Copyright
©The Author(s) 2016.
World J Gastroenterol. Jan 28, 2016; 22(4): 1617-1626
Published online Jan 28, 2016. doi: 10.3748/wjg.v22.i4.1617
Published online Jan 28, 2016. doi: 10.3748/wjg.v22.i4.1617
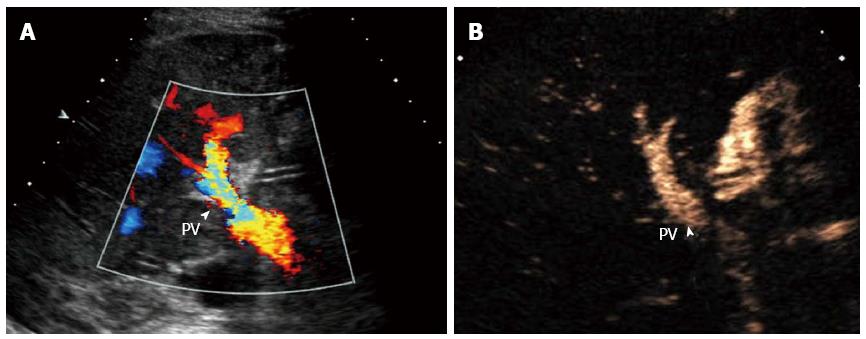
Figure 1 Hepatic artery thrombosis in a 51-year-old woman who underwent right-lobe living donor liver transplantation.
A: Color Doppler ultrasound reveals no hepatic artery flow at the hilus hepatis (arrow head points to the portal vein flow); B: Contrast-enhanced ultrasound shows no enhancement in the hepatic artery neighboring portal vein (arrow head points to the portal vein). PV: Portal vein.
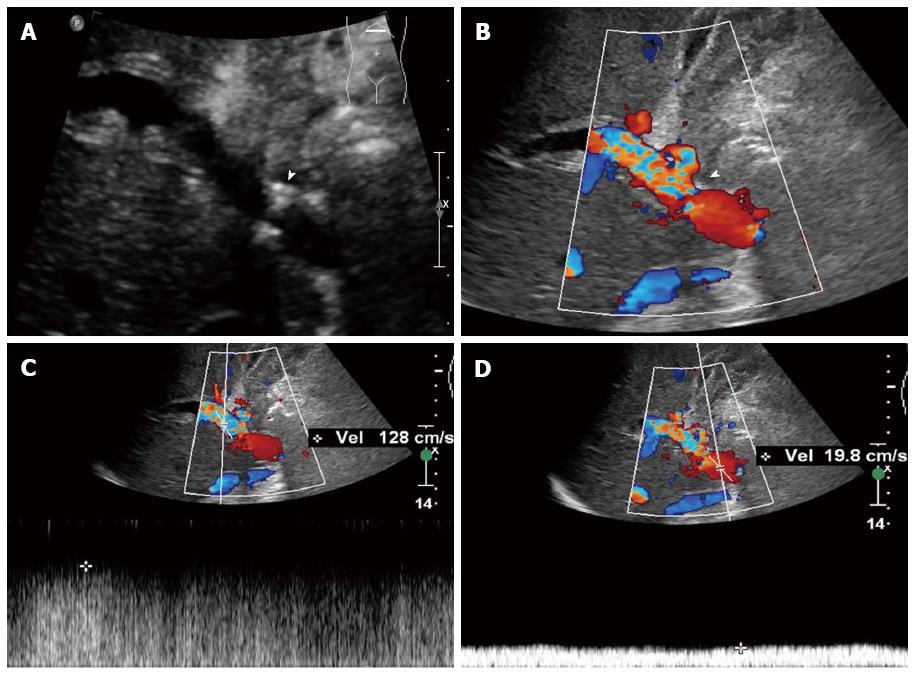
Figure 2 Portal vein stenosis in a 40-year-old woman who underwent right-lobe living donor liver transplantation.
A:Gray-scale ultrasound detected a stenotic region in the portal vein (arrow); B:Color Doppler ultrasound showed disturbance of the blood flow at the stenotic site (arrow); C: Spectrum Doppler ultrasound showed that the blood flow velocity at the stenotic was 128 cm/s; D: Spectrum Doppler ultrasound showed that the blood flow velocity at a pre-stenotic segment of the portal vein was 19.8 cm/s. The ratio between stenotic and pre-stenotic flow was significantly greater than 4:1.
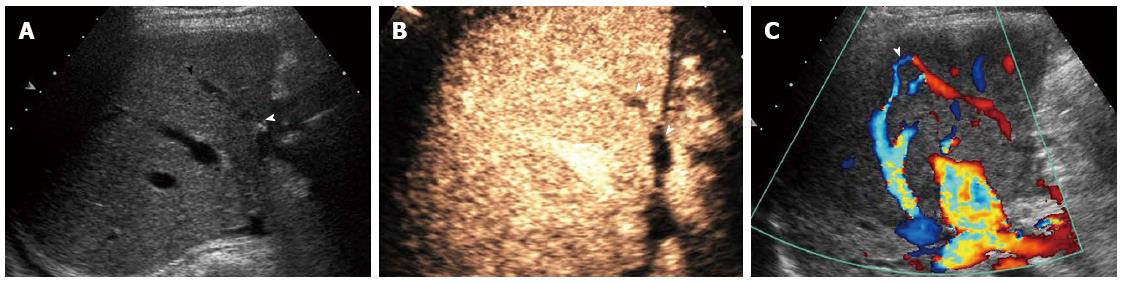
Figure 3 Bridging vein occlusion in a 43-year-old woman who underwent right-lobe living donor liver transplantation sparing the middle hepatic vein.
A:Gray-scale ultrasound showed the bridging vein (arrow); B: Contrast-enhanced ultrasound showed no enhancement in the bridging vein (arrows); C:Color Doppler ultrasound revealed the opening of collateral circulation of intrahepatic veins (arrow).
- Citation: Ma L, Lu Q, Luo Y. Vascular complications after adult living donor liver transplantation: Evaluation with ultrasonography. World J Gastroenterol 2016; 22(4): 1617-1626
- URL: https://www.wjgnet.com/1007-9327/full/v22/i4/1617.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i4.1617