Copyright
©The Author(s) 2015.
World J Gastroenterol. Aug 7, 2015; 21(29): 8739-8752
Published online Aug 7, 2015. doi: 10.3748/wjg.v21.i29.8739
Published online Aug 7, 2015. doi: 10.3748/wjg.v21.i29.8739
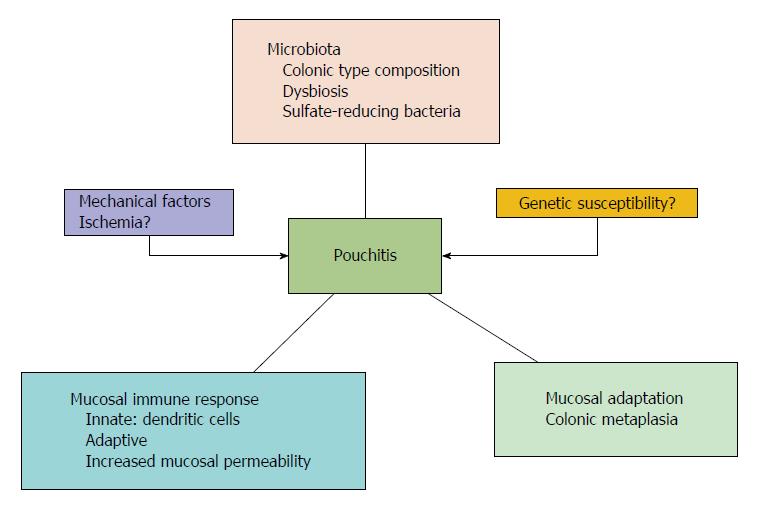
Figure 1 Idiopathic pouchitis pathogenesis.
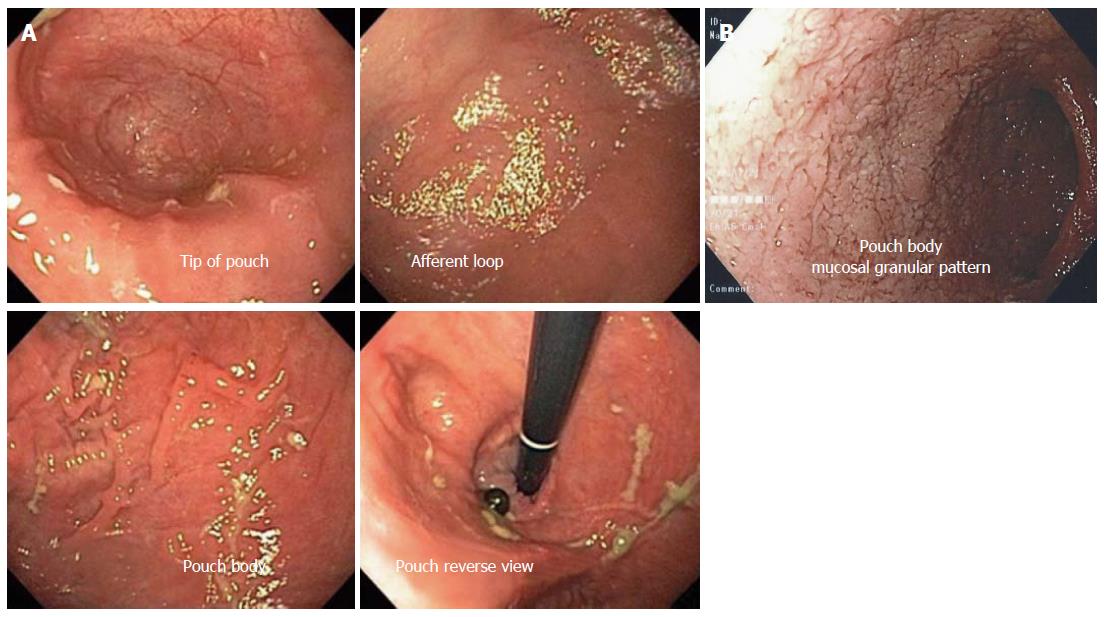
Figure 3 Normal pouch mucosa (A), mucosal granular pattern (edema) with disappearance of the mucosal vascular pattern (B).
