Copyright
©The Author(s) 2018.
World J Gastroenterol. Oct 21, 2018; 24(39): 4489-4498
Published online Oct 21, 2018. doi: 10.3748/wjg.v24.i39.4489
Published online Oct 21, 2018. doi: 10.3748/wjg.v24.i39.4489
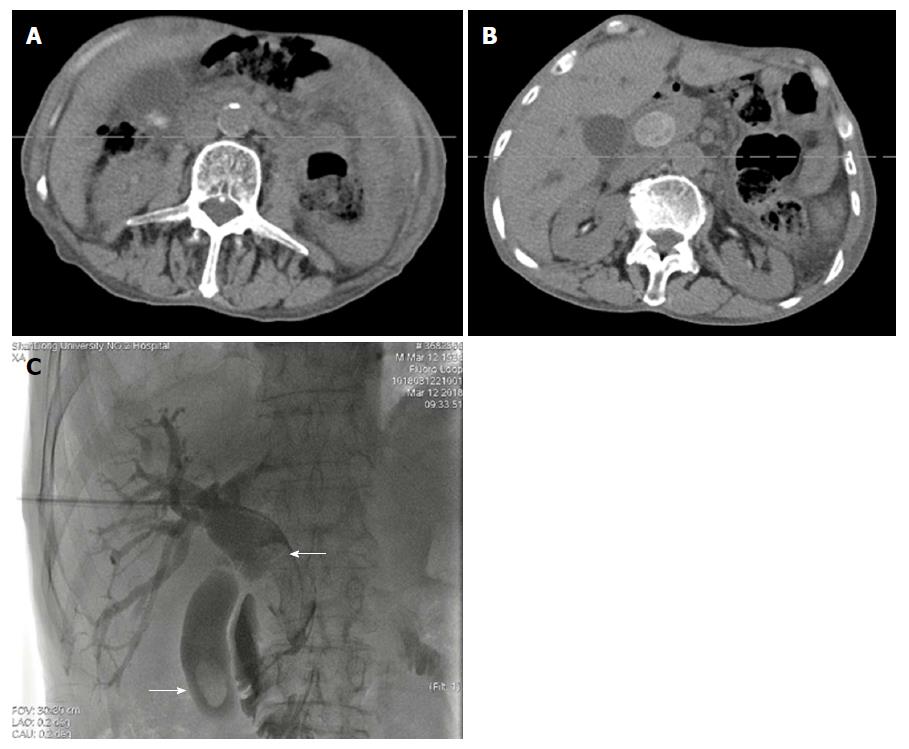
Figure 1 Computed tomography scan and cholangiography showing filling defect in the common bile duct and gallbladder (white arrow).
Dilation of the common bile duct and cystic duct was detected. A and B: Ultrasonography, enhanced computed tomography, magnetic resonance cholangiopancreatography, or cholangiography was carried out to determine the diagnosis of stones; C: Advancing cholangiography was performed to detect the number, size, and location of stones.
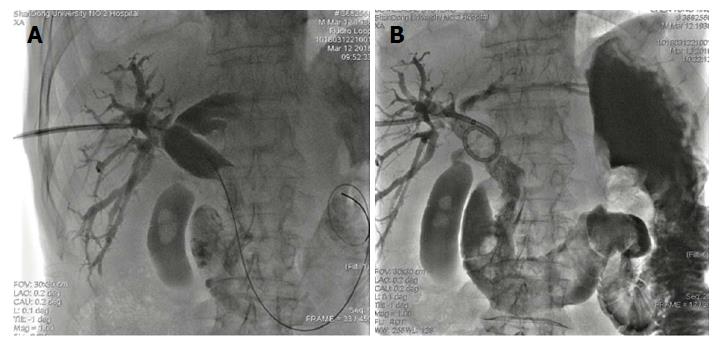
Figure 2 Dilatation of the sphincter of Oddi with a balloon catheter was performed.
Figure 3 Common bile duct stones were expelled into the duodenum through the dilated sphincter.
A and B: An 8.5F external drainage tube was deployed in the common bile duct for postoperative drainage and assessment of efficacy of the procedure.
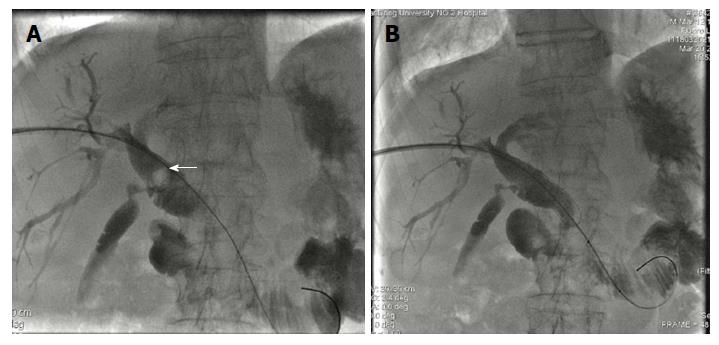
Figure 4 Ursodeoxycholic acid was given and repeated cholangiography was performed.
The secondary common bile duct stones originating from the gallbladder (white arrow) and shrunk gallbladder were detected by cholangiography.
Figure 5 Secondary common bile duct stones (white arrow) were expulsed into the duodenum without gallstone residual.
A and B: After 7-10 d, repeated cholangiography via external drainage catheter was performed, and balloon dilation of the sphincter of Oddi and elimination of stones were carried out in patients with secondary common bile duct stones.
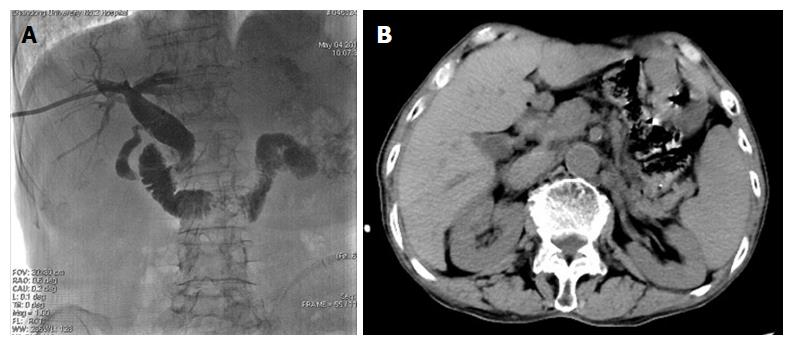
Figure 6 Computed tomography and postoperative cholangiography demonstrating that there was no residual of common bile duct stones or gallstones.
A: Intraoperative cholangiography confirmed the absence of all stones and external drainage tube was left; B: Furthermore, 3-5 d after the procedure, cholangiography was performed again with no residual of stones, and the catheter was retrieved.
- Citation: Chang HY, Wang CJ, Liu B, Wang YZ, Wang WJ, Wang W, Li D, Li YL. Ursodeoxycholic acid combined with percutaneous transhepatic balloon dilation for management of gallstones after elimination of common bile duct stones. World J Gastroenterol 2018; 24(39): 4489-4498
- URL: https://www.wjgnet.com/1007-9327/full/v24/i39/4489.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i39.4489