Copyright
©The Author(s) 2019.
World J Gastroenterol. Mar 21, 2019; 25(11): 1387-1397
Published online Mar 21, 2019. doi: 10.3748/wjg.v25.i11.1387
Published online Mar 21, 2019. doi: 10.3748/wjg.v25.i11.1387
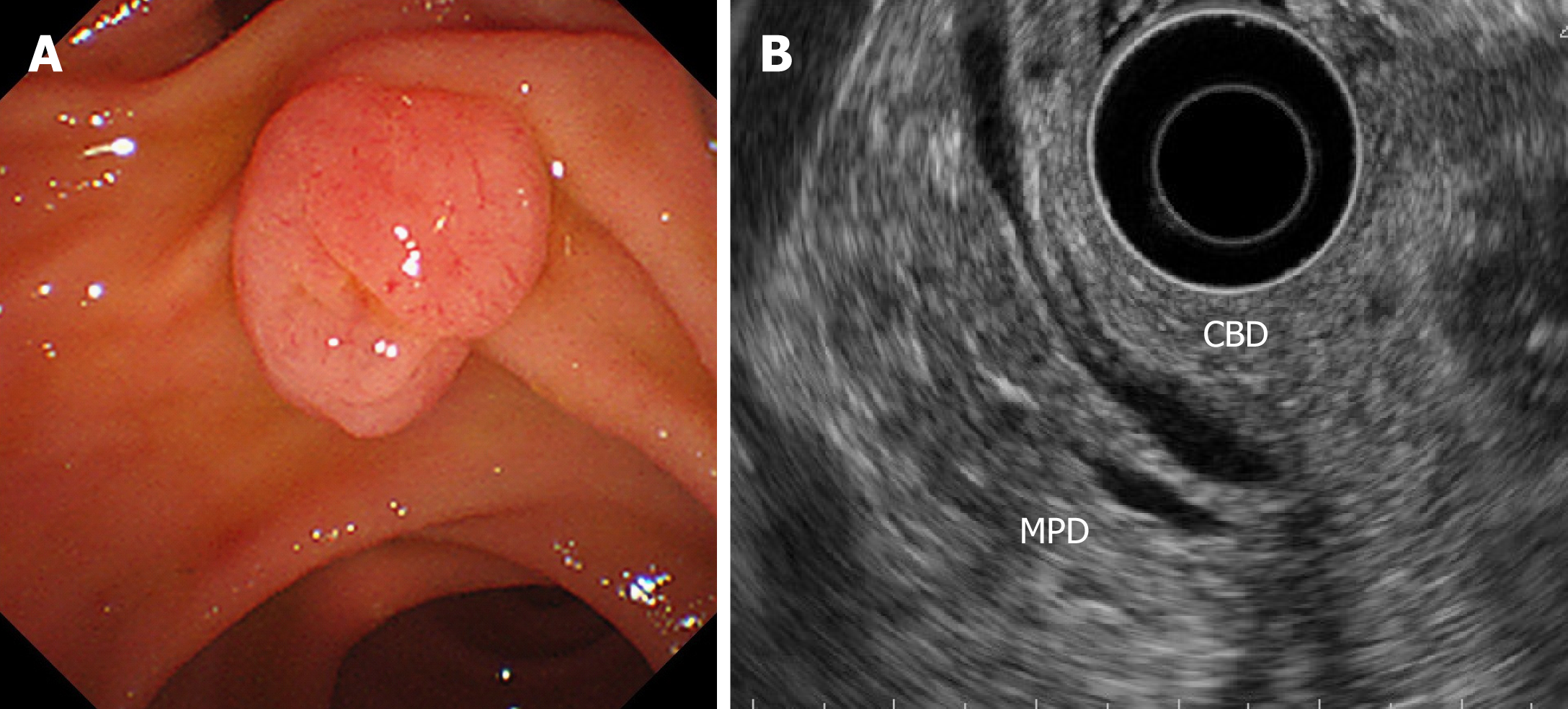
Figure 1 A case of ampullary adenoma that was indicated for endoscopic papillectomy.
A: Duodenoscopy showed an ampullary tumor. The tumor was diagnosed as an adenoma based on an endoscopic biopsy. B: Endoscopic ultrasound did not show any bile/pancreatic duct invasion. CBD: Common bile duct; MPD: Main pancreatic duct.
