Copyright
©2012 Baishideng Publishing Group Co.
World J Gastroenterol. Sep 21, 2012; 18(35): 4811-4822
Published online Sep 21, 2012. doi: 10.3748/wjg.v18.i35.4811
Published online Sep 21, 2012. doi: 10.3748/wjg.v18.i35.4811
Figure 1 Tetsuo Arakawa, MD, PhD, Dean, Osaka City University Graduate School of Medicine, 1-4-3 Asahi-machi, Abeno-ku, Osaka 545-8585, Japan.
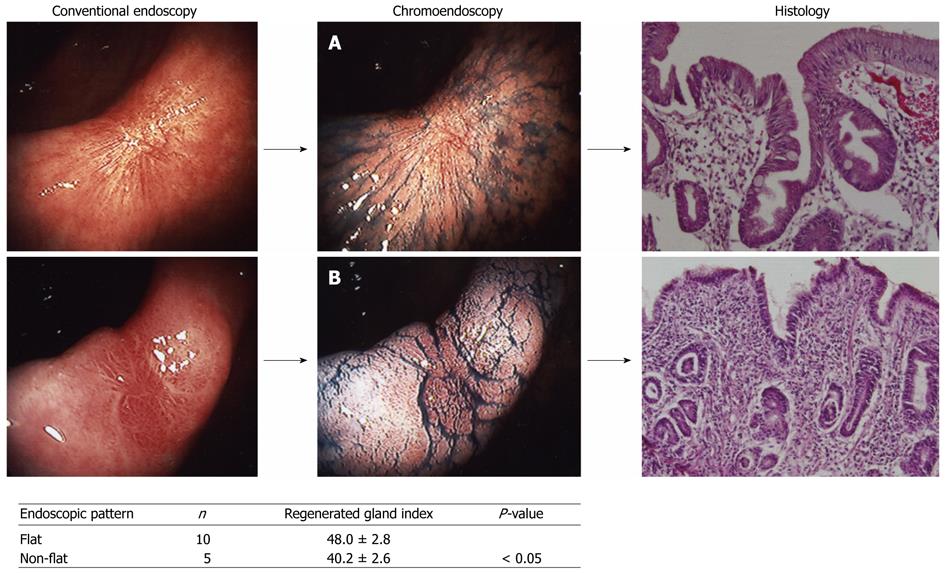
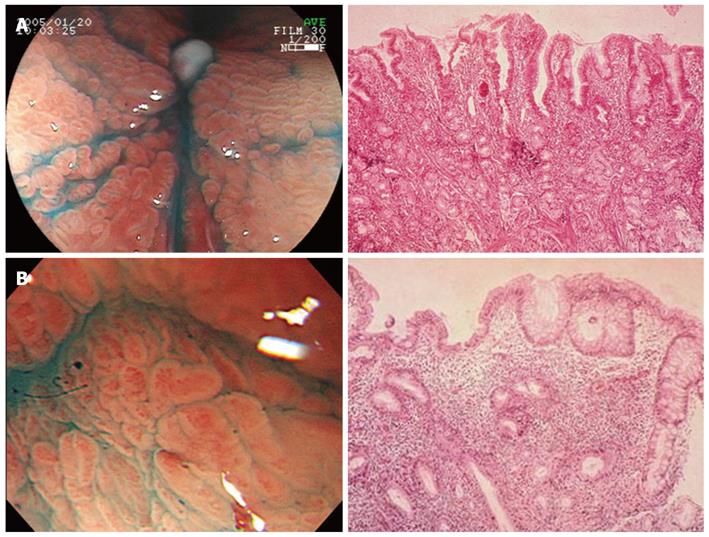
Figure 2 Assessment of endoscopic quality of ulcer healing.
Flat pattern (A) and non-flat pattern (B) are identified by chromoendoscopy, but not by conventional endoscopy. Flat pattern reflects good quality of healing compared to nodular pattern as assessed by histological maturity (Arakawa et al[12] ).
Figure 3 Cumulative remission rates of healed gastric ulcers with flat and non-flat pattern.
The incidence of ulcer recurrence is much higher in the ulcer scar with a non-flat than flat pattern (Nebiki et al[14]).
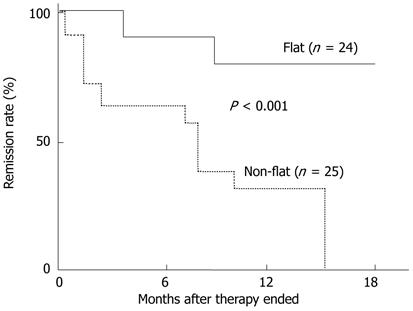
Figure 4 Effect of low-dose indomethacin given during initial period of healing process of gastric ulcer induced by application of acetic acid in rats on cumulative remission rate after healing and on neutrophil infiltration of the interstitial space of the ulcer scar.
