Copyright
©The Author(s) 2016.
World J Gastroenterol. Oct 21, 2016; 22(39): 8670-8683
Published online Oct 21, 2016. doi: 10.3748/wjg.v22.i39.8670
Published online Oct 21, 2016. doi: 10.3748/wjg.v22.i39.8670
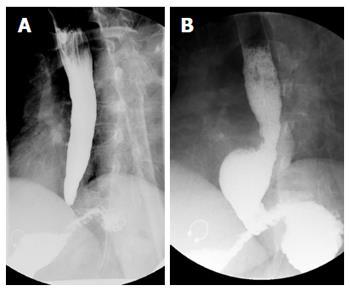
Figure 1 Barium esophagram of a patient before and several months after per oral endoscopic myotomy.
A 45-year-old woman with type II achalasia underwent per oral endoscopic myotomy (POEM). The pre-procedural barium esophagram (A, left panel) demonstrated a dilated esophagus with tapering at the gastroesophageal junction. Following POEM the patient gained 32 lbs over a 9-mo period but had occasional symptoms of regurgitation, which we suspected was from eating too much too quickly. Repeat barium esophagram showed the distal tapering of the gastroesophageal junction has resolved and there was immediate and unimpeded passage contrast passage into the stomach (B, right panel). A distal esophageal diverticulum was incidentally found, which can be seen in patients following POEM with a complete myotomy of the distal esophagus that is carried across the lower esophageal sphincter and into the gastric cardia.
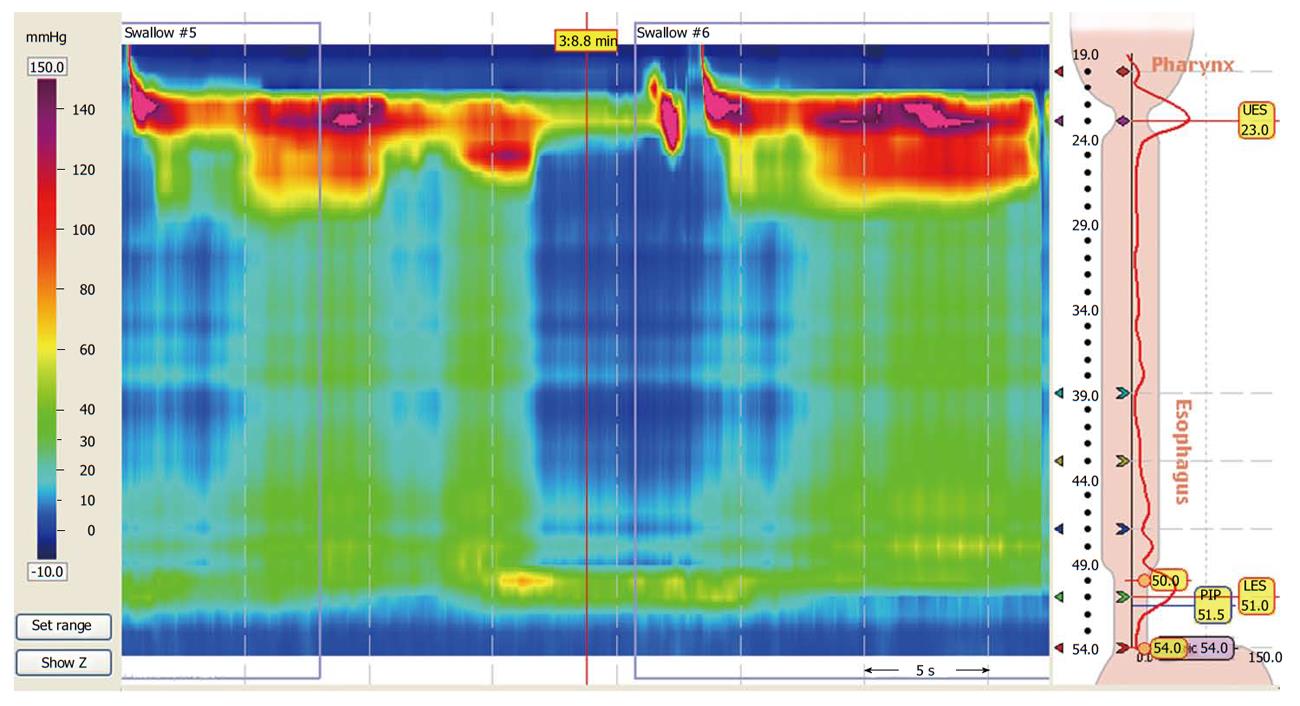
Figure 2 High-resolution esophageal manometry of a patient with achalasia.
A 34-year-old man with progressive dysphagia to liquids and solids had a barium esophagram suggestive of achalasia. He presented for high-resolution manometry to confirm the diagnosis of achalasia. The manometric and topographic findings demonstrated aperistalsis with residual pressure at the lower esophageal sphincter with an elevated integrated relaxation pressure and pan-esophageal pressurization, which was consistent with type II achalasia by the Chicago classification.
