Copyright
©2014 Baishideng Publishing Group Co.
World J Gastroenterol. Mar 7, 2014; 20(9): 2343-2351
Published online Mar 7, 2014. doi: 10.3748/wjg.v20.i9.2343
Published online Mar 7, 2014. doi: 10.3748/wjg.v20.i9.2343
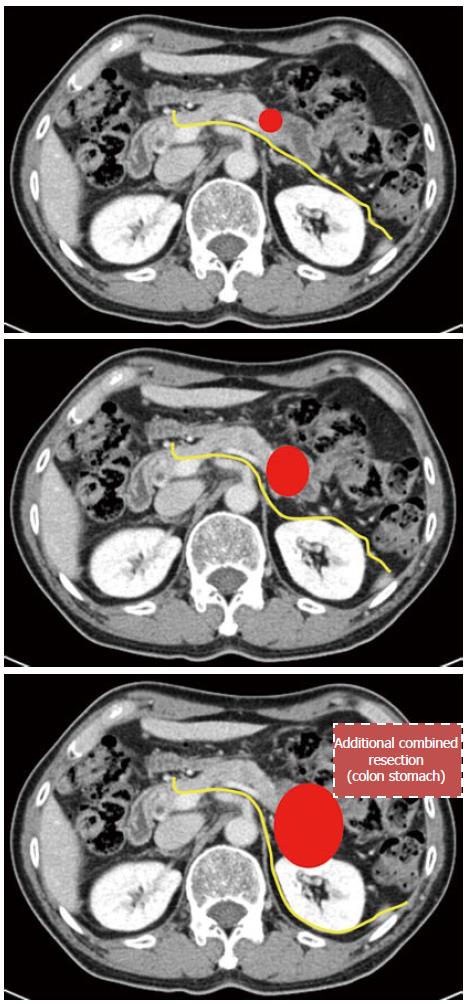
Figure 1 Mode of radical antegrade modular pancreatosplenectomy.
A: Anterior radical antegrade modular pancreatosplenectomy (RAMPS); B: Posterior RAMPS 1; C: Posterior RAMPS 2. Dissection plane (yellow line) should be changed for clear tangential margin a ccording to tumor condition (red circle).
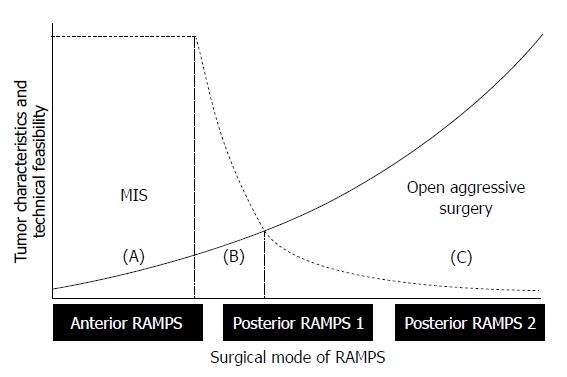
Figure 2 Determining the extent of minimally invasive radical antegrade modular pancreatosplenectomy.
The dotted line shows the technical feasibility of bloodless and margin-negative radical antegrade modular pancreatosplenectomy (RAMPS) by a minimally invasive approach, and the solid line represents the biological aggressiveness of tumors, according to the appropriate mode of RAMPS for margin-negative resection. Tentatively, minimally invasive anterior RAMPS is thought to represent a generally acceptable surgical extent for bloodless and margin-negative resections. Oncologically safe posterior RAMPS 1 and 2 might be difficult to perform using a minimally invasive approach. Note the marginal zone of (B). Only a few expert laparoscopic surgeons can be fully responsible for this region. Future directions include widening the area of (B) by means of technical evolution (shifting of the dotted line to the left) and improving early tumor detection (attenuating the slope of solid line). MIS: Minimally invasive surgery.
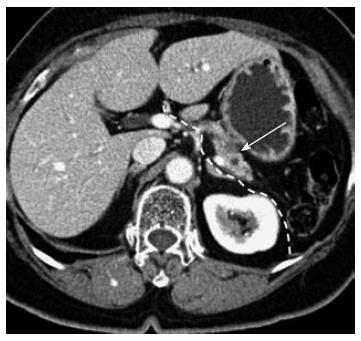
Figure 3 Potential indication for minimally invasive anterior radical antegrade modular pancreatosplenectomy.
A 76-year-old female. A relatively pancreas-confined low density mass lesion is noted (arrow). The dotted white line indicates the dissection plane for minimally invasive anterior radical antegrade modular pancreatosplenectomy (RAMPS). The intact fascia layer between the pancreas and left adrenal gland/kidney can facilitate posterior margin clearance when removing the surgical specimen. The tumor is separated from the origin of the splenic artery, necessary for safe vascular control by introducing a minimally invasive technique. The patient underwent laparoscopic anterior RAMPS and has been followed for more than 1 year without evidence of tumor recurrence.
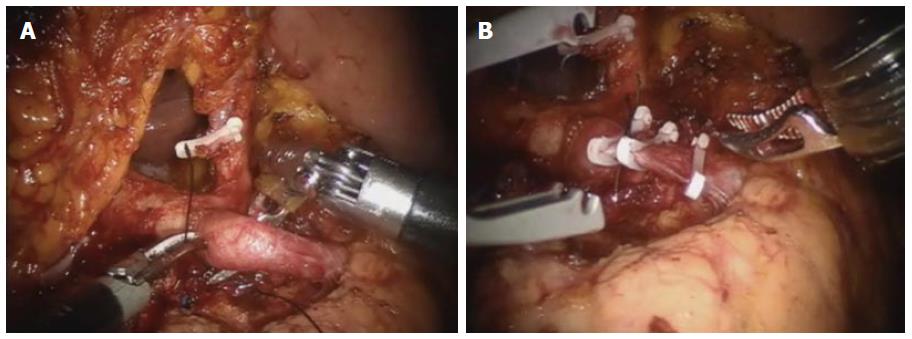
Figure 4 Adequate distance between celiac axis and tumor.
Robotic anterior radical antegrade modular pancreatosplenectomy. The origin of the splenic artery is isolated (A) and ligated (B) by the robotic surgical system. For technically and oncologically safe minimally invasive vascular control, some cancer-free space is extremely necessary.
- Citation: Kang CM, Lee SH, Lee WJ. Minimally invasive radical pancreatectomy for left-sided pancreatic cancer: Current status and future perspectives. World J Gastroenterol 2014; 20(9): 2343-2351
- URL: https://www.wjgnet.com/1007-9327/full/v20/i9/2343.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i9.2343