Copyright
©The Author(s) 2018.
World J Gastroenterol. Mar 28, 2018; 24(12): 1285-1298
Published online Mar 28, 2018. doi: 10.3748/wjg.v24.i12.1285
Published online Mar 28, 2018. doi: 10.3748/wjg.v24.i12.1285
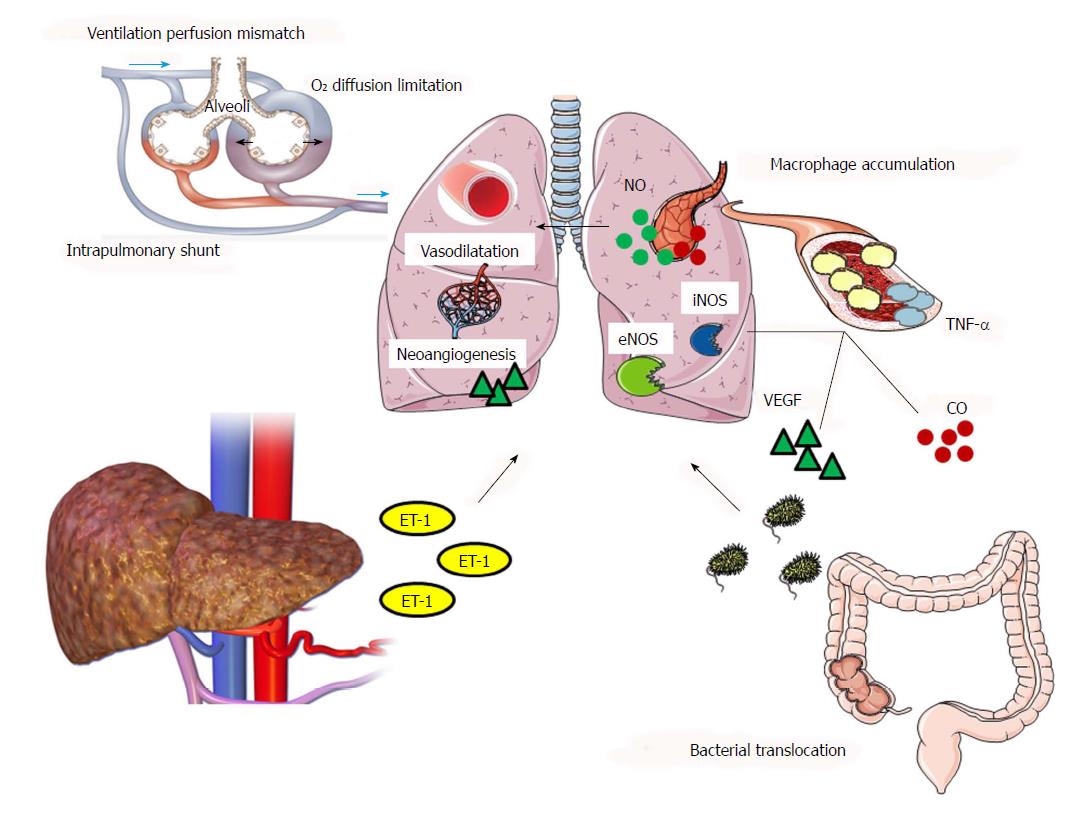
Figure 1 Schematic overview of the main pathways of the pathogenesis of hepatopulmonary syndrome.
Liver cirrhosis and portal hypertension lead to endothelin-1 (ET-1) secretion. The binding of ET-1 to its receptor, activates pulmonary endothelial nitric oxide synthase (eNOS), leading to excessive production of nitric oxide (NO), a natural vasodilator. Bacterial translocation and the subsequent pulmonary macrophage accumulation result in the production of inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-α), which contribute in NO-mediated vasodilatation through inducible nitric oxide synthase (iNOS)-enhanced expression. Carbon monoxide constitutes another pulmonary vasodilator produced by macrophage-induced heme oxygenase-1 (HO-1) increased expression. Pulmonary macrophage accumulation and TNF-α-increased circulation trigger vascular endothelial growth factor (VEGF) pathways, concluding in VEGF-mediated pulmonary angiogenesis. Mixed venous blood passes rapidly, due to hyperdynamic circulation observed in liver cirrhosis, through the dilated capillaries without completing gas exchange. An oxygen (O2) diffusion limitation occurs, as O2 molecules need to cross a longer distance to reach the center of dilated vasculature. As a result, there is an impairment of arterial oxygenation due to ventilation perfusion mismatch, also boosted by direct right-to-left shunt through arteriovenous communications.
- Citation: Soulaidopoulos S, Cholongitas E, Giannakoulas G, Vlachou M, Goulis I. Review article: Update on current and emergent data on hepatopulmonary syndrome. World J Gastroenterol 2018; 24(12): 1285-1298
- URL: https://www.wjgnet.com/1007-9327/full/v24/i12/1285.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i12.1285