Copyright
©2012 Baishideng Publishing Group Co.
World J Gastroenterol. Apr 21, 2012; 18(15): 1708-1722
Published online Apr 21, 2012. doi: 10.3748/wjg.v18.i15.1708
Published online Apr 21, 2012. doi: 10.3748/wjg.v18.i15.1708
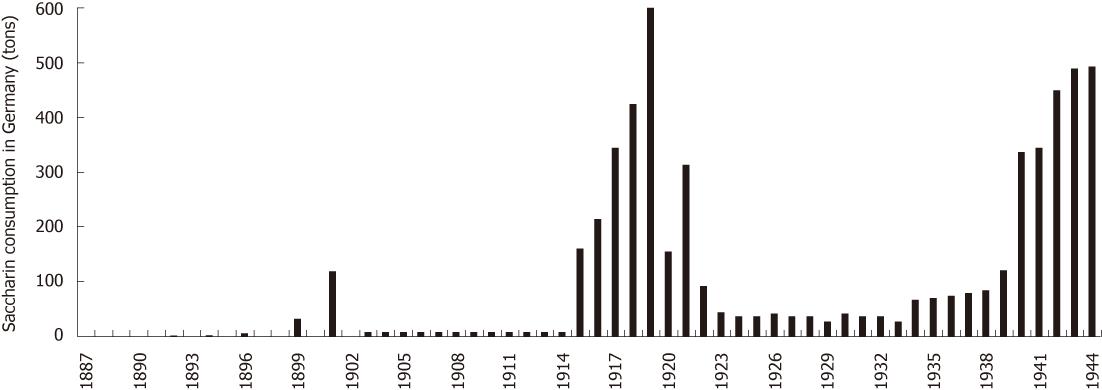
Figure 1 Saccharin consumption in Germany over time (1887-1944).
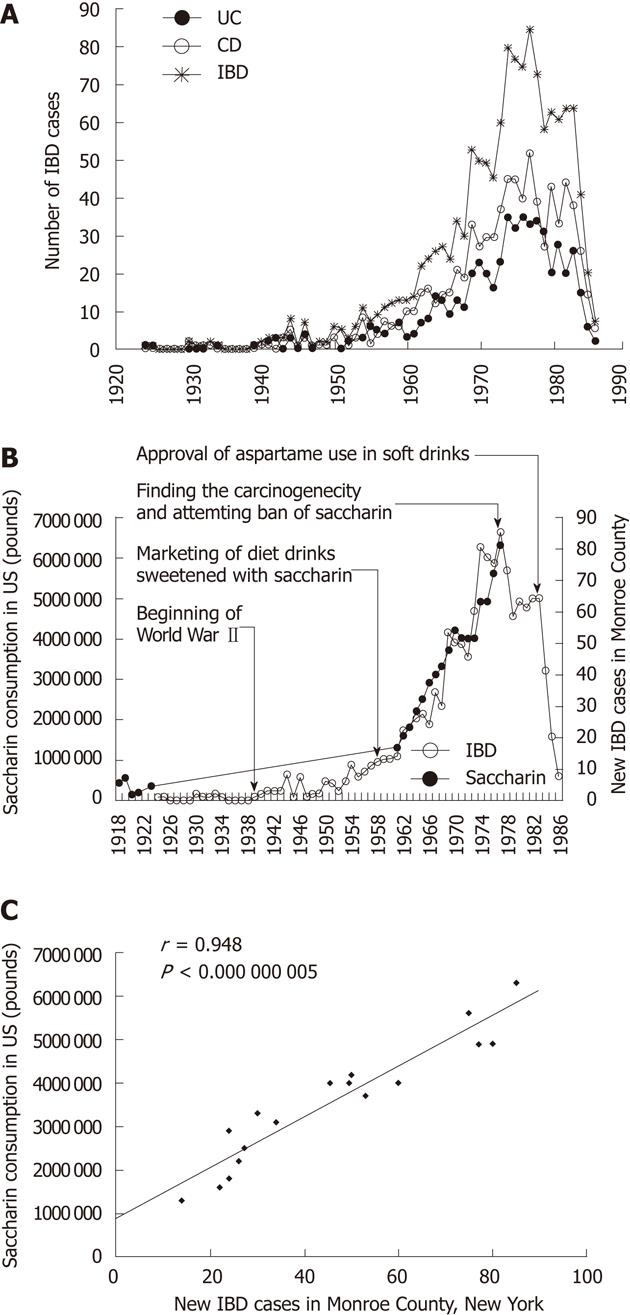
Figure 2 The dramatic increase in saccharin consumption since 1950s and the remarkable increase in inflammatory bowel disease during 1950s and 1970s in countries like the United States.
