Copyright
©The Author(s) 2017.
World J Gastroenterol. Dec 14, 2017; 23(46): 8207-8216
Published online Dec 14, 2017. doi: 10.3748/wjg.v23.i46.8207
Published online Dec 14, 2017. doi: 10.3748/wjg.v23.i46.8207
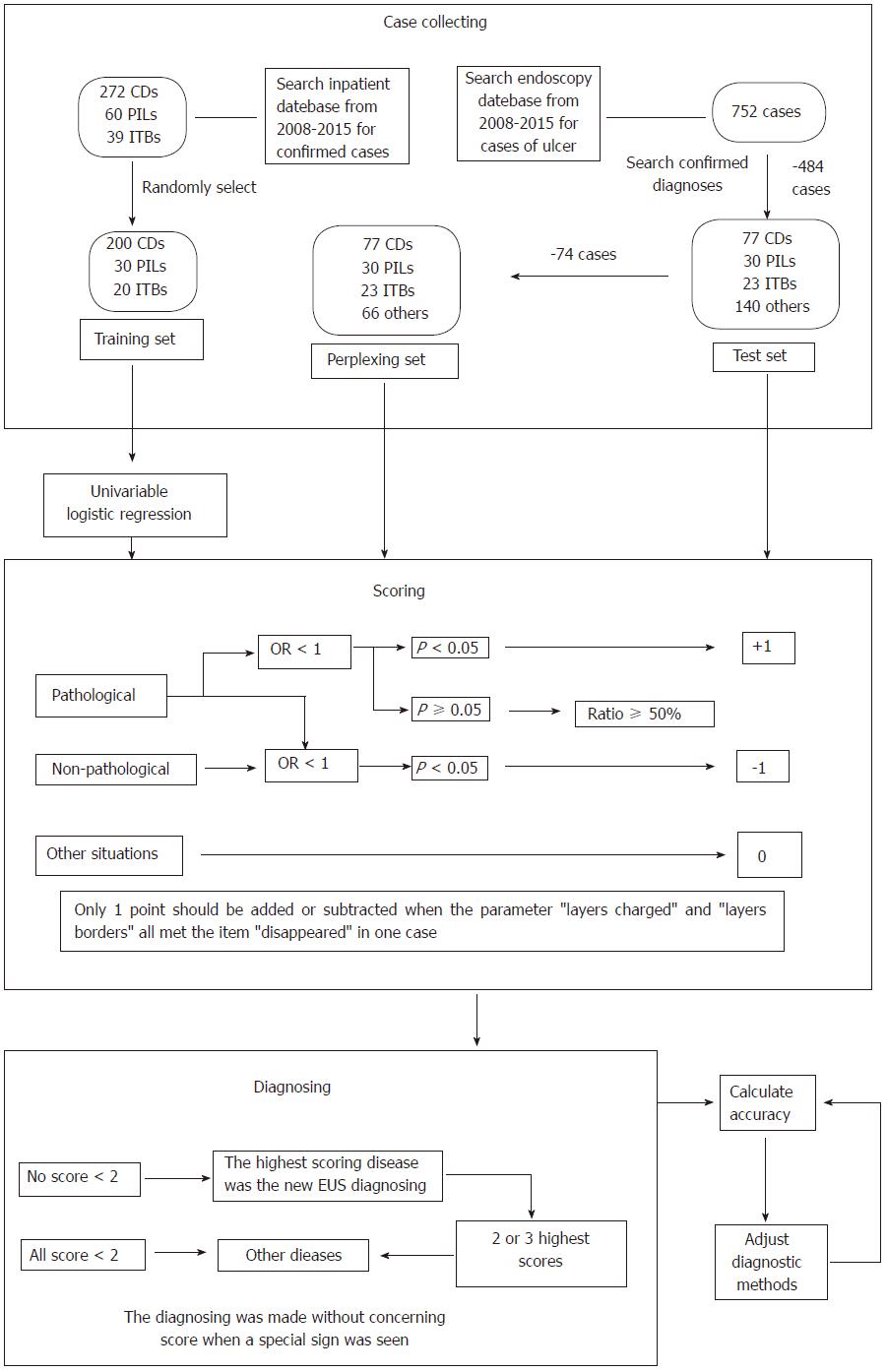
Figure 1 Flowchart of the study.
The cases diagnosed with PIL previously were rediagnosed as cancer when the echo of the lesion was heterogeneous; cases were diagnosed with PIL when a diffuse echo was detected. CD: Crohn’s disease; ITB: Intestinal tuberculosis; OR: Odds ratio; PIL: Primary intestinal lymphoma.
