Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Aug 14, 2013; 19(30): 5000-5005
Published online Aug 14, 2013. doi: 10.3748/wjg.v19.i30.5000
Published online Aug 14, 2013. doi: 10.3748/wjg.v19.i30.5000
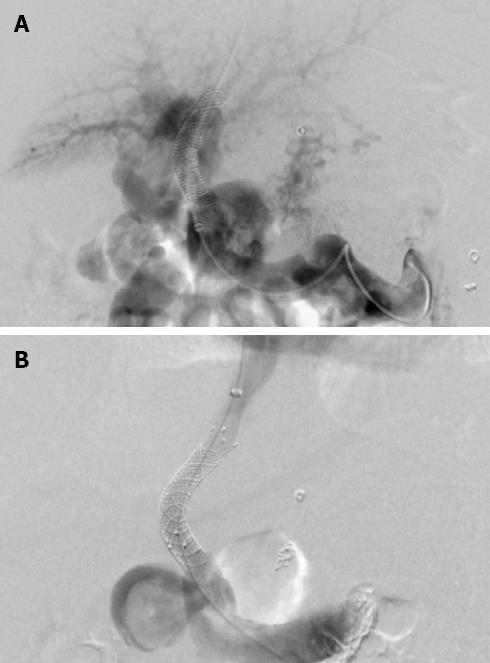
Figure 1 Portal venograms in a 52-year-old woman with hepatitis B cirrhosis who was treated with transjugular intrahepatic portosystemic shunt for recurrent variceal bleeding.
A: Portography after crossing the previous shunt shows a patent splenic vein and the occluded main portal vein with cavernous transformation; B: After implantation with a Fluency stent, the portosystemic pressure gradient was reduced from 31 to 11 mmHg.
Figure 2 Portal venograms in a 45-year-old man with hepatitis B cirrhosis who had undergone transjugular intrahepatic portosystemic shunt for repeated variceal bleeding.
A: The anteroposterior portal venogram obtained 5 mo after the initial transjugular intrahepatic portosystemic shunt procedure shows the complete occlusion of the stent and opacification of a massive spontaneous splenorenal shunt; B: Embolization of the splenorenal shunt was performed to maintain sufficient portal flow to keep the stent open. The portal venogram after Wallgraft stent placement reveals a wide patent shunt. The portosystemic pressure gradient decreased from 37 to 10 mmHg.
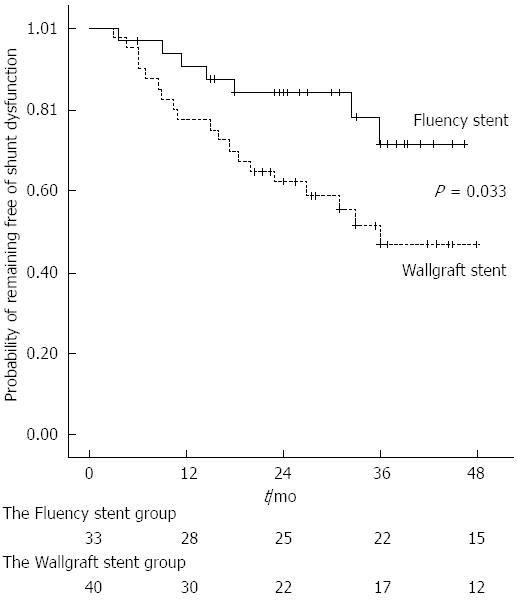
Figure 3 The probability of remaining free of shunt dysfunction.
-
Citation: Luo XF, Nie L, Wang Z, Tsauo J, Liu LJ, Yu Y, Zhou B, Tang CW, Li X. Stent-grafts for the treatment of TIPS dysfunction: Fluency stent
vs Wallgraft stent. World J Gastroenterol 2013; 19(30): 5000-5005 - URL: https://www.wjgnet.com/1007-9327/full/v19/i30/5000.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i30.5000