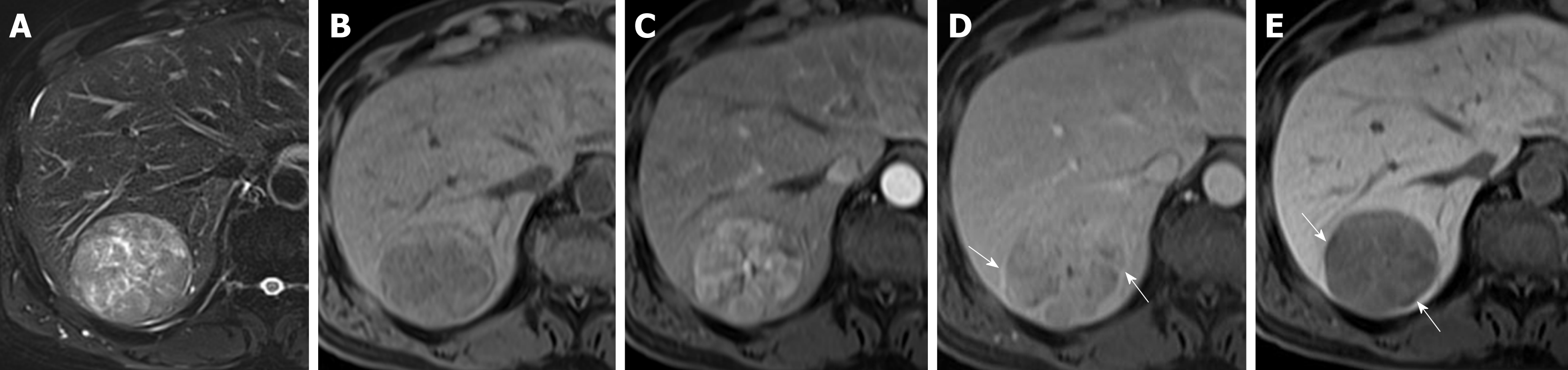
Figure 5 Images in a 60-year-old man with a solitary hepatocellular carcinoma (tumor size 5.
5 cm) in segment VII. A and B: Axial view of T2- and T1-weighted magnetic resonance images with fat suppression before administration of gadolinium ethoxybenzyl diethylene-triaminepentaacetic acid; C: Arterial phase. Note the hyperenhancing hepatocellular carcinoma in segment VII; D: Portal venous phase. Note the capsular appearance (arrow) of the hepatocellular carcinoma; E: Hepatobiliary phase, axial view of T1-weighted three-dimensional gradient-echo magnetic resonance image with fat suppression. The tumor has an obvious hypointense rim (arrow). pT1 hepatocellular carcinoma was diagnosed postoperatively.
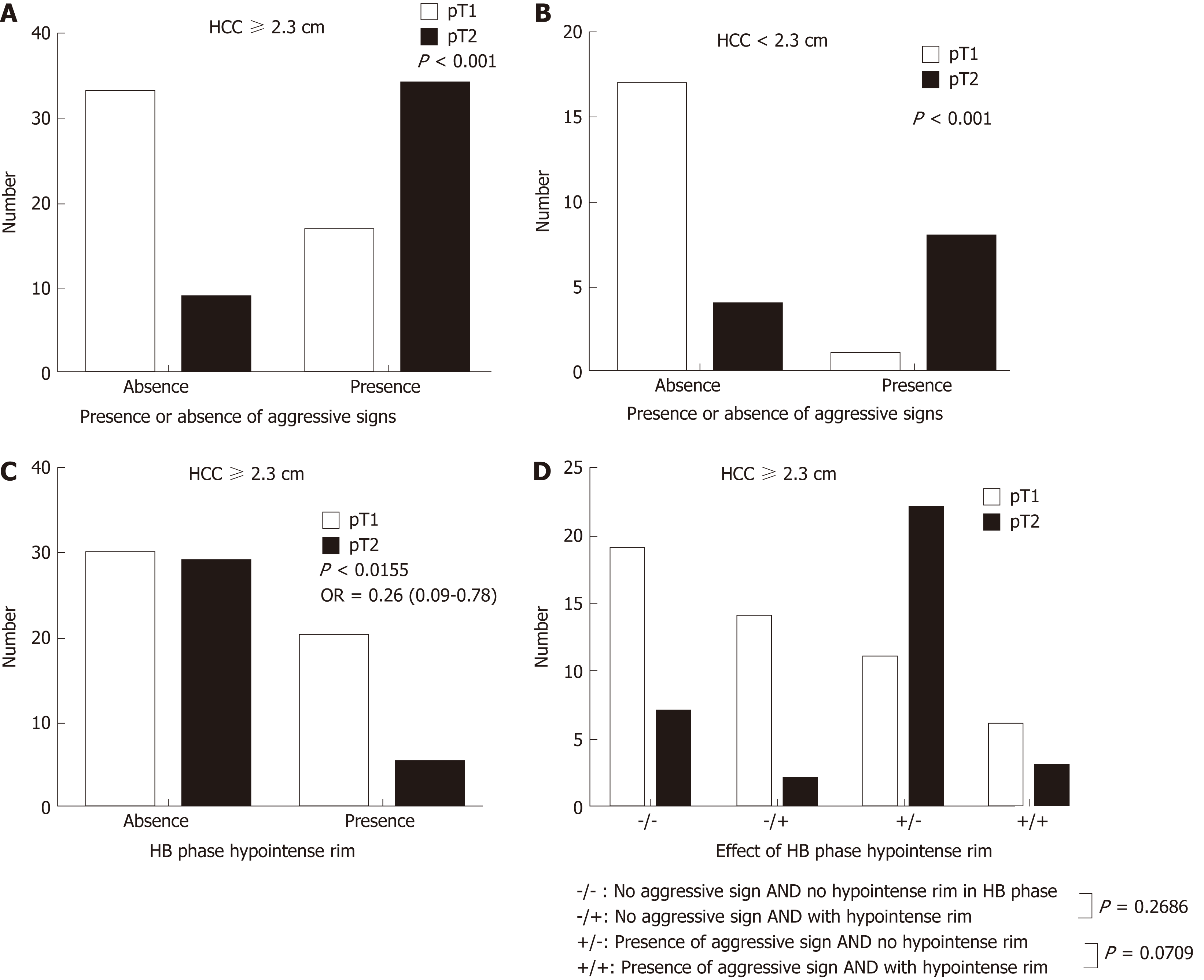
Figure 6 Solitary hepatocellular carcinomas on gadoxetic acid-enhanced magnetic resonance imaging.
Large (≥ 2.3 cm) (A) and small (< 2.3 cm) (B) solitary hepatocellular carcinomas (HCCs) with aggressive imaging findings tend to be stage pT2 tumors (P < 0.001). Large (≥ 2.3 cm) HCCs with hypointense rims on MRI in the HB phase tend to be a stage pT1 tumors (P = 0.0155); C: Large HCCs with aggressive imaging features are more likely to be stage pT2 tumors if a hypointense rim is absent rather than present in the hepatobiliary phase; D: HCC: Hepatocellular carcinoma; HB: Hepatobiliary; pT1: Pathologic stage T1; pT2: Pathologic stage T2.
- Citation: Chou YC, Lao IH, Hsieh PL, Su YY, Mak CW, Sun DP, Sheu MJ, Kuo HT, Chen TJ, Ho CH, Kuo YT. Gadoxetic acid-enhanced magnetic resonance imaging can predict the pathologic stage of solitary hepatocellular carcinoma. World J Gastroenterol 2019; 25(21): 2636-2649
- URL: https://www.wjgnet.com/1007-9327/full/v25/i21/2636.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i21.2636