Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. Oct 28, 2014; 20(40): 14706-14716
Published online Oct 28, 2014. doi: 10.3748/wjg.v20.i40.14706
Published online Oct 28, 2014. doi: 10.3748/wjg.v20.i40.14706
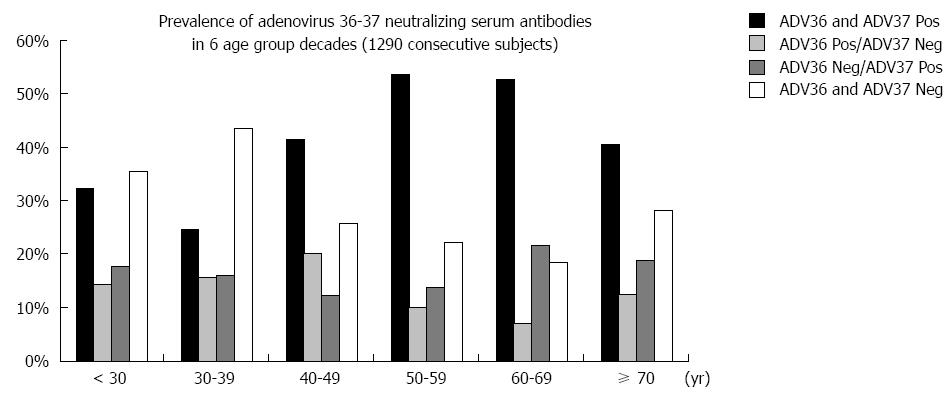
Figure 1 ADV36 seropositivity prevalence increases with ageing (20-29, 30-39, 40-49, 50-59, 60-69 and ≥ 70 years) considering consecutive adult age decades in our population.
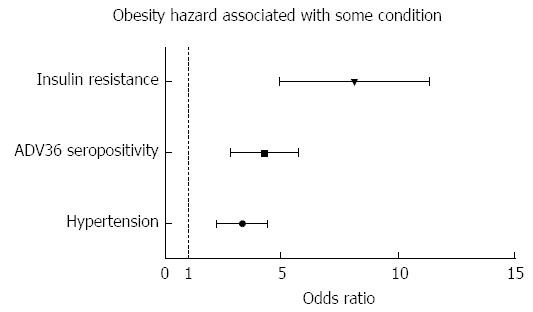
Figure 2 Odds ratios show an increased hazard of obesity associated with ADV36 seropositivity (OR = 6.
879; 95%CI: 3.316-14.274), essential hypertension (OR = 2.977; 95%CI: 1.625-5.451) and insulin resistance (OR = 3.792; 95%CI: 2.052-7.006).
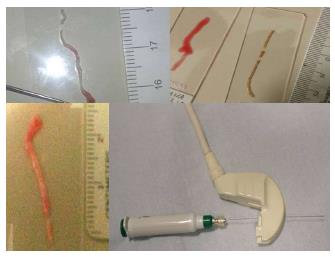
Figure 3 Convex ultrasound transducer with a central hole for allowing co-axial biopsy and four different specimens of liver fine needle aspirate biopsy in fatty liver performed with 20 G needle.
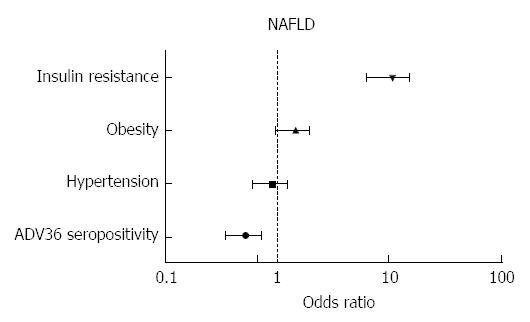
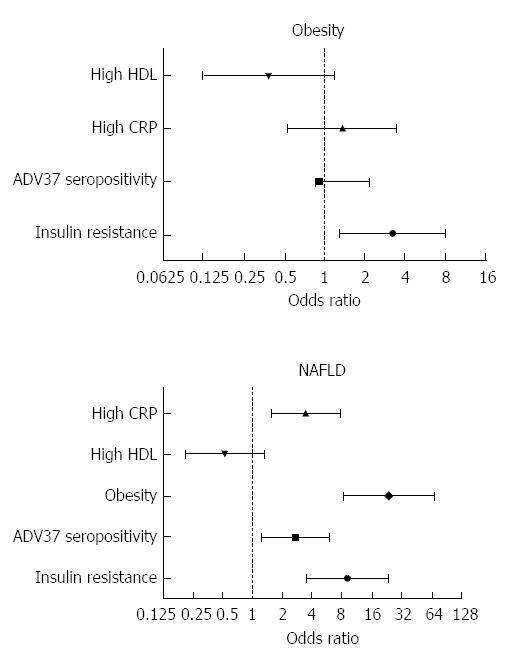
Figure 4 Odds ratio: Higher hazard of non-alcoholic fatty liver disease is associated with insulin resistance and obesity, and a lower non-alcoholic fatty liver disease risk is associated with ADV36 seropositivity.
NAFLD: Nonalcoholic fatty liver disease.
Figure 5 Odds ratio.
Increased risk of obesity (top) is associated with greater insulin resistance, C-reactive protein, and ADV37 seropositivity (Ad37+), whereas higher high-density lipoprotein cholesterol is associated with lower prevalence of obesity. A more consistent association of ADV37+, greater insulin resistance, C-reactive protein (CRP), and obesity was observed with non-alcoholic fatty liver disease (NAFLD) (bottom), whereas higher high-density lipoprotein (HDL) cholesterol was associated with a lower prevalence of NAFLD. No sex difference was found. This behavior is different, if not opposite, of that of ADV36.
