Copyright
©The Author(s) 2015.
World J Gastroenterol. Nov 14, 2015; 21(42): 11887-11892
Published online Nov 14, 2015. doi: 10.3748/wjg.v21.i42.11887
Published online Nov 14, 2015. doi: 10.3748/wjg.v21.i42.11887
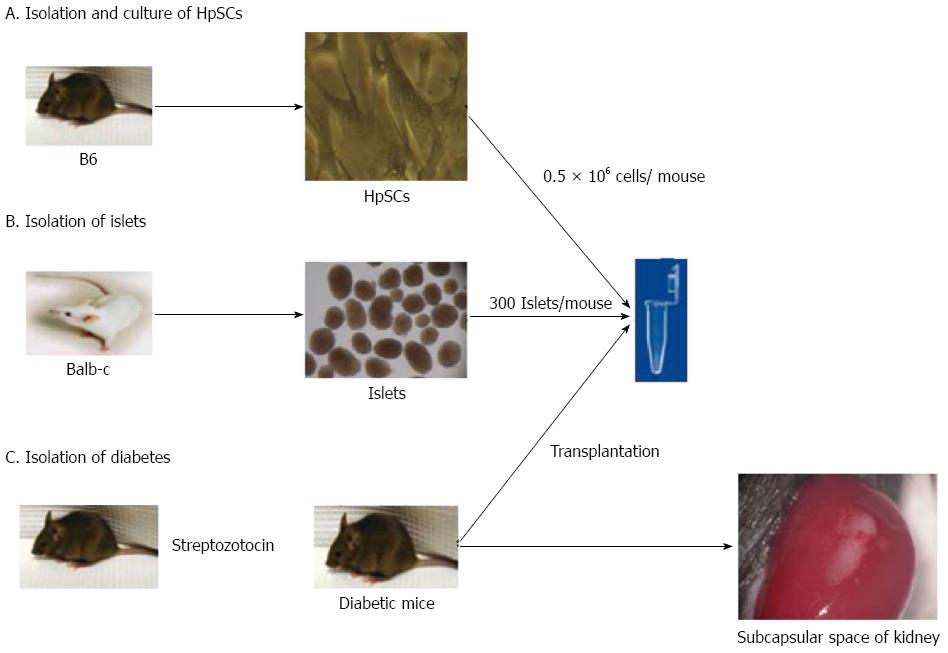
Figure 1 Hepatic stellate cells cotransplanted allogeneic islet animal model.
Diabetes was induced in recipients with a single intraperitoneal injection of streptozotocin (220 mg/kg body weight). Only mice with nonfasting blood glucose levels exceeding 350 mg/dL were used as recipients. Islets were isolated from donor pancreas by collagenase V. After separation on a Ficoll gradient, the islets were purified by hand picking. Three hundred freshly isolated islets alone or mixed with 1 or 3 × 105 hepatic stellate cells (HpSCs) were aspirated into polyethylene tubing, pelleted by centrifugation for 2 min, and then gently placed under the subcapsular space of the recipient kidney. Transplantation was considered successful if the nonfasting blood glucose returned to and remained normal (< 150 mg/dL) for the first 4 d after transplantation. The tail vein nonfasting blood glucose level was monitored after transplantation, and the first day of 2 consecutive readings of blood glucose levels greater than 350 mg/dL was defined as the date of diabetes onset. No immunosuppressive reagents were administered throughout the experiments.
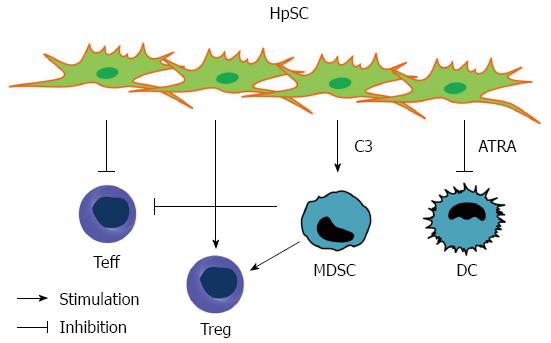
Figure 2 Immune regulatory functions of hepatic stellate cells.
Hepatic stellate cells exert potent immune regulatory mechanisms to prevent immense inflammation in the liver. Hepatic stellate cells (HpSCs) can induce regulatory T cells and inhibit effector T cells responses and the function of APCs. These mechanisms contribute to the unique immune tolerant microenvironment of the liver. DCs: Dendritic cells; MDSCs: Myeloid-derived suppressor cells; Treg: Regulatory T cells; Teff: Effector T cells; ATRA: All-trans retinoic acid; C3: Complement component 3.
- Citation: Hsieh CC, Hung CH, Lu L, Qian S. Hepatic immune tolerance induced by hepatic stellate cells. World J Gastroenterol 2015; 21(42): 11887-11892
- URL: https://www.wjgnet.com/1007-9327/full/v21/i42/11887.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i42.11887