Copyright
©2014 Baishideng Publishing Group Co.
World J Gastroenterol. Mar 21, 2014; 20(11): 2825-2838
Published online Mar 21, 2014. doi: 10.3748/wjg.v20.i11.2825
Published online Mar 21, 2014. doi: 10.3748/wjg.v20.i11.2825
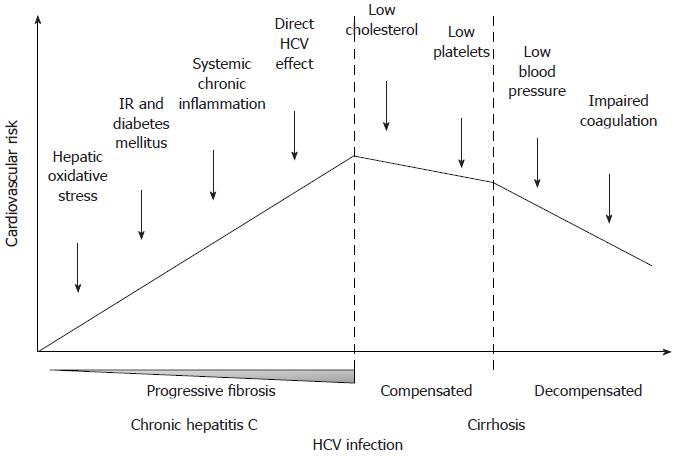
Figure 1 Hypothetical trend of cardiovascular risk during the natural history of hepatitis C virus infection, from chronic hepatitis to decompensated cirrhosis.
IR: Insulin resistance; HCV: Hepatitis C virus.
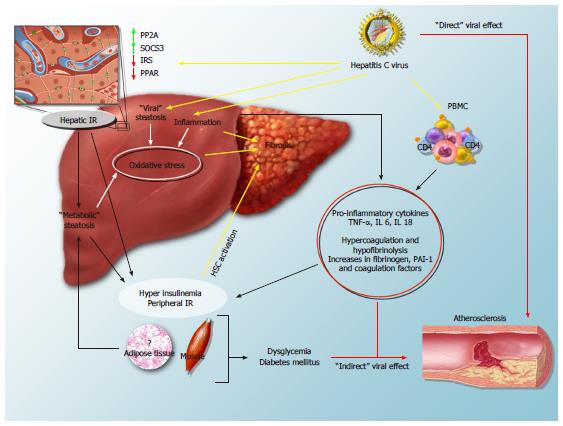
Figure 2 Mechanisms of hepatitis C virus-induced insulin resistance and steatosis and their impact on the progression of fibrosis and cardiovascular disease.
In the hepatocyte, the virus interferes with insulin signalling, leads to overexpression of protein phosphatase 2A (PP2A) and suppressor of cytokine signalling-3 (SOCS-3), and down-regulates the expression of peroxisome proliferator activated receptors (PPAR) and of insulin receptor substrate (IRS): all these mechanisms lead to hepatic insulin resistance (IR). By inducing hepatic injury and activating peripheral blood mononuclear cells (PBMC), HCV increases circulating levels of proinflammatory cytokines, such as tumor necrosis factor-α (TNF-α), interleukin-6 and -18 (IL-6 and IL-18), and leads to peripheral IR and hyperinsulinemia. “Viral” and “metabolic” steatosis, together with the direct stimulus of increased insulin levels on hepatic stellate cells (HSCs), likely stimulate the progression of fibrosis. Furthermore, systemic inflammation, the procoagulative state and direct viral effects may contribute to the atherogenic process.
- Citation: Vespasiani-Gentilucci U, Gallo P, Vincentis AD, Galati G, Picardi A. Hepatitis C virus and metabolic disorder interactions towards liver damage and atherosclerosis. World J Gastroenterol 2014; 20(11): 2825-2838
- URL: https://www.wjgnet.com/1007-9327/full/v20/i11/2825.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i11.2825