Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Jul 28, 2013; 19(28): 4537-4544
Published online Jul 28, 2013. doi: 10.3748/wjg.v19.i28.4537
Published online Jul 28, 2013. doi: 10.3748/wjg.v19.i28.4537
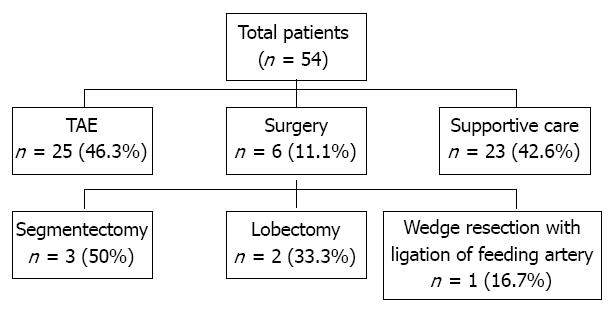
Figure 1 Flow diagram showing the treatment of 54 patients.
Of the 54 patients enrolled, 6 (11.1%) underwent surgery and 25 (46.3%) transarterial embolization (TAE), and the remaining 23 (42.6%) patients received supportive care without hemostatic intervention.
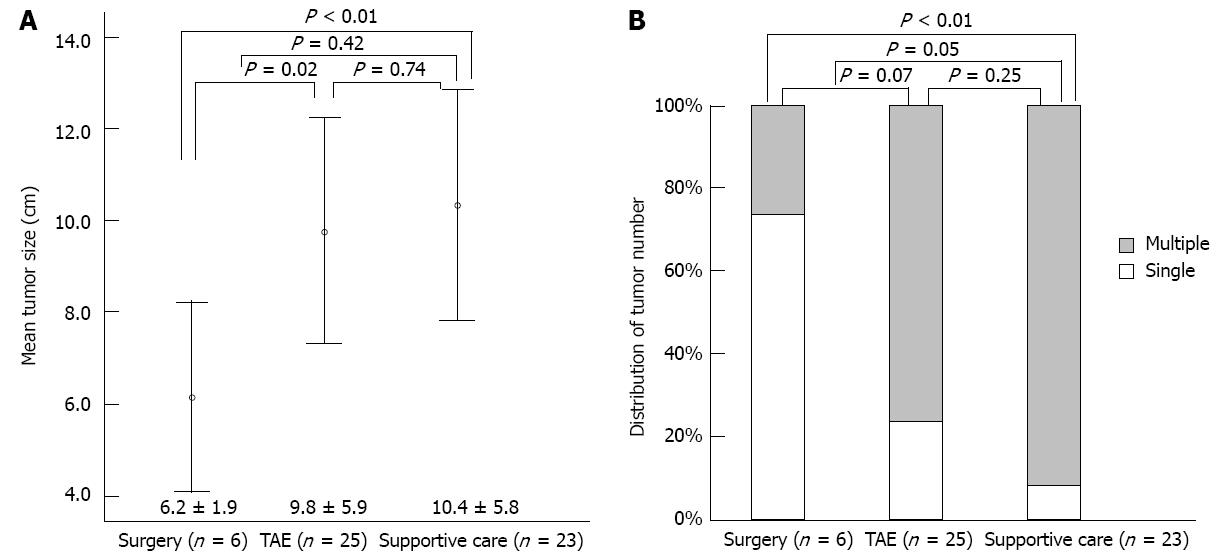
Figure 2 Comparison of clinical parameters in the three treatment groups.
A: Mean tumor size was significantly smaller in the surgical group than in the transarterial embolization (TAE) (P = 0.02) or supportive care (P < 0.01) groups; B: The single tumor rate was significantly higher in the surgical group than in the supportive care group (P < 0.01).
