Copyright
©2014 Baishideng Publishing Group Co.
World J Gastroenterol. Mar 7, 2014; 20(9): 2255-2266
Published online Mar 7, 2014. doi: 10.3748/wjg.v20.i9.2255
Published online Mar 7, 2014. doi: 10.3748/wjg.v20.i9.2255
Figure 1 Computed tomography of locally advanced pancreatic cancer.
Encasement is defined as greater than 180-degree involvement of the major vessels. A: Celiac axis is encased by locally advanced pancreatic cancer (arrow); B: Superior mesenteric artery and the replaced right hepatic artery are encased by pancreatic cancer (arrow); C: The portal vein and its confluence with splenic vein are encased by pancreatic cancer (arrow).
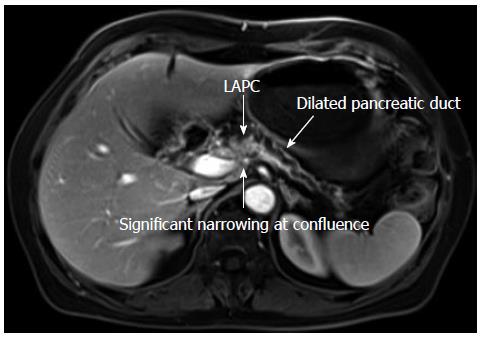
Figure 2 Magnetic resonance imaging of locally advanced pancreas cancer with vascular invasion and dilated pancreatic duct.
LAPC: Locally advanced pancreatic cancer.
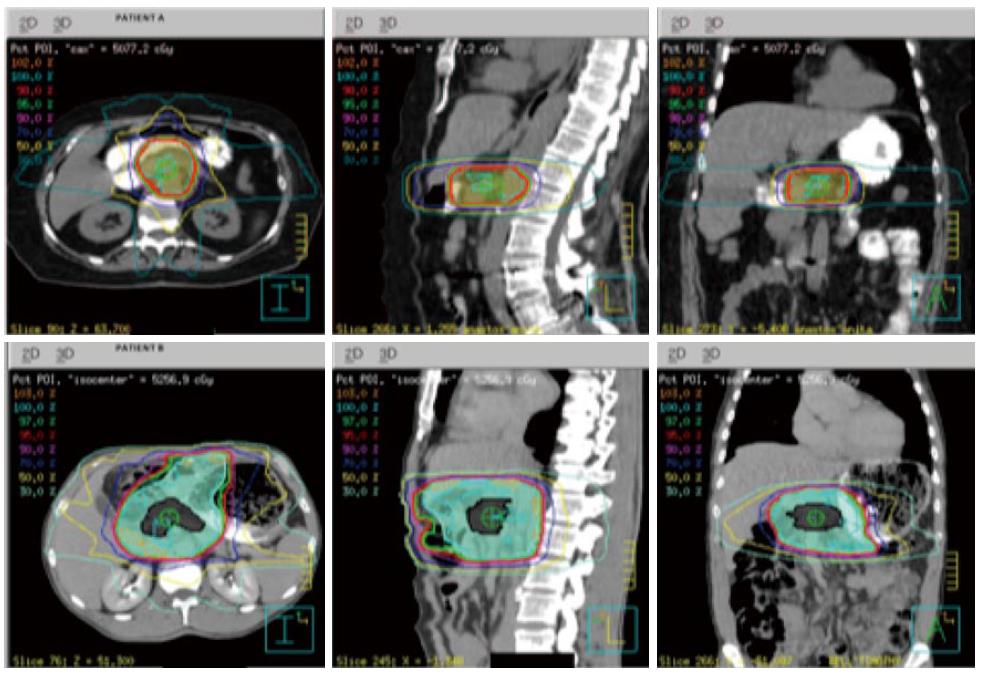
Figure 3 Depiction of stereotactic body radiation plan using computed tomography.
Typically the tumor is expanded 2-3 mm to account for set up error microscopic extension and set-up error planning treatment volume. In the lower panel, (patient b) this represents a plan integrating intensity modulated radiation therapy (IMRT) where the tumor is expanded 1-3 cm to cover the tumor and peripancreatic lymph nodes. Stereotactic body radiation is often delivered over 1-5 d without chemotherapy. IMRT is delivered over 5-6 wk with concurrent chemotherapy.
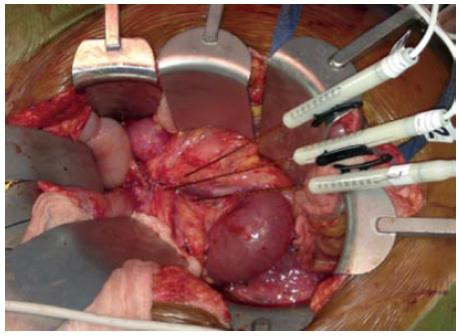
Figure 4 An intraoperative image of in situ irreversible electroporation being used in a patient with locally advanced pancreatic cancer.
Three probes are placed around the tumor which is encasing the superior mesenteric vein causing complete occlusion plus superior mesenteric artery involvement.
Figure 5 This is the representative base unit and generator for irreversible electroporation, manufactured by AngioDynamics, Latham, NY.
- Citation: He J, Page AJ, Weiss M, Wolfgang CL, Herman JM, Pawlik TM. Management of borderline and locally advanced pancreatic cancer: Where do we stand? World J Gastroenterol 2014; 20(9): 2255-2266
- URL: https://www.wjgnet.com/1007-9327/full/v20/i9/2255.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i9.2255