Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Mar 7, 2013; 19(9): 1451-1457
Published online Mar 7, 2013. doi: 10.3748/wjg.v19.i9.1451
Published online Mar 7, 2013. doi: 10.3748/wjg.v19.i9.1451
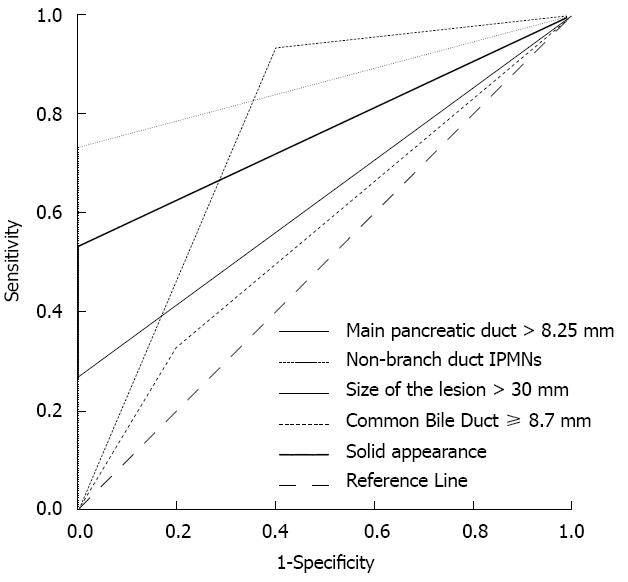
Figure 1 Characteristics of computed tomography/magnetic resonance imaging.
Receiver operating characteristic analysis showed that non-branch duct intraductal papillary mucinous neoplasms (IPMNs), lesion size > 30 mm and a solid component appearance in the lesion had great significance for predicting pancreatic resection, and the area under the curve reached 0.76 (P = 0.012, 95%CI: 0.569-0.964), 0.867 (P = 0.001, 95%CI: 0.758-0.976) and 0.76 (P < 0.01, 95%CI: 0.623-0.910), respectively.
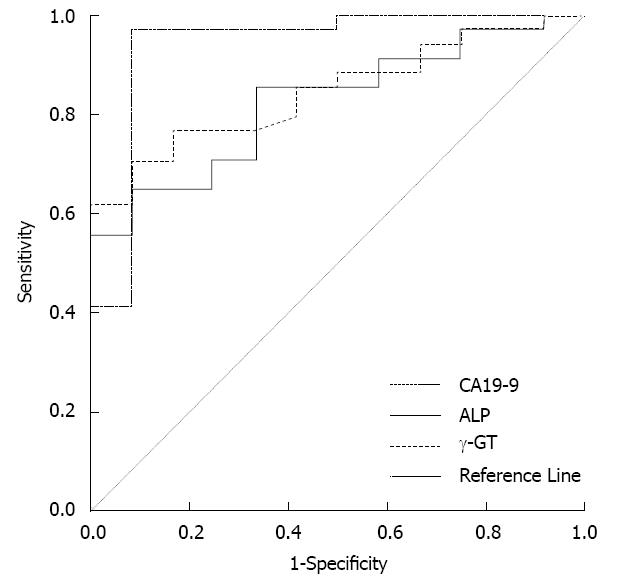
Figure 2 The predictors of malignant intraductal papillary mucinous neoplasms.
Receiver operating characteristic analysis showed that γ-GT > 50 U/L, alkaline phosphatase (ALP) > 115 U/L or carbohydrate antigen 19-9 (CA19-9) > 37 U/mL effectively predicted malignant intraductal papillary mucinous neoplasms. However, the area under the curve for CA19-9 > 37 U/mL was the largest among the three indices and reached 0.939 (P < 0.01, 95%CI: 0.843-1.035).
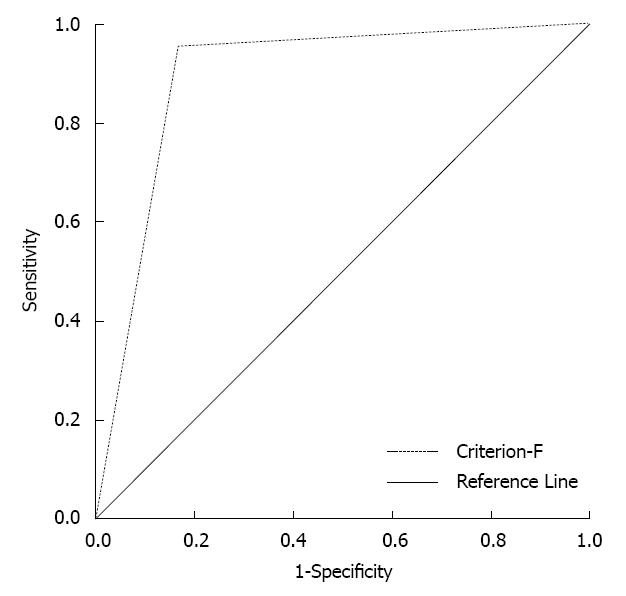
Figure 3 The predictive value of the combination of carbohydrate antigen 19-9 and computed tomography/magnetic resonance imaging (criterion-F).
The area under the curve by receiver operating characteristic analysis reached 0.893 (P < 0.01, 95%CI: 0.763-1.023).
- Citation: Xu B, Ding WX, Jin DY, Wang DS, Lou WH. Decision making for pancreatic resection in patients with intraductal papillary mucinous neoplasms. World J Gastroenterol 2013; 19(9): 1451-1457
- URL: https://www.wjgnet.com/1007-9327/full/v19/i9/1451.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i9.1451