Copyright
©2010 Baishideng.
World J Gastroenterol. Jan 28, 2010; 16(4): 411-417
Published online Jan 28, 2010. doi: 10.3748/wjg.v16.i4.411
Published online Jan 28, 2010. doi: 10.3748/wjg.v16.i4.411
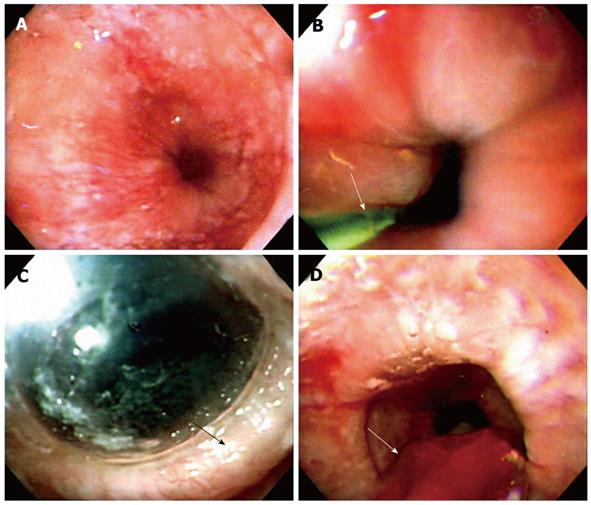
Figure 1 Technique of endoscope-guided pneumatic dilation (PD).
A: A dilated low esophageal lumen with tight gastroesophageal junction under endoscope-guided PD; B: The endoscope is inserted down to the duodenum. A guide-wire (arrow) is placed into the duodenum under endoscopic guidance and the endoscope is removed. A Regiflex balloon dilator, which is marked with a thick colored marker at the mid-section of the balloon, is passed over the guide wire to the stomach; C: The endoscope is reinserted to serve as a guide to control the position of the balloon in the esophagus. The balloon is withdrawn to the esophagus, until the mark reaches the gastroesophageal junction. The balloon is then inflated up to 12 psi and maintained for 60 s, until an ischemic ring (arrow) at the LES is seen by the endoscope through the transparent balloon; D: The balloon is flattened completely and removed together with the endoscope (arrow).
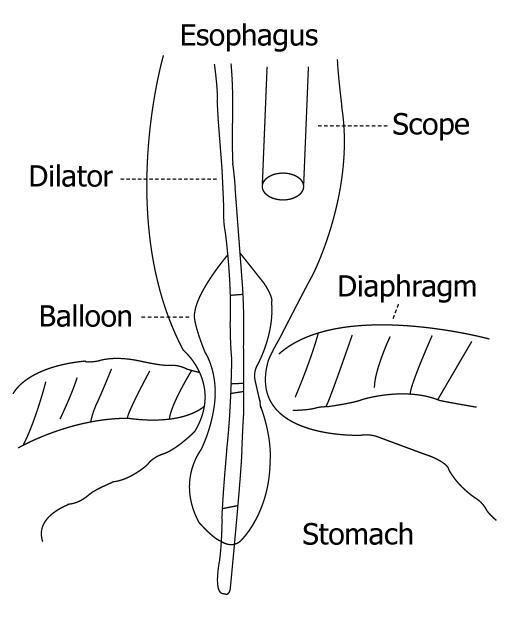
Figure 2 Almost all endoscope-guided PD are performed by using a low compliance Rigiflex balloon dilator by positioning the endoscope above the balloon without fluoroscopy.
The advantages are that the procedure can be performed without any extra equipment in a time and cost-effective manner.
- Citation: Chuah SK, Wu KL, Hu TH, Tai WC, Changchien CS. Endoscope-guided pneumatic dilation for treatment of esophageal achalasia. World J Gastroenterol 2010; 16(4): 411-417
- URL: https://www.wjgnet.com/1007-9327/full/v16/i4/411.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i4.411