Copyright
©The Author(s) 2016.
World J Gastroenterol. Sep 21, 2016; 22(35): 7983-7998
Published online Sep 21, 2016. doi: 10.3748/wjg.v22.i35.7983
Published online Sep 21, 2016. doi: 10.3748/wjg.v22.i35.7983
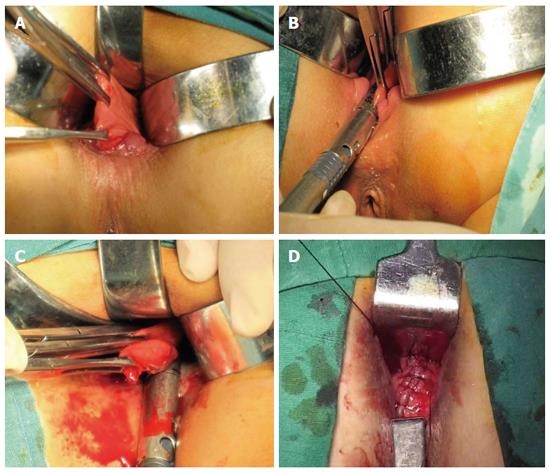
Figure 1 Surgical technique of Bresler procedure.
A: The anterior wall of the defect in the rectum should be raised with two or three Allis clamps, and it should be ensured every time that it does not involve the posterior wall of the vagina to avoid further complications; B, C: A single use, reloadable endoscopic linear cutter is introduced, and one or two firings might be necessary depending on the extent of prolapse seen in the rectocele; D: A longitudinal locked running suture, including rectal mucosa, submucosa, and muscle, was made with 2-0 absorbable Vicryl suture along the staple line for the plication of the repaired anterior rectal wall to strengthen the stapled region.
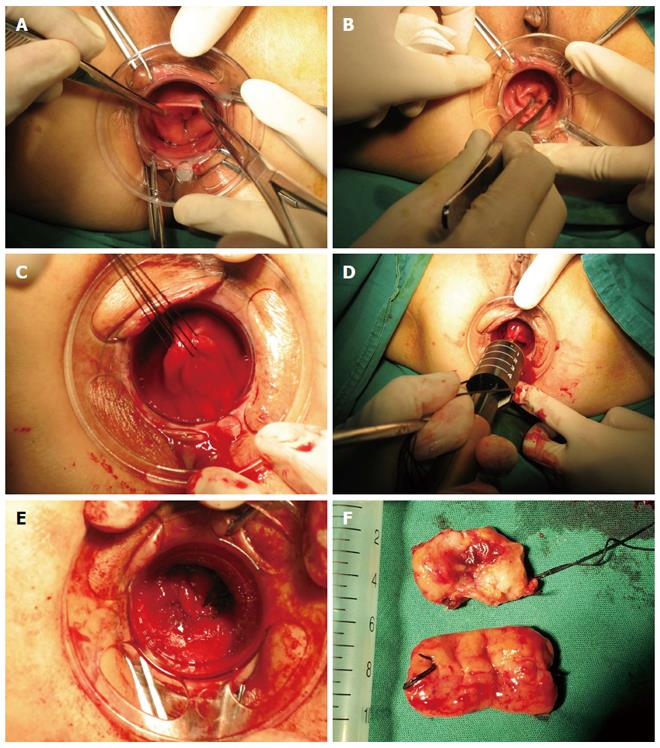
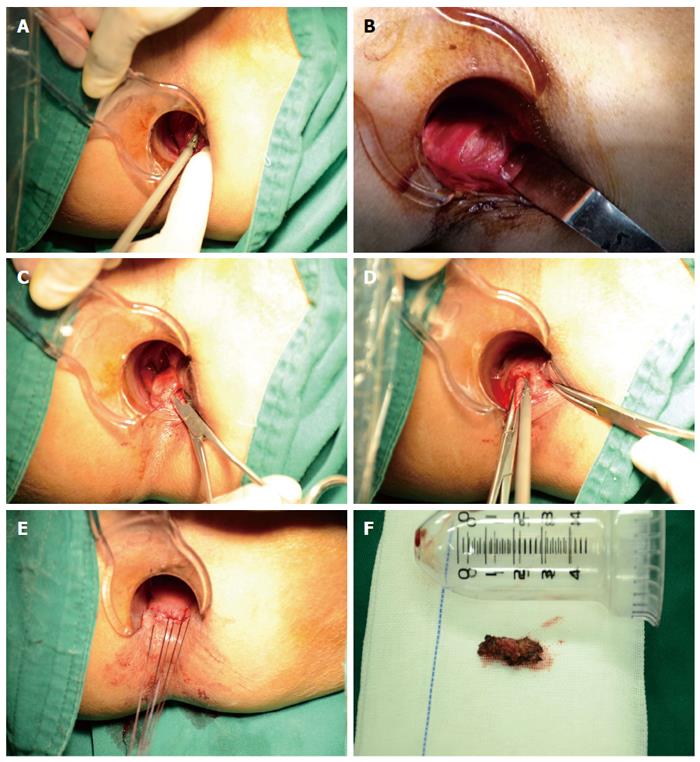
Figure 2 Surgical technique of prolapse and hemorrhoids-stapled transanal rectal resection procedure.