Indomethacin treatment enhances neutrophil infiltration and this phenomenon persists even after cessation of this drug. Concomitant administration of 16, 16-dimethyl prostaglandin E2 (PGE2) with indomethacin reverses these effects by indomethacin. A: Cumulative remission rate after healing; B: Infiltration with polymorphonuclear cells during and after healing. Control; indomethacin; indomethacin + 16, 16-dimethyl prostaglandin E2 (Arakawa et al[18]). aP < 0.05 vs control group.
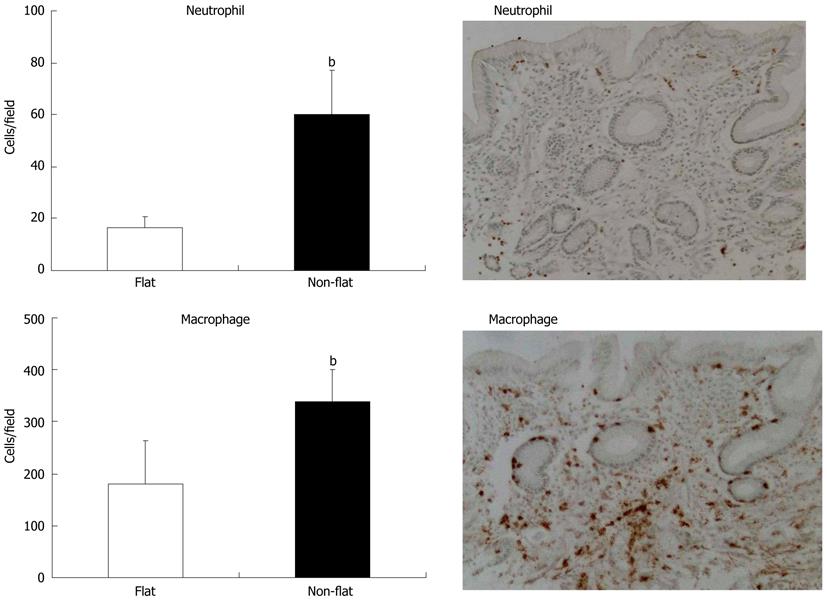
Figure 5 Number of inflammatory cells infiltrating interstitial space of ulcer scar with flat or non-flat pattern assessed by chromoendoscopy in patients with macroscopically healed gastric ulcer.
The number of neutrophils and macrophages is much higher in non-flat than in flat pattern. The number of macrophages is increased five times vs neutrophils in non-flat scar. n = 6, bP < 0.01 vs flat group.
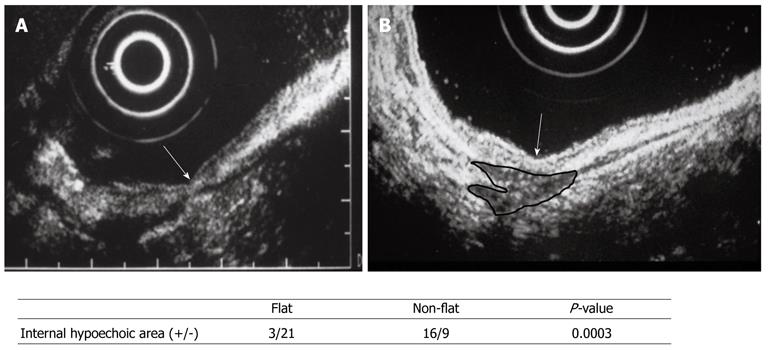
Figure 6 Assessment of interstitial space beneath gastric ulcer scar with endoscopic ultrasonography.
Hypoechoic area (circle of black line) is clearly seen in non-flat scar (B), but not in flat scar (A). Arrow shows a point of ulcer scar (Nebiki et al[14]).