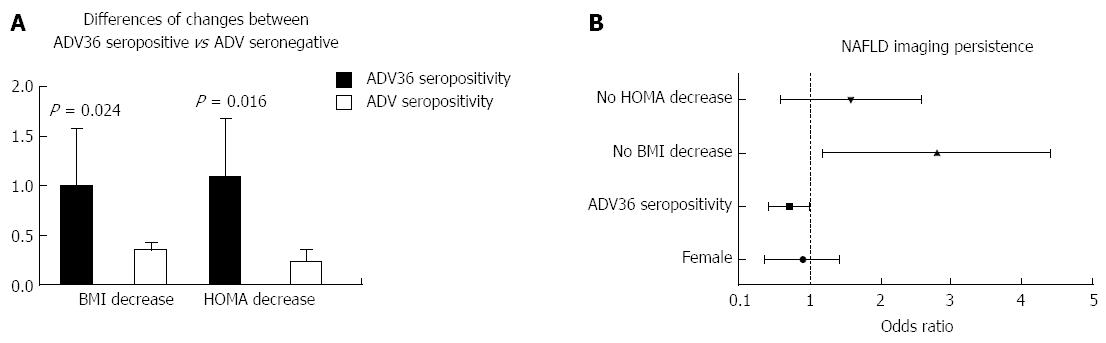
Figure 6 After a comprehensive nutritional and lifestyle intervention, the improvement is more relevant in ADV36 seropositive than in ADV36 seronegative non-alcoholic fatty liver disease patients: a greater decrease of insulin resistance (homeostasis model assessment) and of overweight (body mass index) was achieved in ADV seropositive non-alcoholic fatty liver disease patients (A) and the odds of bright liver persistence is associated with lack of insulin resistance (homeostasis model assessment) and body weight (body mass index) decrease, while a relevant association with improvement, i.
e., bright liver disappearance, is observed in ADV36 seropositive non-alcoholic fatty liver disease patients (B). BMI: Body mass index; HOMA: Homeostasis model assessment; NAFLD: Non-alcoholic fatty liver disease.
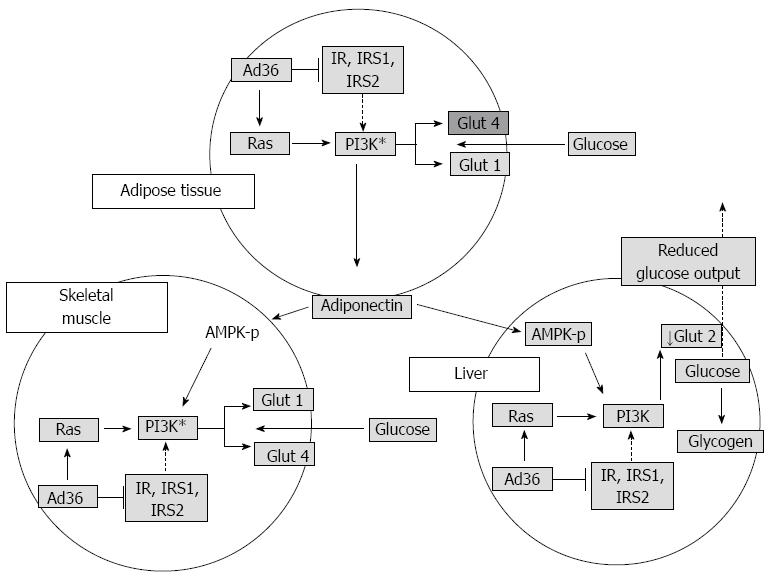
Figure 7 Working model to explain the antidiabetic effect of ADV36.
Overall, data from suggest that, in adipose tissue, skeletal muscle, and liver of mice, ADV36 downregulates insulin signaling yet upregulates the Ras-PI3K pathway, which upregulates Glut1 and Glut4 in skeletal muscle and adipose tissue and downregulates Glut2 in liver. Furthermore, ADV36 increases adiponectin, which may activate AMPK. Collectively, this leads to greater glucose uptake by adipose tissue and skeletal muscle and reduces hepatic glucose release, which may contribute to ADV36-induced improvement in systemic glycemic control[53]. Modified from Krishnapuram et al[54].
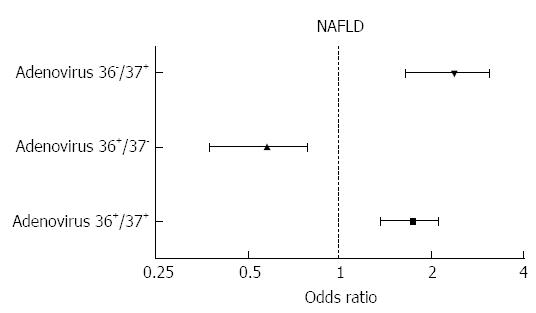
Figure 8 Compound ADV36/ADV37 seropositivity is associated with a risk profile more similar to ADV37 seropositivity, whose effect is not blunted by ADV36 seropositivity.
NAFLD: Non-alcoholic fatty liver disease.
- Citation: Trovato FM, Catalano D, Garozzo A, Martines GF, Pirri C, Trovato GM. ADV36 adipogenic adenovirus in human liver disease. World J Gastroenterol 2014; 20(40): 14706-14716
- URL: https://www.wjgnet.com/1007-9327/full/v20/i40/14706.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i40.14706