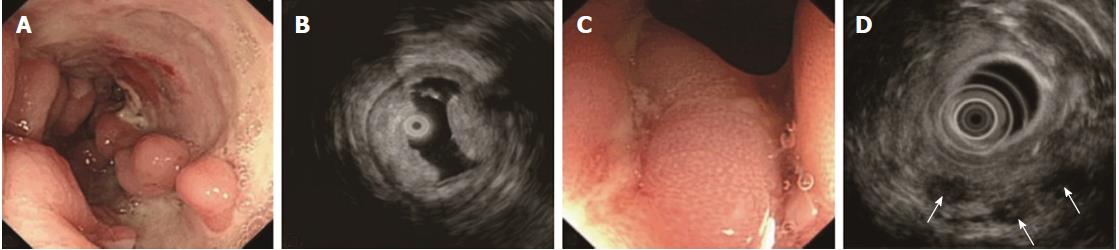
Figure 2 A 21-year-old male with confirmed Crohn’s disease.
A: Multiple irregular ulcers with cobblestone appearance; B: EUS shows heterogeneous thickened bowel wall, thickened SM and absent M; C: Longitudinal ulcers within the swollen M; D: EUS shows irregular heterogeneous hypoechoic areas (arrows) which were considered to be abscesses. CD: Crohn’s disease; EUS: Endoscopic ultrasound; M: Mucosa; SM: Submucosa.
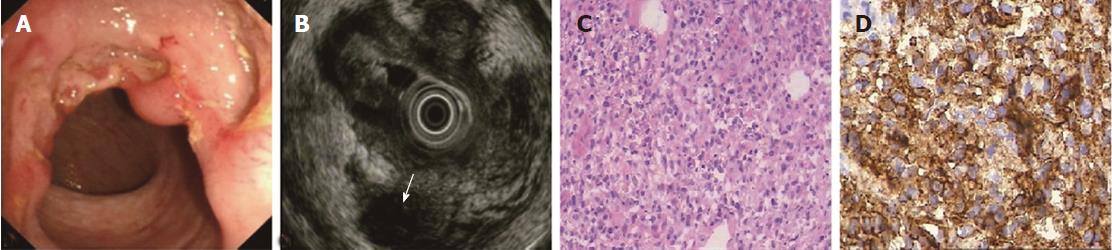
Figure 3 A 58-year-old male with confirmed primary intestinal lymphoma.
A: A circular ulcer with a nodular edge and smooth base; B: EUS shows disappearance of layers, instead of an irregular diffuse area with adjacent nodules (arrow); C, D: Diffuse large B-cell lymphoma confirmed by big-forceps deep biopsy and immunohistochemistry. EUS: Endoscopic ultrasound.
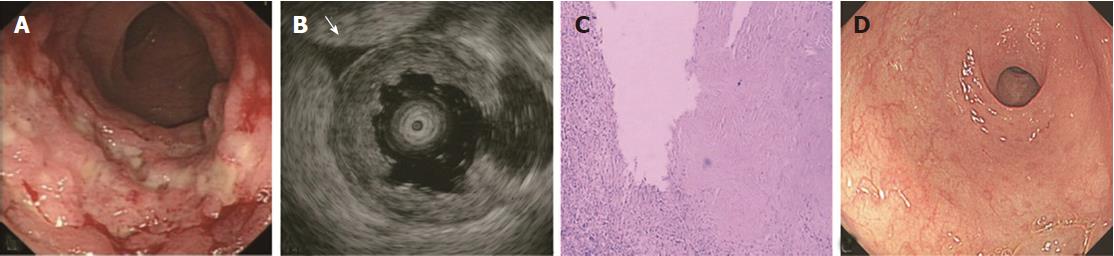
Figure 4 A 49-year-old male with confirmed intestinal tuberculosis.
A: Circular ulcers with a nodular base; B: EUS shows significantly thickened M, thinned obscure SM and extra-luminal fluid sonolucent areas (arrow); C: Biopsy shows caseous necrosis in M; D: Healed M after 4 mo of anti-TB therapy. EUS: Endoscopic ultrasound; M: Mucosa; SM: Submucosa; TB: Tuberculosis.
- Citation: Qiu EQ, Guo W, Cheng TM, Yao YL, Zhu W, Liu SD, Zhi FC. Diagnostic classification of endosonography for differentiating colorectal ulcerative diseases: A new statistical method. World J Gastroenterol 2017; 23(46): 8207-8216
- URL: https://www.wjgnet.com/1007-9327/full/v23/i46/8207.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i46.8207