Copyright
©The Author(s) 2018.
World J Gastroenterol. Oct 21, 2018; 24(39): 4482-4488
Published online Oct 21, 2018. doi: 10.3748/wjg.v24.i39.4482
Published online Oct 21, 2018. doi: 10.3748/wjg.v24.i39.4482
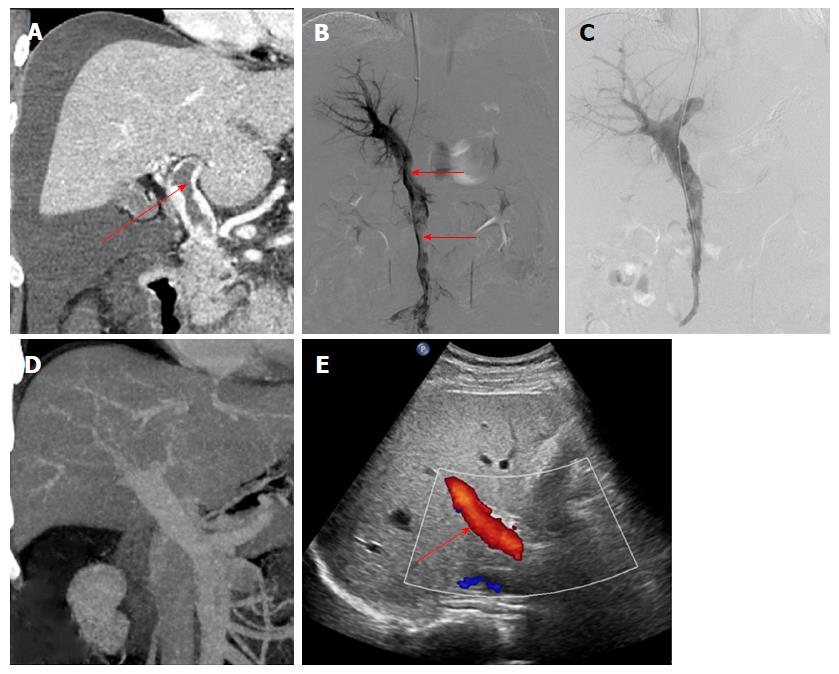
Figure 1 A 29-year-old man had acute abdominal pain and distension for 4 d.
A and B: Contrast-enhanced computed tomography (CT) and portography via the transjugular intrahepatic portosystemic route showed thrombus formation in the portal vein and superior mesenteric vein (arrow) with massive ascites; C: Portography after agitation thrombolysis and catheter-directed thrombolysis showed that the filling defect in the portal vein had decreased; D: Contrast-enhanced CT after surgery showed that the thrombus had disappeared completely; E: At 6 mo after treatment, color Doppler ultrasound showed smooth blood flow in the portal vein (arrow).
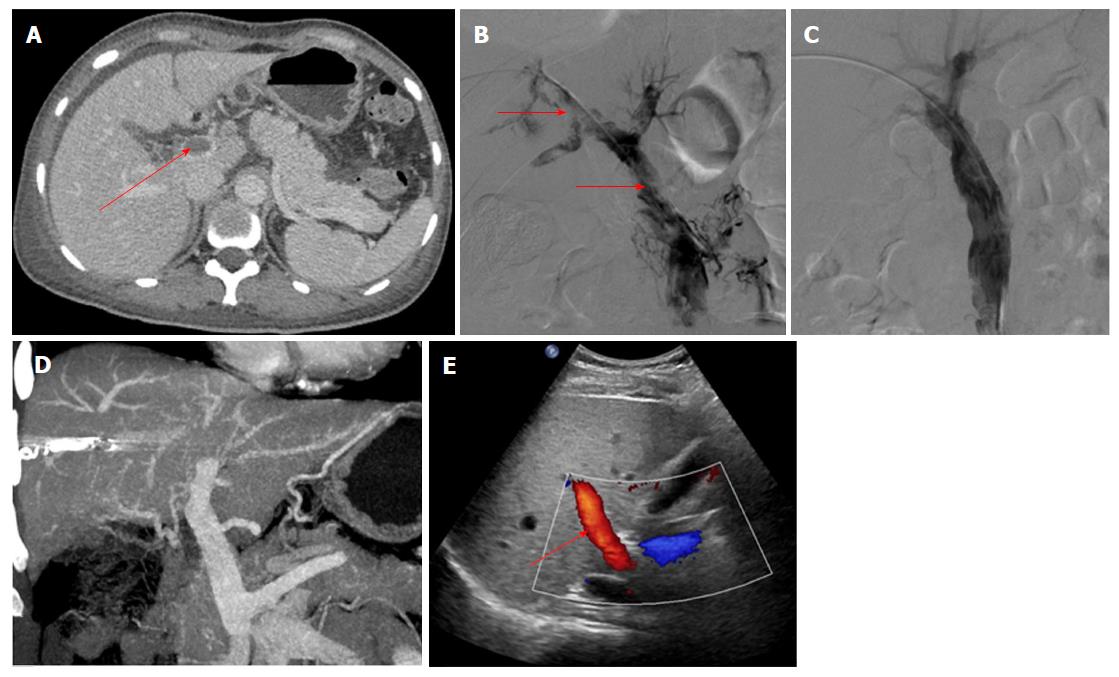
Figure 2 A 57-year-old woman had acute abdominal pain for 16 d.
A and B: Contrast-enhanced computed tomography (CT) and portography via the percutaneous transhepatic route showed thrombus formation in the portal vein and superior mesenteric vein (arrow); C: Portography after agitation thrombolysis and catheter-directed thrombolysis showed that the filling defect in the portal vein had decreased; D: Contrast-enhanced CT after treatment showed that the thrombus had disappeared completely; E: At 12 mo after treatment, color Doppler ultrasound showed smooth blood flow in the portal vein (arrow).
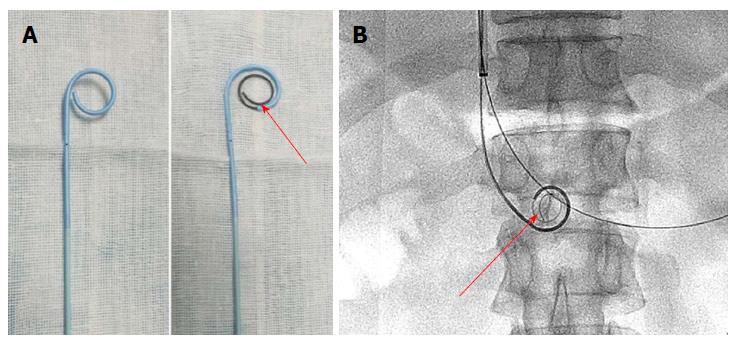
Figure 3 Pigtail catheter was inserted into the thrombus through the sheath, and a guidewire with a helical tip molded in vitro was advanced through the catheter.
A: A pigtail catheter, and a guidewire with a helical tip (arrow) through the catheter in vitro; B: The catheter and guidewire in the portal vein (arrow) during agitation thrombolysis via the transjugular intrahepatic portosystemic route.
- Citation: Wang CY, Wei LQ, Niu HZ, Gao WQ, Wang T, Chen SJ. Agitation thrombolysis combined with catheter-directed thrombolysis for the treatment of non-cirrhotic acute portal vein thrombosis. World J Gastroenterol 2018; 24(39): 4482-4488
- URL: https://www.wjgnet.com/1007-9327/full/v24/i39/4482.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i39.4482