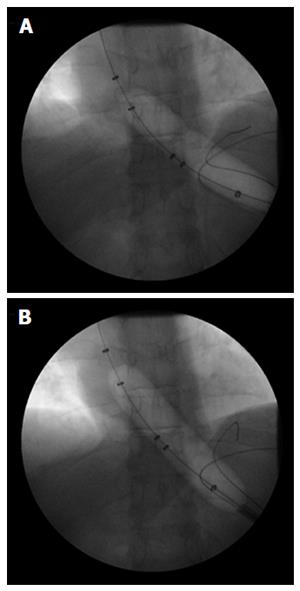
Figure 3 Pneumatic balloon dilation of the lower esophageal sphincter in a patient with achalasia.
A 44-year-old man with type II achalasia underwent pneumatic dilation of the lower esophageal sphincter (LES) under fluoroscopic guidance to 30 mm in diameter. The pneumatic balloon catheter was passed across the LES over a wire and then inflated with initial evidence of a waist in the mid-portion of the balloon (A); The balloon was kept inflated until the waist in the balloon was obliterated (B). A barium esophagram done immediately following pneumatic dilation showed no evidence of perforation.
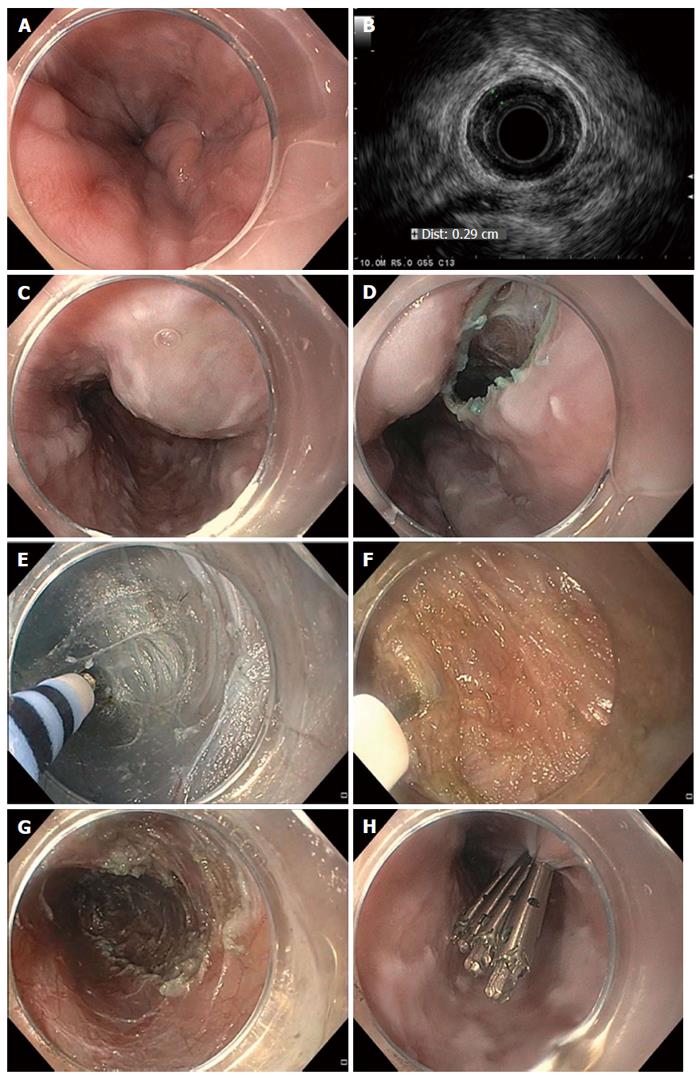
Figure 4 Per oral endoscopic myotomy in a patient with achalasia.
A 56-year-old man with type II achalasia and a history of chronic alcohol use underwent attempted laparoscopic Heller myotomy. Upon retraction of the liver during surgery, large gastroesophageal varices were noted to arise and the surgery was aborted. The patient was exhorted to stop drinking alcohol. Doppler ultrasonography and magnetic resonance imaging with arterial and venous phase imaging did not show any significant gastroesophageal varices or obvious portal hypertension. Per oral endoscopic myotomy (POEM) was performed. Endoscopic views in the distal esophagus found some enlarged veins but no high-grade esophageal or gastric varices (A); Radial endosonography found a thickened deep circular muscle layer measuring 2.9 mm, which is commonly found in patients with achalasia, but no obvious esophageal varices were noted (B); A mucosal weal was created by injecting saline tinted with indigo carmine (C); and a mucosal entry incision was made (D); Submucosal dissection was carried out with sequential injection and electrosurgical dissection (E) using a T-type Hybrid knife in conjunction with an ERBEJET 2 and a VIO 300 D generator set at EndoCut Q 3-2-1 (ERBE, Marietta, GA, United States). Dissection of the circular layer of the muscularis propria was performed using the T-type Hybrid knife (F); After completion of the 7-cm-long myotomy in the distal esophagus that was carried out an additional 2 cm into the gastric cardia (G); the mucosal entry site was closed by using endoclips (H). The patient did well without any intra- or post-procedural bleeding. At clinic follow-up 2 mo later, the patient reported complete resolution of his symptoms of dysphagia and weight gain of 14 lbs.
- Citation: Uppal DS, Wang AY. Update on the endoscopic treatments for achalasia. World J Gastroenterol 2016; 22(39): 8670-8683
- URL: https://www.wjgnet.com/1007-9327/full/v22/i39/8670.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i39.8670