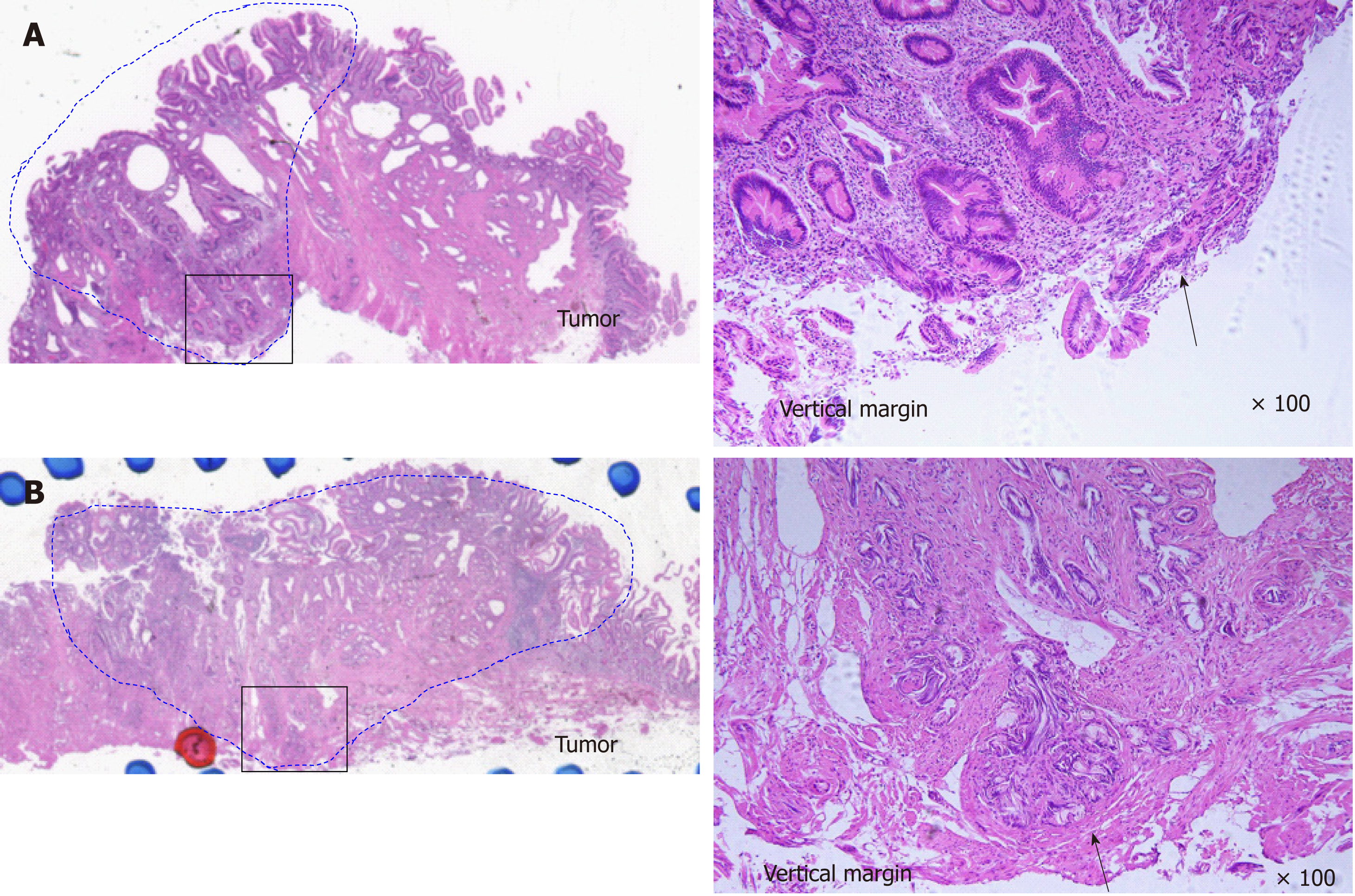
Figure 2 Ampullary adenoma.
A: Ampullary adenoma with vertical margin positive. Tumor is present at resected vertical margin. (black arrow). (left) hematoxylin and eosin, loupe image. (right) hematoxylin and eosin × 100. B: Ampullary adenoma with vertical margin uncertain. Tubular gland is present at resected vertical margin, but it cannot distinguish whether or not the tumor exists because of thermal denaturation (black arrow). (left) Hematoxylin and eosin, loupe image. (right) Hematoxylin and eosin × 100.