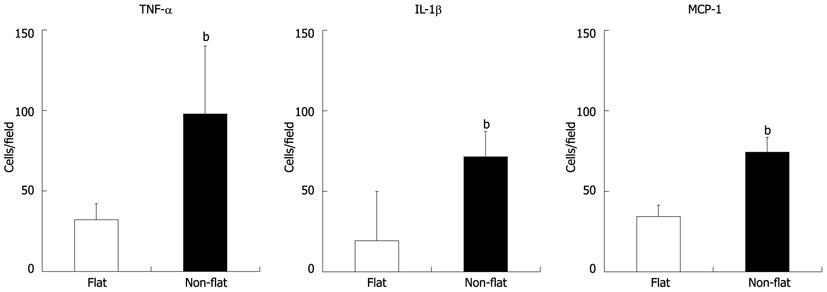
Figure 7 Number of tumor necrosis factor-α-, interleukin-1β-, and monocyte chemotactic protein-1-producing cells in interstitial space of ulcer scar site in patients with gastric ulcer whose ulcer healed with flat vs non-flat pattern assessed by chromoendoscopy.
n = 6, bP < 0.01 vs flat group. TNF-α: Tumor necrosis factor α; IL-1β: Interleukin-1β; MCP-1: Monocyte chemotactic protein-1.
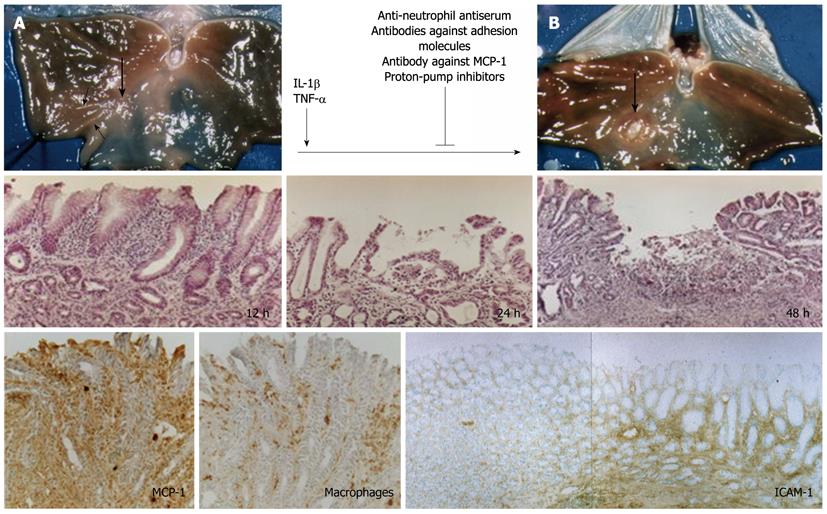
Figure 8 Original rat model of gastric ulcer recurrence.
A: Ulcer scar of acetic-acid-induced gastric ulcer healed spontaneously (big arrow) with fold convergence (small arrows); B: Recurrence of ulcer with white coat at the same site as previous ulcer (big arrow). Interleukin-1β (IL-1β) or tumor necrosis factor α (TNF-α) administered systemically causes recurrence of ulcer macroscopically and histologically. Antineutrophil antiserum, antibodies against adhesion molecules, antibody against monocyte chemotactic protein-1 (MCP-1), or proton-pump inhibitors prevent recurrence. MCP-1 is overexpressed in macrophages in the interstitial space of the ulcer scar site at 12 h after administration of IL-1β or TNF-α. Adhesion molecules are overexpressed only at the ulcer scar site (Watanabe et al[22-24]). ICAM: Intercellular adhesion molecule.
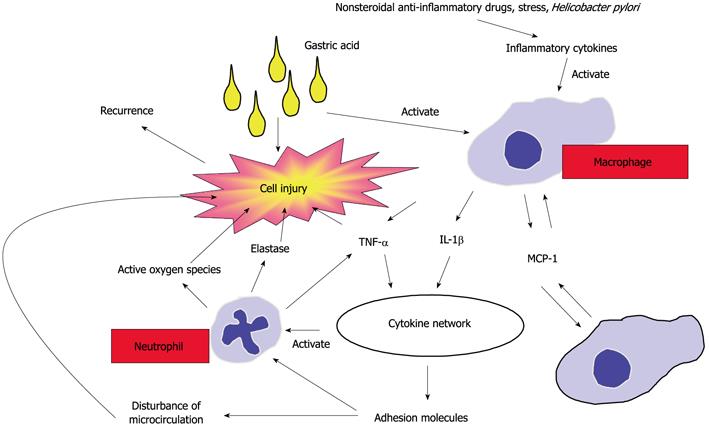
Figure 9 Proposed mechanisms of ulcer recurrence.