A, B: A CAD was introduced into the anal canal, and a sterile betadine gauze hold with a pincer should be used to draw the prolapsed tissue inside the dilator; C: Three purse-string sutures in all of the layers of the rectum were made at 1 cm intervals using Prolene 2-0 in the anterior area of the rectum at 4 cm above the dentate line and from the 9 o’clock direction to the 3 o’clock direction including the apex of the anterior rectocele; D: A PPH device was inserted into the anal canal and closed and fired to perform the rectal anastomosis, and the staple line was reinforced using a 3-0 absorbable Vicryl suture; E: The same procedure was repeated on the posterior rectal wall; F: The resected sample. PPH: Procedure for prolapse and hemorrhoids; STARR: Stapled transanal rectal resection; CAD: Circular anal dilator.
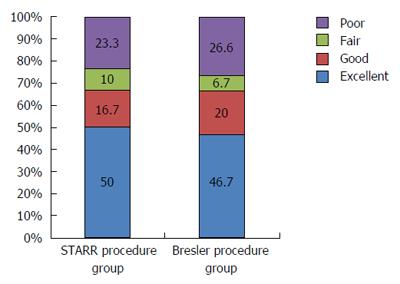
Figure 3 Short-term follow-up of postoperative satisfaction grade of both prolapse and hemorrhoids-stapled transanal rectal resection procedure and Bresler procedure.
In 30 patients who underwent PPH-STARR procedure, there were 15 (50%) persons who felt excellent and five (16.7%) persons who felt good post operation. And there were three (10%) persons who just said fair and seven (23.3%) persons complaining about poor outcome after operation. In 30 patients who underwent Bresler procedure, there were 14 (46.7%) persons who felt excellent and six (20%) persons who felt good post operation. And there were two (6.7%) persons who just said fair and eight (26.6%) persons complaining about poor outcome after operation. PPH: Procedure for prolapse and hemorrhoids; STARR: Stapled transanal rectal resection.
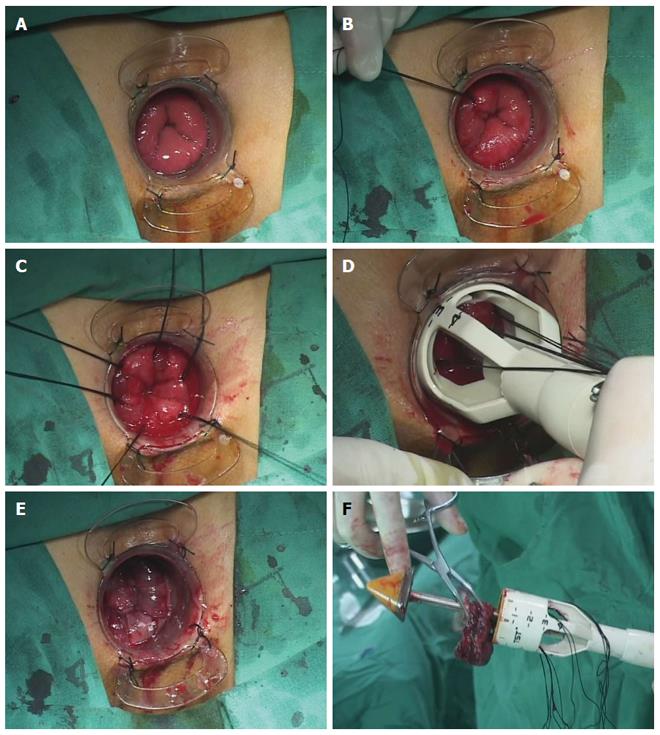
Figure 4 Surgical technique of tissue selecting therapy-stapled transanal rectal resection procedure.
A: A CAD was gently introduced and fixed to the perianal skin after digital anal dilatation to assess the scope and degree of prolapse and rectocele; B, C: The parachute technique with six figure-eight sutures was used to pull out the rectocele and prolapsed tissues, and the depth of each suture should reach the rectal muscular layer; D: A 36-mm TST stapler was placed through the CAD, and all traction lines were pulled out through the mega windows; E: The stapler was closed and fired to perform the rectal anastomosis, and the staple line was reinforced using a 3-0 absorbable Vicryl suture; F: The resected sample. TST: Tissue selecting therapy; STARR: Stapled transanal rectal resection; CAD: Circular anal dilator.
Figure 5 Technique of transanal partial excision of the puborectalis.
A: Making a lateral incision of approximately 3 cm located 1 cm up on the dentate line on the rectal mucosa from the 3 o’clock direction to the 5 o’clock direction using an ultrasound knife; B: The rectal postero-lateral wall was dissected to the puborectalis; C, D: The puborectalis muscle was lifted up and approximately 2 cm was removed with an ultrasound knife; E: A full-thickness suture of the rectal wall was carried out; F: The resected sample.
- Citation: Liu WC, Wan SL, Yaseen S, Ren XH, Tian CP, Ding Z, Zheng KY, Wu YH, Jiang CQ, Qian Q. Transanal surgery for obstructed defecation syndrome: Literature review and a single-center experience. World J Gastroenterol 2016; 22(35): 7983-7998
- URL: https://www.wjgnet.com/1007-9327/full/v22/i35/7983.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i35.7983