Copyright
©2014 Baishideng Publishing Group Co.
World J Gastroenterol. Feb 21, 2014; 20(7): 1724-1745
Published online Feb 21, 2014. doi: 10.3748/wjg.v20.i7.1724
Published online Feb 21, 2014. doi: 10.3748/wjg.v20.i7.1724
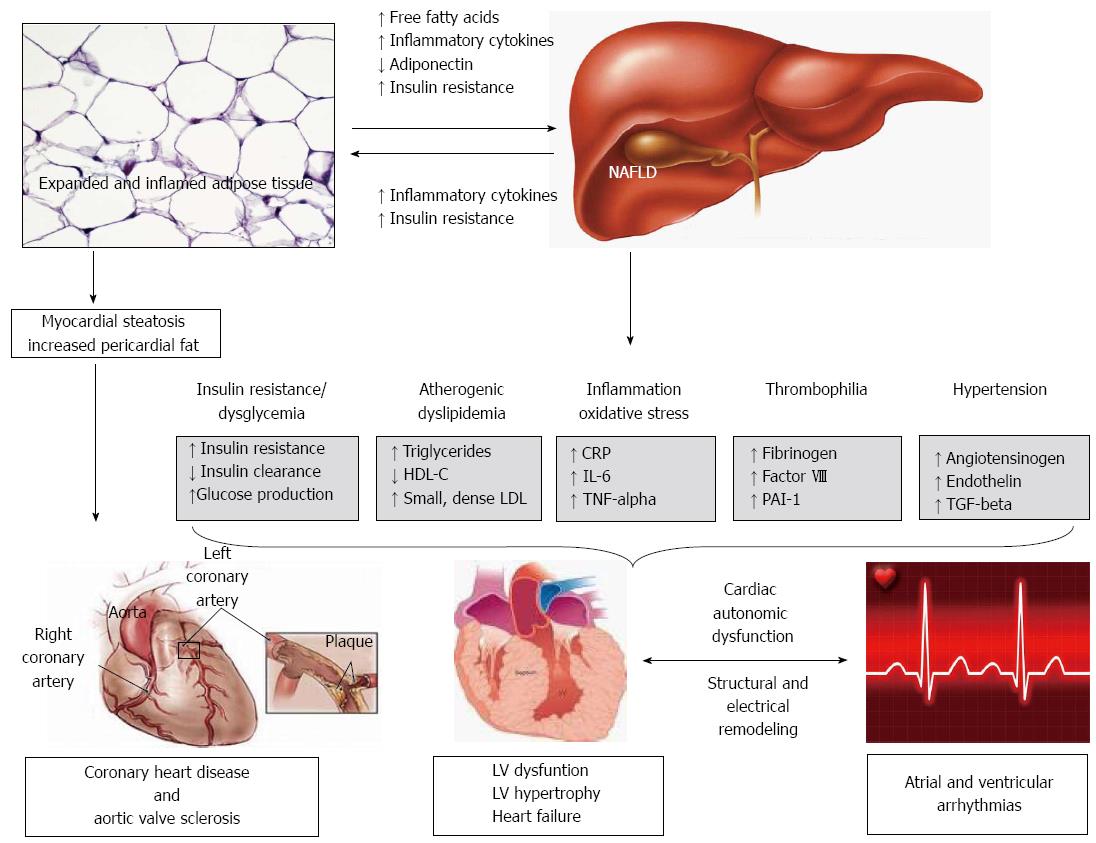
Figure 1 Possible mechanisms leading to cardiac and arrhythmogenic complications in non-alcoholic fatty liver disease.
The close and complex inter-relationships among non-alcoholic fatty liver disease (NAFLD), visceral obesity and insulin resistance make it extremely difficult to dissect out the specific role of the liver and the underlying mechanisms responsible for the association between NAFLD and the risk of developing coronary heart disease (CHD), aortic valve sclerosis, left ventricular (LV) dysfunction/hypertrophy and arrhythmias. NAFLD might be associated with such complications either as a consequence of shared cardiometabolic risk factors and co-morbidities or as a marker of ectopic fat accumulation in other organs. For instance, myocardial steatosis and increased pericardial fat volume might exert local adverse effects that result in functional and structural derangements of the myocardium. Such myocardial remodelling will likely also result in pro-arrhythmogenic effects. The occurrence of cardiac arrhythmias is likely facilitated in remodeled heart by (local) pro-inflammatory cytokines, chemokines and concurrent cardiac autonomic dysfunction occurring on this dysmetabolic milieu. However, in this dangerous scenario, which may potentially account for premature CHD and increased risk of arrhythmias, NAFLD seems to be not simply a marker of cardiac and arrhythmogenic complications but also may play a part in their pathogenesis possibly via atherogenic dyslipidemia and the hepatic secretion of several pathogenic mediators into the bloodstream. HDL-C: High-density lipoprotein cholesterol; LDL: Low-density lipoprotein; CRP: C reactive protein; IL: Interleukin; TNF: Tumor necrosis factor; PAI-1: Plasminogen activator inhibitor-1; TGF: Transforming growth factor.
- Citation: Ballestri S, Lonardo A, Bonapace S, Byrne CD, Loria P, Targher G. Risk of cardiovascular, cardiac and arrhythmic complications in patients with non-alcoholic fatty liver disease. World J Gastroenterol 2014; 20(7): 1724-1745
- URL: https://www.wjgnet.com/1007-9327/full/v20/i7/1724.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i7.1724