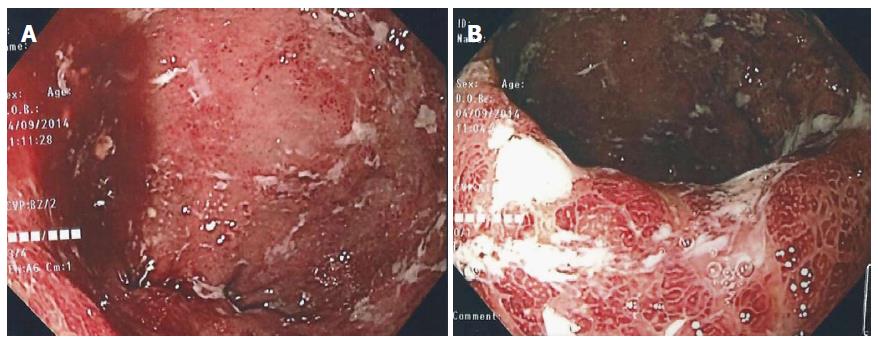
Figure 4 Active pouchitis (A, B).
The mucosal vascular pattern has been lost and the mucosa is characterized by diffuse redness, severe edema with erosions and ulcers.
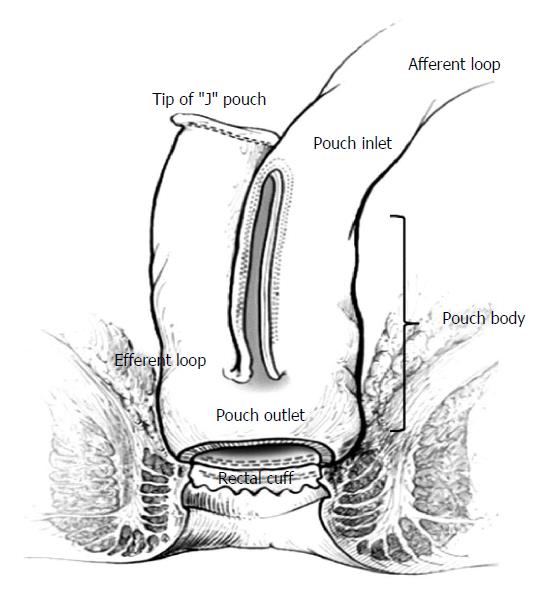
Figure 2 The J-pouch anatomy (adapted and modified from Cima et al[40]).
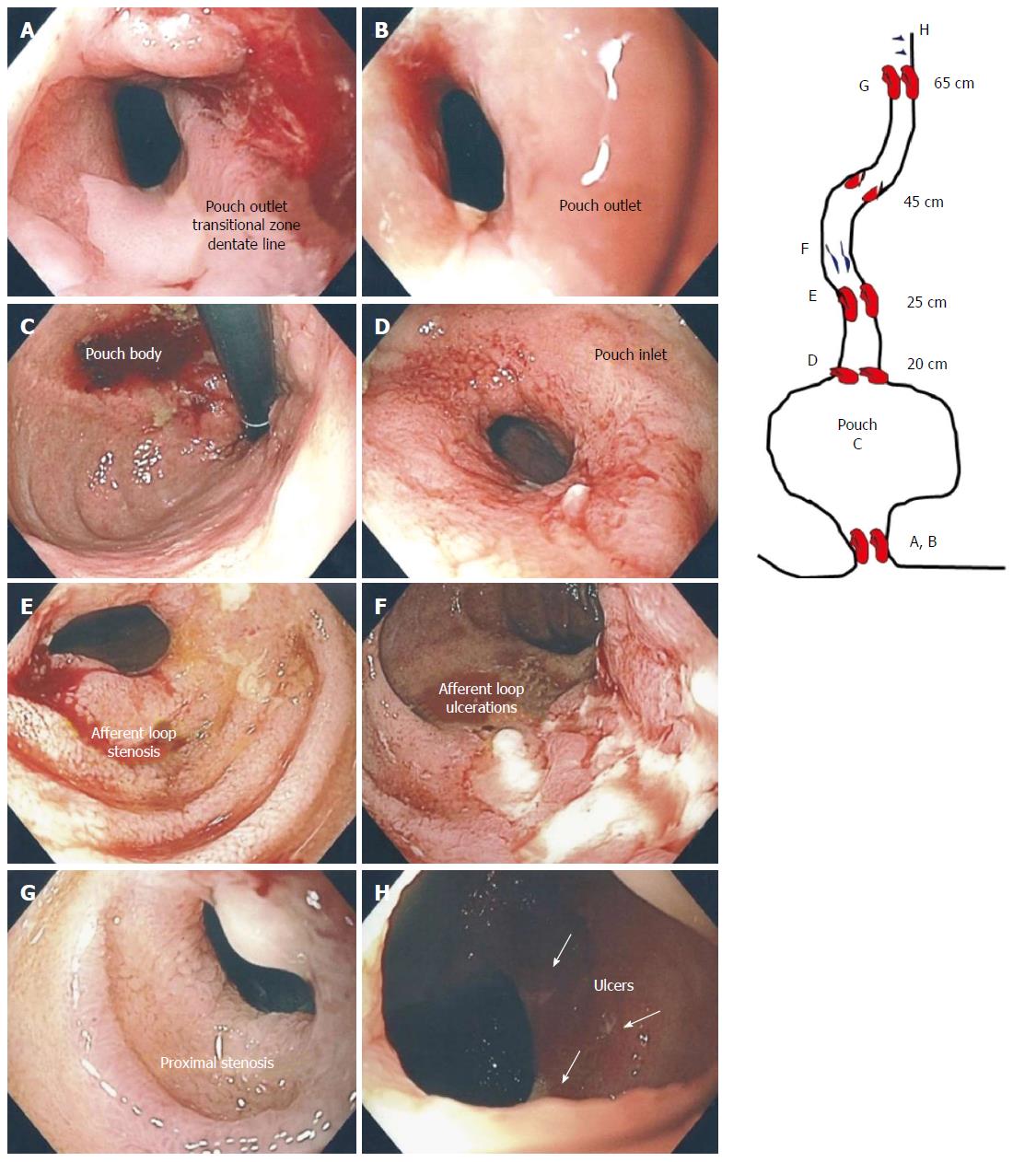
Figure 5 Crohn’s ileo-pouchitis.
