Copyright
©The Author(s) 2017.
World J Gastroenterol. Jan 7, 2017; 23(1): 11-24
Published online Jan 7, 2017. doi: 10.3748/wjg.v23.i1.11
Published online Jan 7, 2017. doi: 10.3748/wjg.v23.i1.11
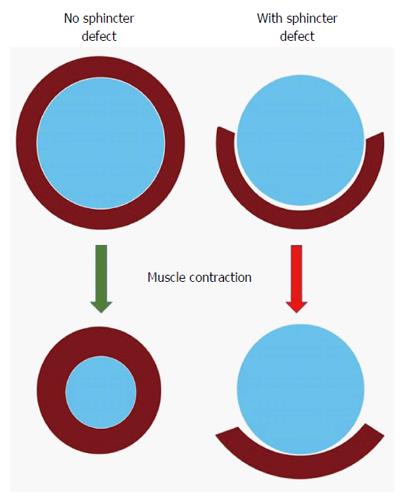
Figure 1 Negative impact of sphincter defect: A normal circumferential muscle configuration results in a concentric contraction and narrowing of the anus (left); if there is a segmental defect in the muscle, contraction may result in shortening of the muscle fibers behind the anus without narrowing it (right).
Figure 2 Keyhole deformity: After a previous fistulotomy, the anus is not patulous but appears to have a deformity (arrow).
Figure 3 Anorectal ultrasound showing an anterior defect in external anal sphincter.
Figure 4 Cloaca-like deformity, corrected with sphincteroplasty and X-flaps.
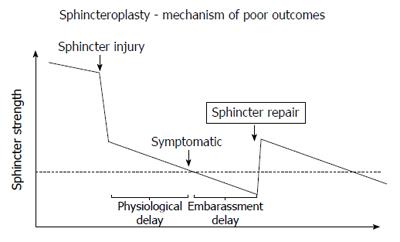
Figure 5 Model for poor outcomes after sphincteroplasty.
Hypothetical model to explain poor outcomes after sphincteroplasty: The graph shows a hypothetical time course (x-axis) of the sphincter strength (y-axis) with the dotted line representing the threshold below which incontinence becomes clinically evident. There may be a natural decline of sphincter strength (time before sphincter injury), a dramatic reduction through the injury, followed by an accelerated decline. The physiological delay represents the time until symptoms evolve, while the embarrassment delay reflects the time until a symptomatic patient acknowledges the problem. A sphincter repair may restore some strength, but with continued and possibly accelerated decline of the sphincter function the threshold is again crossed after a period of time.
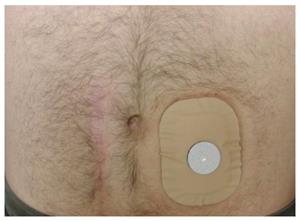
Figure 6 Trained colostomy.
Trained colostomy: After observation of cyclic emptying pattern, in conjunction with appropriate supportive measures (e.g., timed enemas), the patient may not need a true bag, but simply covers the stoma with a mini-appliance with a gas filter.
- Citation: Saldana Ruiz N, Kaiser AM. Fecal incontinence - Challenges and solutions. World J Gastroenterol 2017; 23(1): 11-24
- URL: https://www.wjgnet.com/1007-9327/full/v23/i1/11.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i1.11