A: Occurrence of ulcerative colitis (UC), Crohn’s disease (CD), and inflammatory bowel disease [inflammatory bowel disease (IBD) = UC + CD] in Monroe County, New York during 1920s to 1980s; B: A comparison of the temporal change of IBD in Monroe County, New York and the saccharin consumption in the United States; C: Correlation between IBD in Monroe County, New York and the saccharin consumption in the United States.
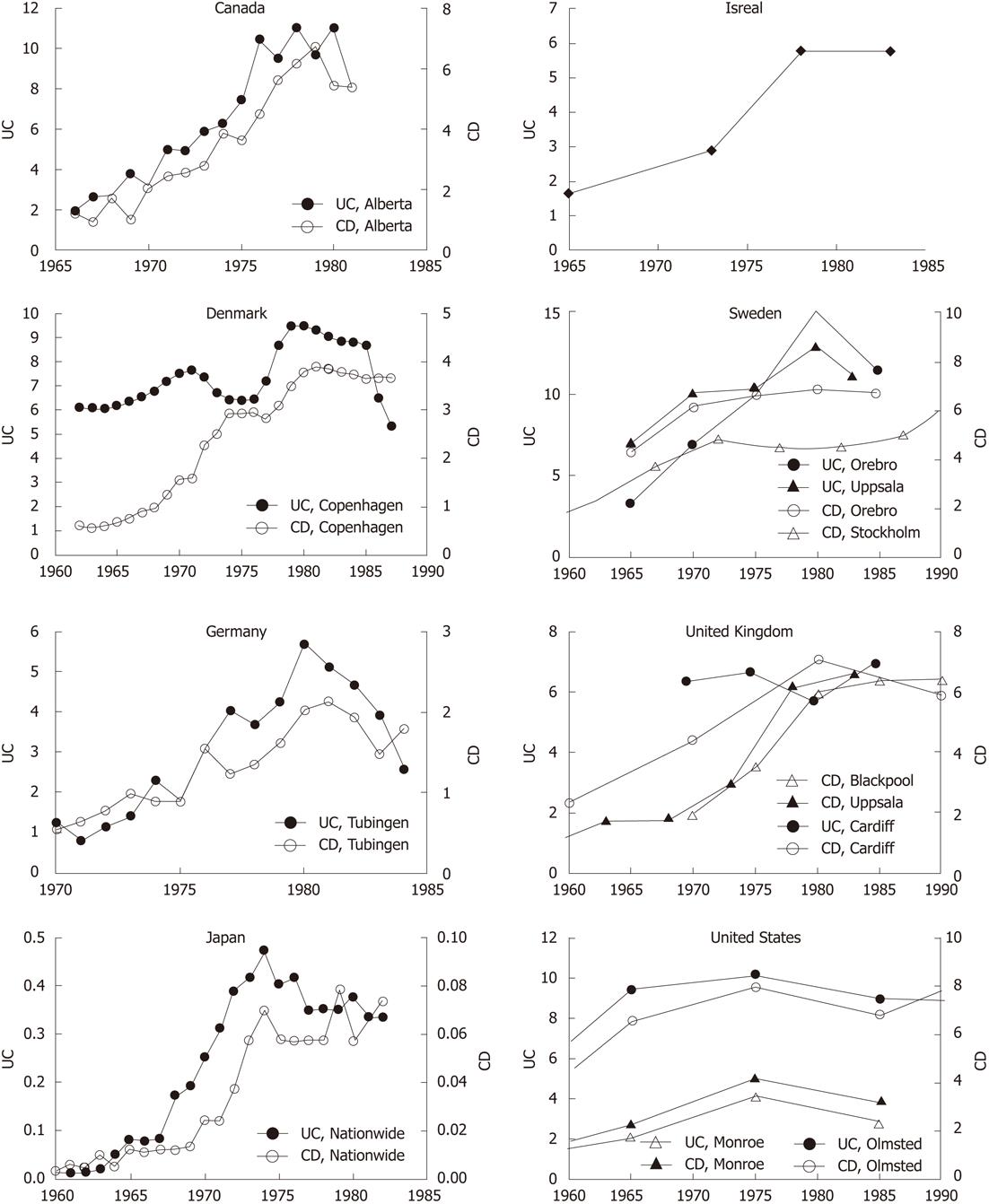
Figure 3 A leveling off or decrease of ulcerative colitis or Crohn’s disease during 1970s and 1980s in the different countries such as Canada, Demark, Germany, Japan, Israel, Sweden, United Kingdom, and United States.
UC: Ulcerative colitis; CD: Crohn’s disease.
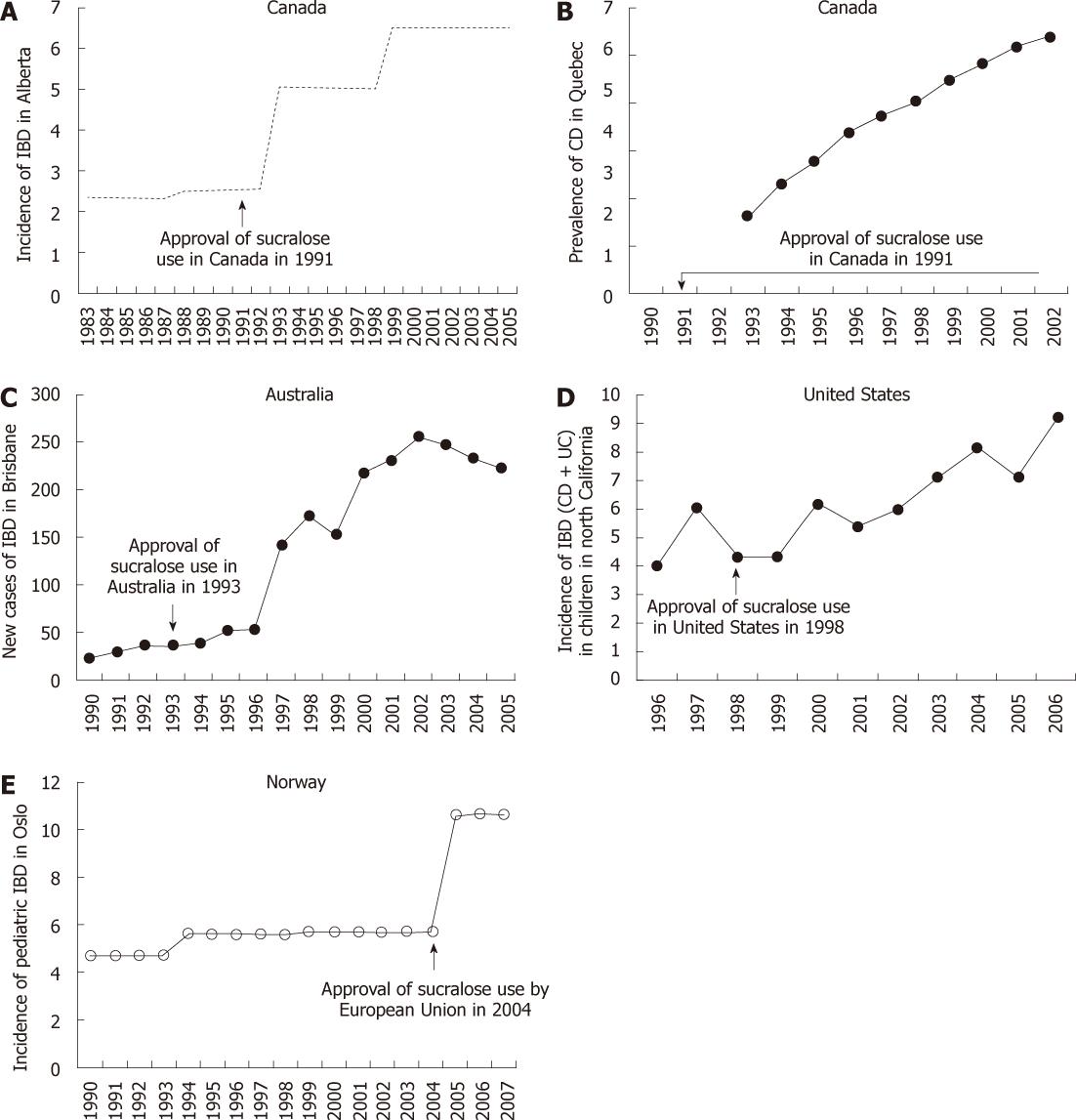