Stenosis of the pouch outlet (A, B), normal appearing mucosa of the pouch (C), stenosis of the pouch inlet (D), stenosis of the afferent limb at 25 cm (E), linear deep ulcerations in the ileum (F), proximal stenosis of the ileum at 65 cm (G) and ulcers more proximally (H).
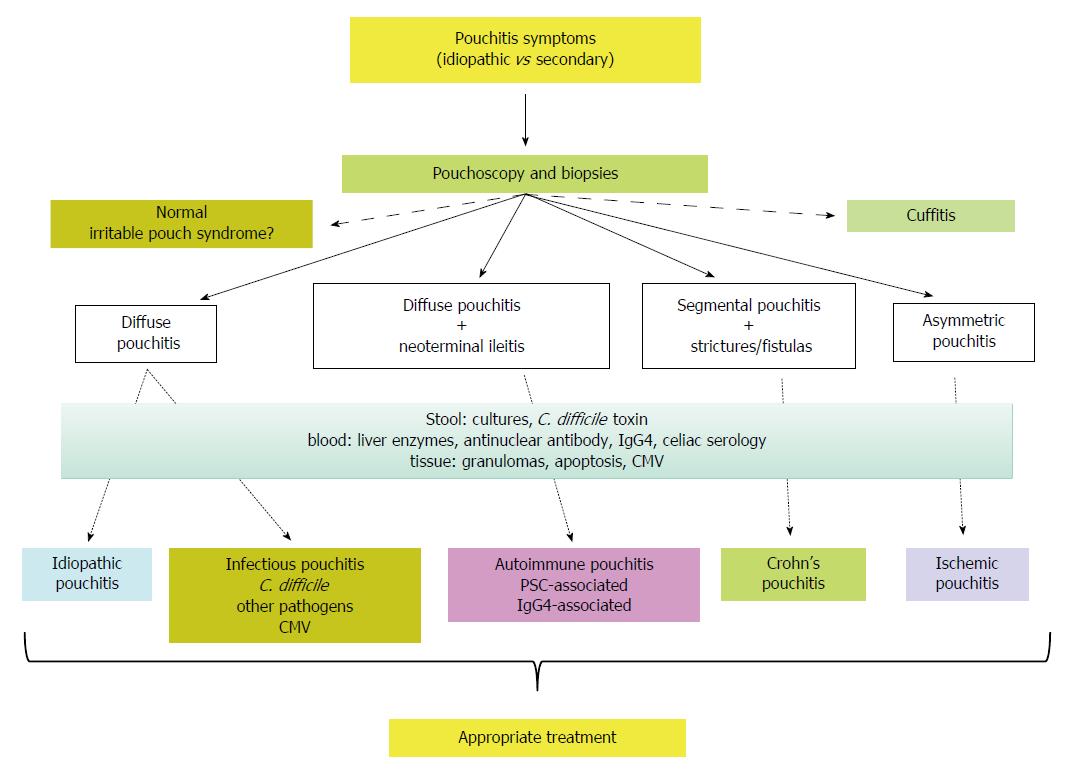
Figure 6 Pouchitis diagnostic algorithm (adapted and modified from Shen[15]).