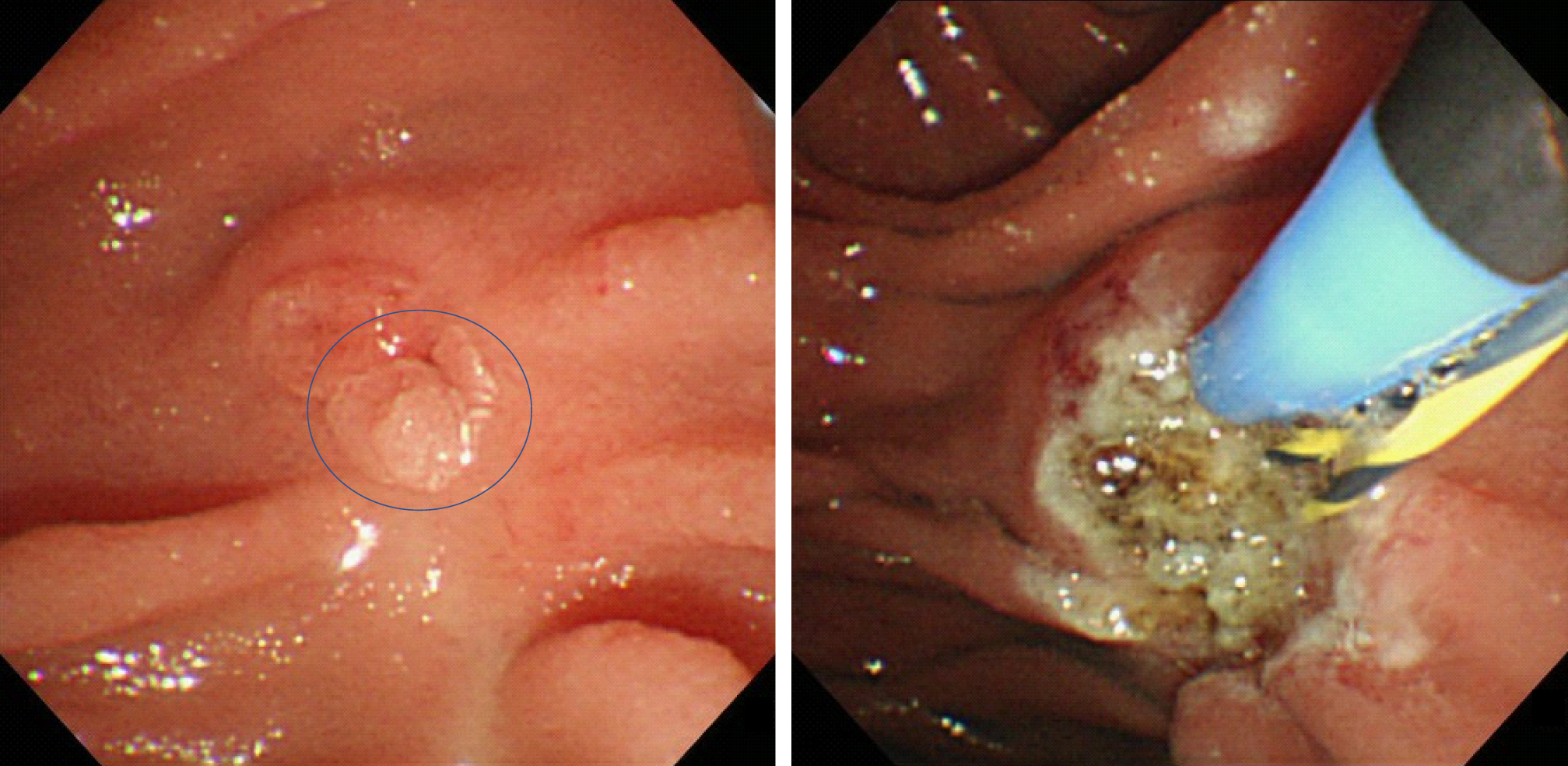
Figure 3 A recurrent tumor that was successfully treated with argon plasma coagulation.
