Copyright
©The Author(s) 2015.
World J Gastroenterol. Aug 21, 2015; 21(31): 9253-9261
Published online Aug 21, 2015. doi: 10.3748/wjg.v21.i31.9253
Published online Aug 21, 2015. doi: 10.3748/wjg.v21.i31.9253
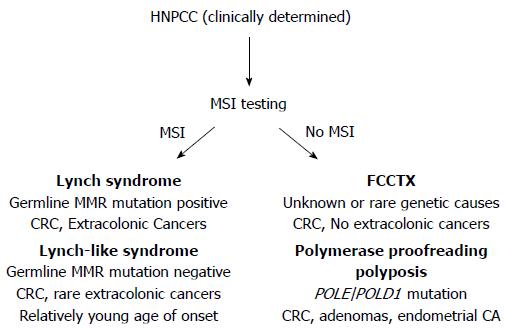
Figure 1 Hereditary non-polyposis colorectal cancer conditions can be dichotomized via microsatellite instability testing and/or DNA mismatch repair protein immunohistochemistry.
When MSI [or loss of mismatch repair (MMR) protein expression] is present in the colorectal cancer indicating loss of functional DNA MMR, Lynch syndrome and Lynch-like syndrome remain in the differential. Germline testing for DNA MMR gene mutation can differentiate these two syndromes. When MSI is absent meaning DNA MMR remains intact and functional, consideration for polymerase proofreading associated polyposis and familial colorectal cancer type X should be undertaken. Performing germline testing for POLE and POLD1 mutations might help differentiate these two syndromes. HNPCC: Hereditary non-polyposis colorectal cancer; MSI: Microsatellite instability; CRC: Colorectal cancer.
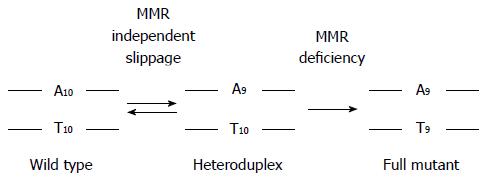
Figure 2 Loss of DNA mismatch repair forces polymerase slippage mistakes to become permanent frameshift mutations at microsatellite sequences.
Depicted is a mononucleotide microsatellite of 10 adenines. During DNA replication, occasional polymerase mistakes allow slippage at microsatellite sequences, creating a heteroduplex structure often with one nucleotide as a loop. With intact DNA mismatch repair (MMR), the deletion loop is recognized, excised, and resynthesized correctly such that daughter cells will maintain fidelity of the proper microsatellite length. In the absence of DNA MMR, the deletion loop becomes a permanent frameshift in daughter cells. Frameshift mutations can occur in non-coding as well as in coding microsatellites; coding frameshifts cause the transcription and ultimate translation of truncated proteins that can act as neoantigens to the immune system.
- Citation: Carethers JM, Stoffel EM. Lynch syndrome and Lynch syndrome mimics: The growing complex landscape of hereditary colon cancer. World J Gastroenterol 2015; 21(31): 9253-9261
- URL: https://www.wjgnet.com/1007-9327/full/v21/i31/9253.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i31.9253