Ulcerogenic factors such as nonsteroidal anti-inflammatory drugs, stress, and Helicobacter pylori stimulate the production of inflammatory cytokines, which activate macrophages under acidic conditions. The activated macrophages produce monocyte chemotactic protein-1 (MCP-1), which accumulates other macrophages. These macrophages all produce a large amount of interleukin-1β (IL-1β) and tumor necrosis factor α (TNF-α), which activate the cytokine network, resulting in activation of adhesion molecules and neutrophils. Activated neutrophils migrate from arterioles to the interstitial space and injure the tissue with noxious substances such as reactive oxygen species and elastase produced by themselves together with gastric acid (Arakawa et al[25]).
Figure 10 Magnifying chromoendoscopy shows different findings in flat scar as a fine regular pattern (A) and non-flat scar as coarse irregular pattern (B) compatible with histological findings.
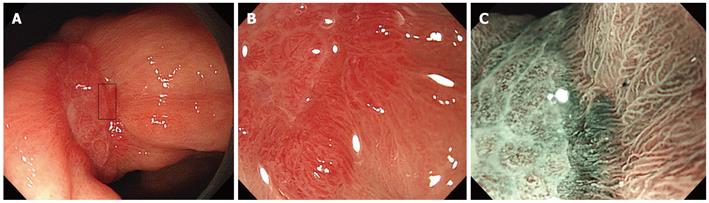
Figure 11 Narrow band imaging with magnification by endoscopy in patients with gastric ulcer shows fine vascular patterns, which may reflect precise quality of ulcer healing.
A: Conventional endoscopy; B: Magnifying endoscopy; C: Magnification + narrow band imaging.
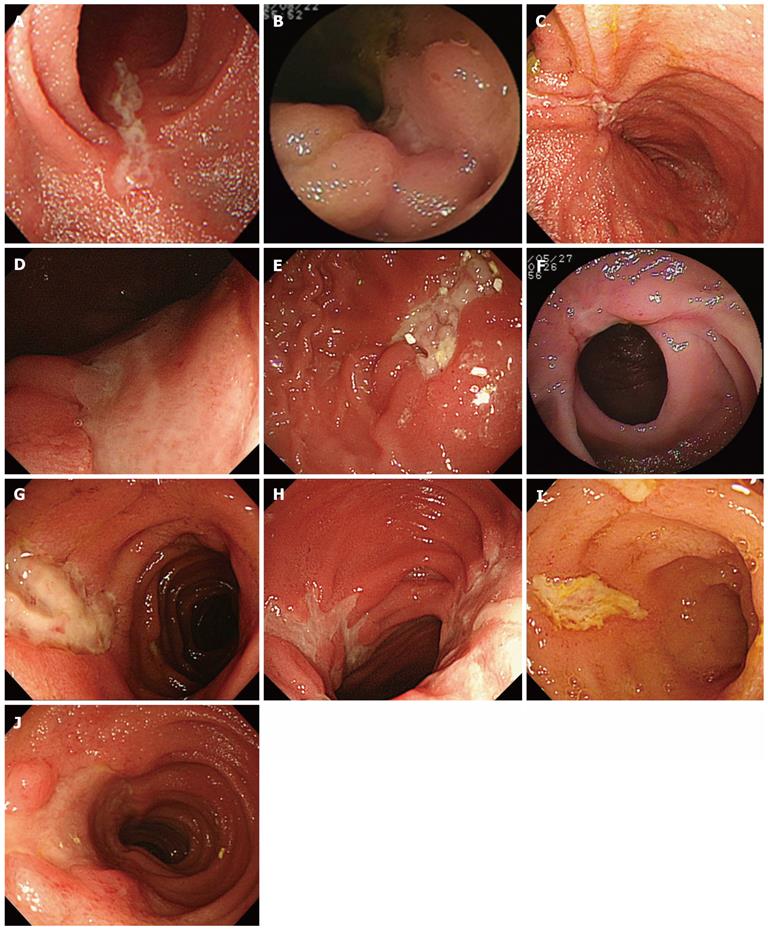
Figure 12 Morphological characteristics of active ulcer in patients with Crohn’s disease.
Shape of ulcer edge, flat (A) or non-flat (B); fold convergence, negative or positive (C); shape of ulcer base, flat (D) or non-flat (E); stenosis, negative or positive (F); neighboring ulcer, negative (G) or positive (H); width of ulcer, narrow (I) or wide (J).
- Citation: Arakawa T, Watanabe T, Tanigawa T, Tominaga K, Fujiwara Y, Morimoto K. Quality of ulcer healing in gastrointestinal tract: Its pathophysiology and clinical relevance. World J Gastroenterol 2012; 18(35): 4811-4822
- URL: https://www.wjgnet.com/1007-9327/full/v18/i35/4811.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i35.4811