Figure 4 Relationship between the increase of inflammatory bowel disease and approval of sucralose in countries like Canada, Australia, United States and Norway.
IBD: Inflammatory bowel disease; UC: Ulcerative colitis; CD: Crohn’s disease.
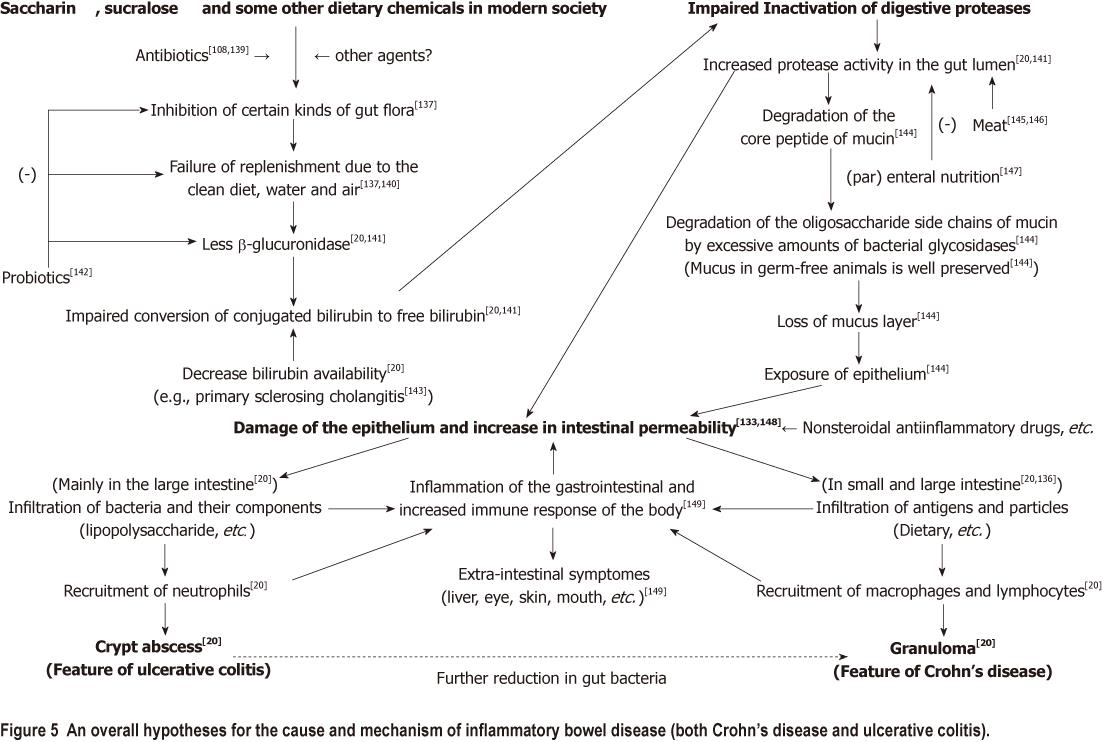
Figure 5 An overall hypotheses for the cause and mechanism of inflammatory bowel disease (both Crohn’s disease and ulcerative colitis).