C. difficile: Clostridium difficile.
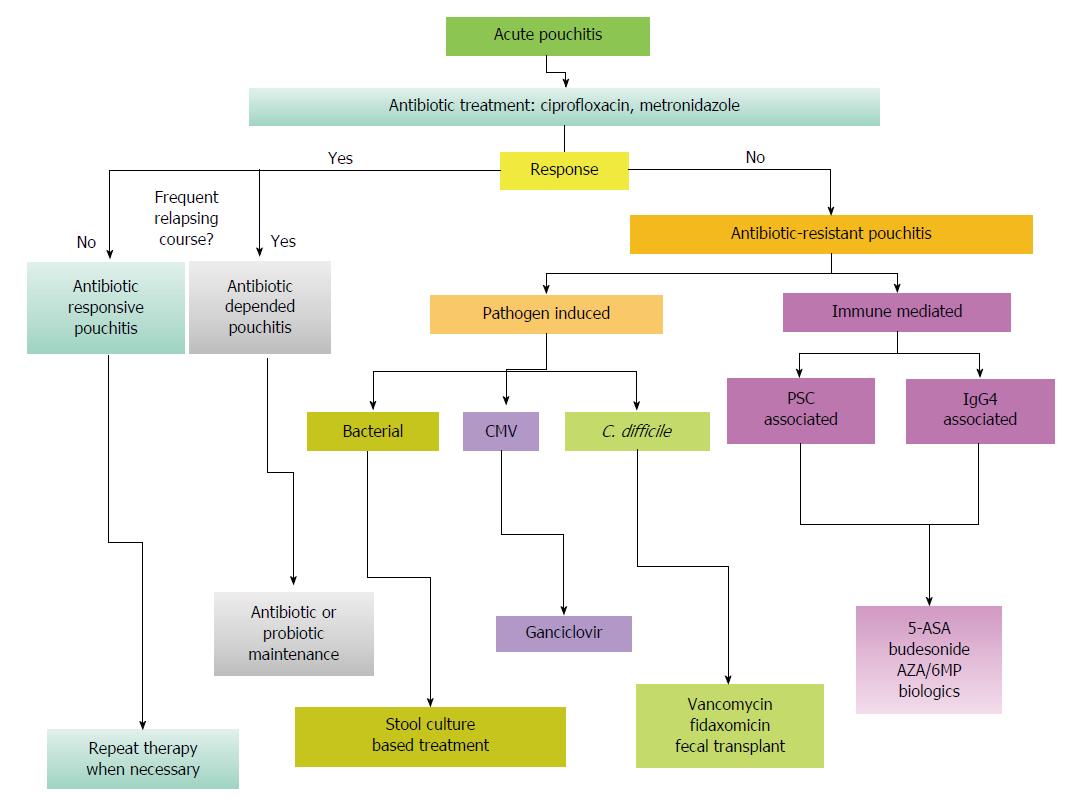
Figure 7 Pouchitis treatment algorithm (adapted and modified from Shen et al[15]).
C. difficile: Clostridium difficile.
- Citation: Zezos P, Saibil F. Inflammatory pouch disease: The spectrum of pouchitis. World J Gastroenterol 2015; 21(29): 8739-8752
- URL: https://www.wjgnet.com/1007-9327/full/v21/i29/8739.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i29.8739