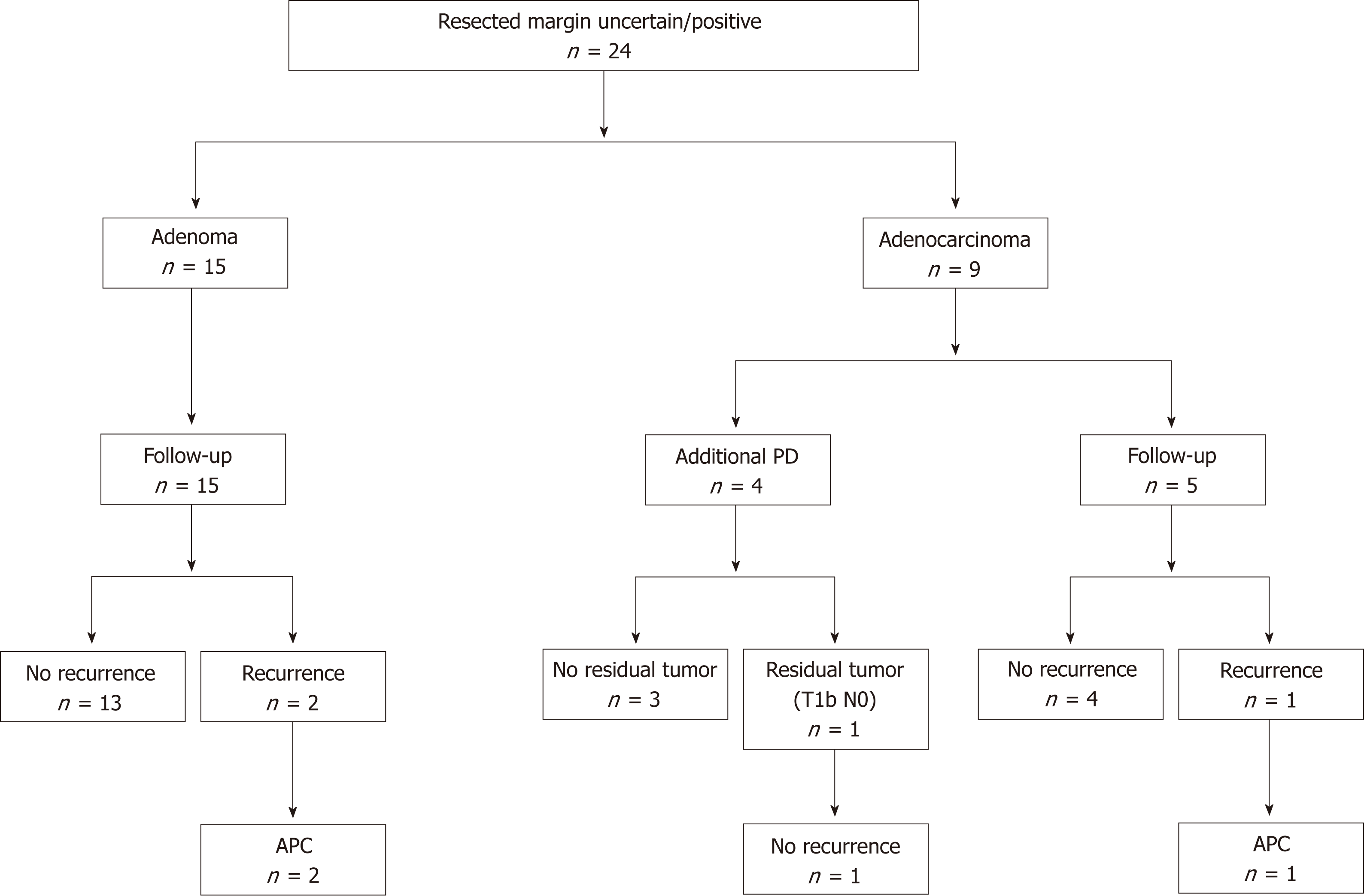
Figure 4 Clinical outcomes of resected margin positive or uncertain cases.
APC: Argon plasma coagulation; PD: Pancreatoduodenectomy.
Figure 5 Clinical outcomes of resected margin negative cases.
APC: Argon plasma coagulation.
- Citation: Sakai A, Tsujimae M, Masuda A, Iemoto T, Ashina S, Yamakawa K, Tanaka T, Tanaka S, Yamada Y, Nakano R, Sato Y, Kurosawa M, Ikegawa T, Fujigaki S, Kobayashi T, Shiomi H, Arisaka Y, Itoh T, Kodama Y. Clinical outcomes of ampullary neoplasms in resected margin positive or uncertain cases after endoscopic papillectomy. World J Gastroenterol 2019; 25(11): 1387-1397
- URL: https://www.wjgnet.com/1007-9327/full/v25/i11/1387.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i11.1387