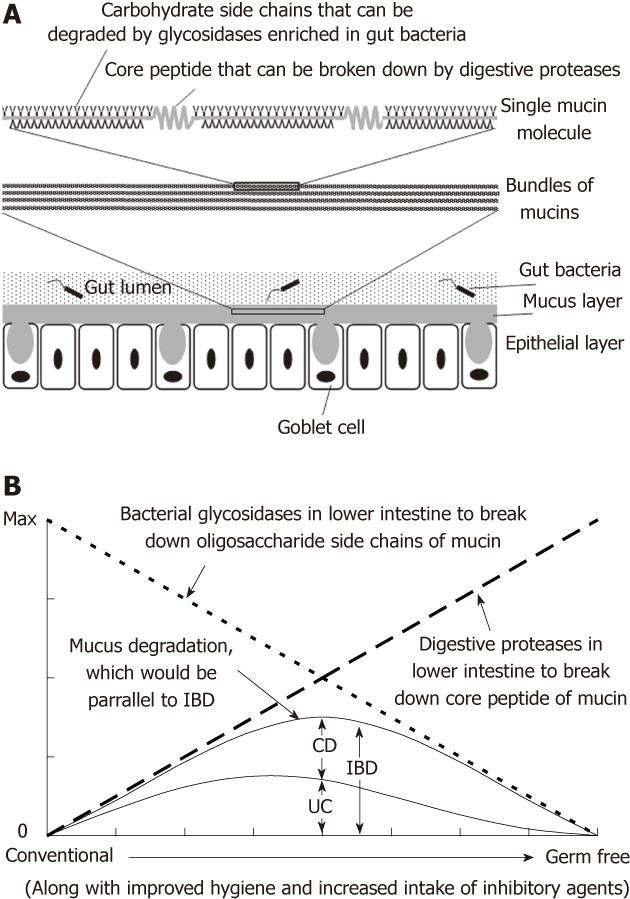
Figure 6 Ulcerative colitis and Crohn’s disease are likely just two symptoms of the same morbidity rather than two different diseases.
A: The structure of mucin; B: Mechanistic sketch of the temporal changes of ulcerative colitis (UC) and Crohn’s disease (CD) and their relationship. A reduction in gut bacteria along with the improved hygiene and increased intake of dietary chemicals like saccharin and sucralose will result in impairment in digestive proteases inactivation. The poorly inactivated proteases will work together with glycosidases from the gut bacteria to cause accelerated degradation of the mucus layer that is proposed here paralleling the risk of developing inflammatory bowel disease (IBD = UC + CD). UC and CD differ in that UC is caused by the increased infiltration of bacteria and the resultant recruitment of neutrophils and formation of crypt abscess, while CD is caused by increased infiltration of luminal antigens and particles and the resultant recruitment of macrophages and formation of granulomas. Thus the reduction in gut bacteria along with the modernization or other factors will result in a shift of predominance from the bacteria-meditated UC to antigen/particle-mediated CD. Max: maximum.
- Citation: Qin X. Etiology of inflammatory bowel disease: A unified hypothesis. World J Gastroenterol 2012; 18(15): 1708-1722
- URL: https://www.wjgnet.com/1007-9327/full/v18/i15/1708.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i15.1708