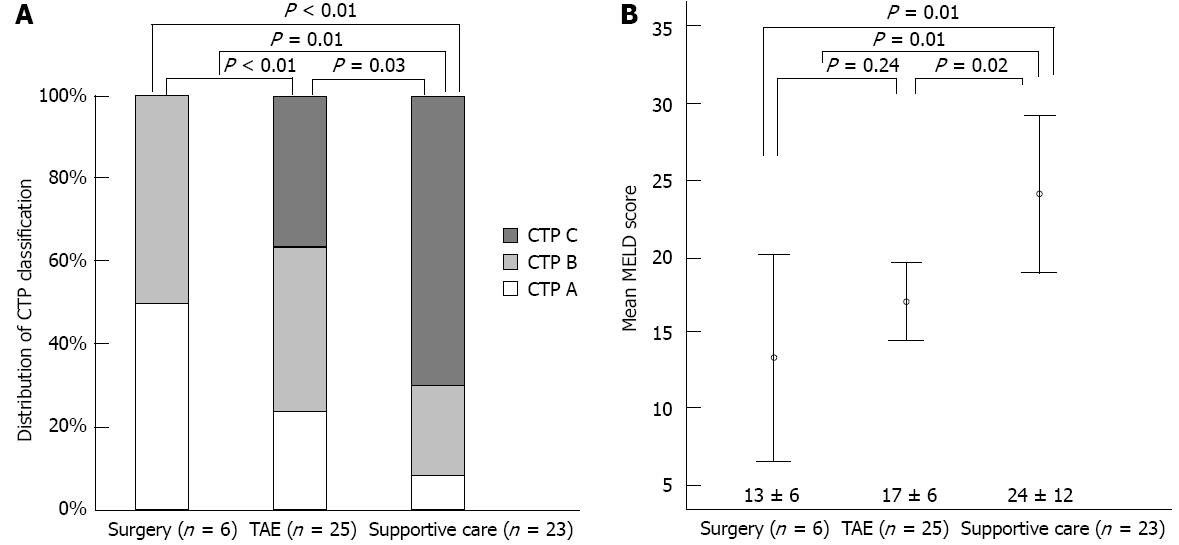
Figure 3 Comparison of Child-Turcotte-Pugh and Model for End-stage Liver Disease scores in the three treatment groups.
A: The surgical group had better reserve hepatic function [Child-Turcotte-Pugh (CTP) class] than the other two groups (both P < 0.01); B: Mean Model for End-stage Liver Disease (MELD) score was higher in the supportive care group than in the other two groups (both P = 0.01), but was not different in the surgical and transarterial embolization (TAE) groups (P = 0.24).
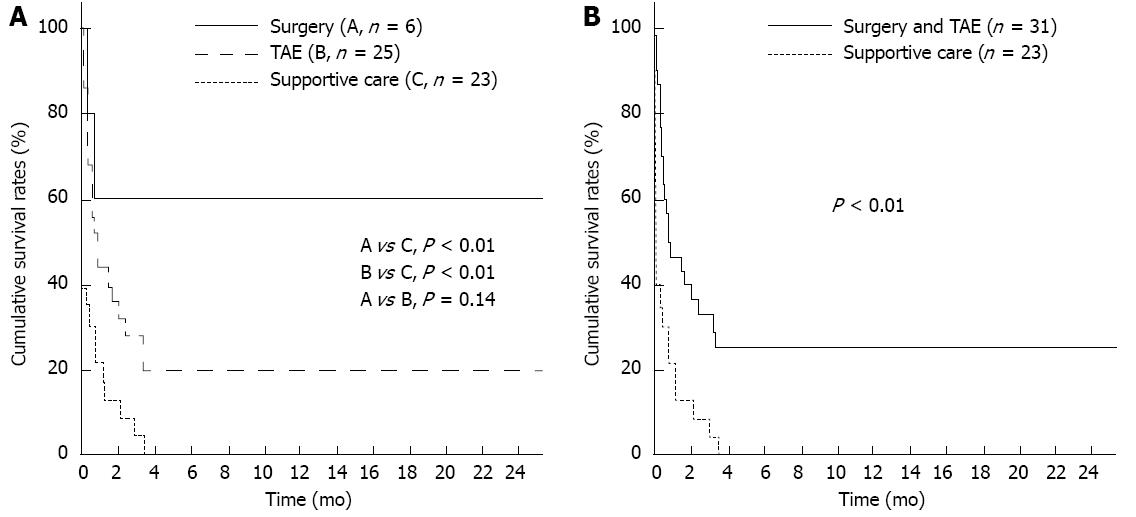
Figure 4 Cumulative overall survival according to treatment types.
A: Cumulative survival rates at 2-, 4- and 6-mo in the surgical group or in the transarterial embolization (TAE) group were significantly higher in the supportive care group (each, P < 0.01); B: Cumulative survival rates at 2-, 4- and 6-mo were significantly higher in the intervention group such as surgery and TAE than in the supportive care group (P < 0.01).
- Citation: Jin YJ, Lee JW, Park SW, Lee JI, Lee DH, Kim YS, Cho SG, Jeon YS, Lee KY, Ahn SI. Survival outcome of patients with spontaneously ruptured hepatocellular carcinoma treated surgically or by transarterial embolization. World J Gastroenterol 2013; 19(28): 4537-4544
- URL: https://www.wjgnet.com/1007-9327/full/v19/i28/4537.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i28.4537